
Medication Assisted Treatment: Compassionate, Evidence-Based Medication-Assisted Treatment Online
November 7, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
7-hydroxymitragynine, commonly known as 7-OH, is an alkaloid compound found naturally in kratom leaves. While kratom contains over 40 different alkaloids, this particular compound stands out as one of kratom's most potent, despite being present in relatively small concentrations—typically less than 2% within the plant's total alkaloid content. The specific 7-OH kratom effects are significantly more intense than those of the raw plant, creating a unique profile of risks and physiological responses.
What makes this alkaloid particularly significant is its powerful interaction with opioid receptors in the brain. Research indicates that this compound binds to these receptors with considerably greater affinity than mitragynine, kratom's primary alkaloid. This enhanced binding capacity translates to effects that can be substantially more intense than those produced by traditional kratom consumption.
The compound has gained attention in recent years as manufacturers have developed extraction and concentration methods to isolate it from kratom plant material. These concentrated products can contain alkaloid levels far exceeding what occurs naturally, creating preparations that are exponentially stronger than conventional kratom powder or tea.
"What was once a relatively obscure component within an already controversial botanical has become a standalone product marketed in various forms—from tablets and tinctures to vape liquids."
For individuals in recovery or those supporting someone navigating addiction challenges, recognizing this alkaloid as distinct from kratom itself is essential. The concentrated nature these products introduce involves different considerations around tolerance, dependence, and withdrawal. As the compound continues to appear in convenience stores, online marketplaces, and specialty shops throughout New England and beyond, awareness about what it is—and why it differs from its source plant—has become increasingly important for making informed decisions about use and recovery.
Decision Tool: Spotting the Difference
Traditional kratom leaf contains a wide array of natural alkaloids, with 7-hydroxymitragynine (7-OH) present only in trace amounts—typically less than 0.02%2. In contrast, many modern products are engineered to dramatically increase 7-OH levels, resulting in effects that mimic prescription opioids rather than the milder, traditional kratom experience1.
| Feature | Traditional Kratom Leaf | Concentrated 7-OH Products |
|---|---|---|
| Form | Loose leaf, powder, tea | Gummies, vapes, liquid shots, tablets |
| 7-OH Content | Trace amounts (<0.02%) | Highly concentrated/Synthetic |
| Risk Profile | Lower potency | High overdose & addiction potential |
Both addiction risk and overdose potential are much higher with concentrated 7-OH than with plant-based kratom, a distinction highlighted by recent FDA warnings about mislabeled products1.
Quick Assessment: Is Your Product Naturally-Derived or Synthetic?
Naturally, 7-hydroxymitragynine (7-OH) exists in kratom leaves at trace levels. Most traditional kratom products deliver only these minimal amounts. In comparison, synthetic or concentrated 7-OH products are engineered to dramatically amplify this alkaloid, creating powerful opioid-like effects that are not found in nature2. Increased reports of adverse outcomes are closely tied to synthetic 7-OH, not traditional kratom leaf1.
When comparing 7-OH kratom effects to traditional kratom, the difference in strength is dramatic. While traditional leaf is mild and slow-acting, concentrated 7-OH can deliver effects rivaling prescription opioids.
Studies reveal that even small doses of synthesized 7-OH can trigger intense euphoria, sedation, and respiratory depression—outcomes rarely observed with plain kratom powder1. This approach is ideal for anyone weighing the safety of traditional kratom versus newer extracts: the leap in potency is not just a minor difference, but a major shift in both effect and risk profile.
Regulatory Action Checklist: Are You Impacted by New 7-OH Laws?
The landscape for 7-OH kratom effects is rapidly changing as lawmakers and agencies respond to mounting public health concerns. In 2025, the FDA formally recommended that 7-OH be scheduled as a controlled substance, distinguishing it from traditional kratom leaf and targeting concentrated forms sold in convenience outlets1. State-level actions—especially in the Northeast—include bans on gas station sales and new labeling rules for kratom extracts.
In 2025, the FDA issued a formal recommendation to schedule 7-OH as a controlled substance, separating it from traditional kratom leaf and focusing on concentrated, synthetic, or extract products1. This move reflects mounting evidence that 7-OH kratom effects—especially in vapes, gummies, and flavored edibles—are far more potent and carry opioid-like risks including overdose, addiction, and respiratory depression1.
States in the Northeast, such as Vermont and Massachusetts, have begun aligning with the FDA by passing laws that ban the sale of 7-OH products in gas stations and impose strict penalties for unlicensed distribution, while still permitting traditional kratom leaf sales under new labeling requirements.
Gas station and convenience store 7-OH products present a higher risk because they often feature concentrated or synthetic forms, are poorly labeled, and can be marketed to youth as appealing edibles or vapes1. These environments lack consistent oversight, so products may contain unexpectedly high doses or impurities, increasing the severity of 7-OH kratom effects and the likelihood of overdose or adverse reactions. Industry leaders note a spike in emergency cases tied to these outlets, as consumers may not realize they are buying opioid-strength substances1.
7-hydroxymitragynine interacts with the brain's opioid receptors, the same neural pathways activated by prescription painkillers and illicit opioids. When someone uses this compound, it binds primarily to mu-opioid receptors throughout the central nervous system, triggering the release of dopamine and creating feelings of euphoria and pain relief.
What makes this alkaloid particularly concerning is its potency. Preliminary research suggests it may be up to 10 times more potent than morphine in activating these receptors. While this doesn't necessarily mean the effects are ten times stronger in practice—potency depends on dosage, individual tolerance, and other factors—it does indicate that relatively small amounts can produce significant effects on brain chemistry. This intense binding affinity potentially leads to rapid tolerance development as the brain adjusts to repeated exposure.
The compound also influences other neurotransmitter systems beyond the opioid pathway. Some studies indicate it affects serotonin and norepinephrine levels, which help regulate mood, sleep, and stress responses. This multi-system impact explains why people using this kratom derivative may experience a wide range of psychological effects, from initial mood elevation to eventual dysregulation when not taking the substance.
Over time, regular use alters the brain's natural reward circuitry. The brain begins to rely on external sources of opioid receptor stimulation rather than producing its own endorphins. This neurochemical adaptation creates a cycle where normal activities that once brought pleasure feel less rewarding, while cravings for the alkaloid intensify.
Receptor Activation Checklist: Are You at Risk of Opioid-Like Brain Effects?
When 7-OH enters the brain, it binds powerfully to mu, delta, and kappa opioid receptors—the same pathways targeted by prescription opioids4. This strong opioid receptor binding is what makes 7-OH kratom effects so intense, leading not only to pain relief and euphoria but also to serious risks like respiratory depression and altered neural signaling4. Studies reveal that concentrated 7-OH can change the way the brain processes reward and motivation, increasing susceptibility to dependence and neurotoxicity3.
When 7-OH enters the brain, it binds with remarkable strength to mu, delta, and kappa opioid receptors—key sites responsible for regulating pain, mood, and consciousness.
The mu receptor is most closely tied to the powerful euphoria and high addiction potential seen with 7-OH kratom effects, while delta receptors are linked to mood fluctuation and may drive emotional instability at higher doses. Kappa receptor activation can cause sedation or even feelings of disconnection from reality, especially in concentrated products4.
After 7-OH enters the system and binds to opioid receptors, the body converts a portion of it into mitragynine pseudoindoxyl (MP)—a process that further intensifies the clinical impact of 7-OH kratom effects. MP is recognized for its nearly fentanyl-level potency and can amplify both the duration and strength of opioid-like outcomes such as euphoria, sedation, and respiratory depression2. Research shows that the conversion to MP is a key reason why concentrated 7-OH products may be far more hazardous than traditional kratom, sometimes outlasting initial effects and increasing risk for overdose and dependency2.
Cognitive Health Checklist: Are You Noticing These Changes?
7-OH kratom effects extend well beyond pain relief or sedation—they can significantly disrupt cognition and overall neurological health. Research indicates that high doses of 7-OH, especially in concentrated or synthetic products, have been linked to memory problems, confusion, and episodes of disorientation3. For some, even at lower doses, there may be subtle effects on attention and clarity, while higher doses raise the likelihood of pronounced neurotoxic outcomes.
Studies reveal that 7-OH kratom effects are highly dose-dependent. At low exposures, some kratom alkaloids have shown antioxidant and neuroprotective properties through pathways like Keap1-Nrf2 activation. However, as the dose increases, especially with concentrated or synthetic 7-OH, the risk shifts sharply toward neurotoxicity, including oxidative stress, synapse loss, and nerve cell death3. Recognizing where you are on this spectrum is key to avoiding long-term neurological harm.
Breakthrough seizures are a documented complication of high-dose 7-OH kratom effects, especially among individuals with a personal or family history of epilepsy7. Clinical reports show that seizures can occur even in people without prior neurological issues, with rates ranging from 6% to 17.5% in kratom-only exposures7. The risk appears highest when using concentrated, synthetic, or adulterated forms, which can disrupt normal brain signaling and lower the seizure threshold.
The physical toll of 7-hydroxymitragynine use extends beyond the immediate euphoric effects, with individuals often experiencing a cascade of concerning symptoms that worsen over time. Understanding these warning signs can help people recognize when recreational use has crossed into dangerous territory.
Gastrointestinal distress ranks among the most common complaints, with many people experiencing severe constipation, nausea, and stomach cramping. These digestive issues can become chronic, significantly impacting daily functioning and nutritional intake. The compound's interaction with opioid receptors in the gut disrupts normal digestive processes, sometimes leading to conditions that require medical intervention.
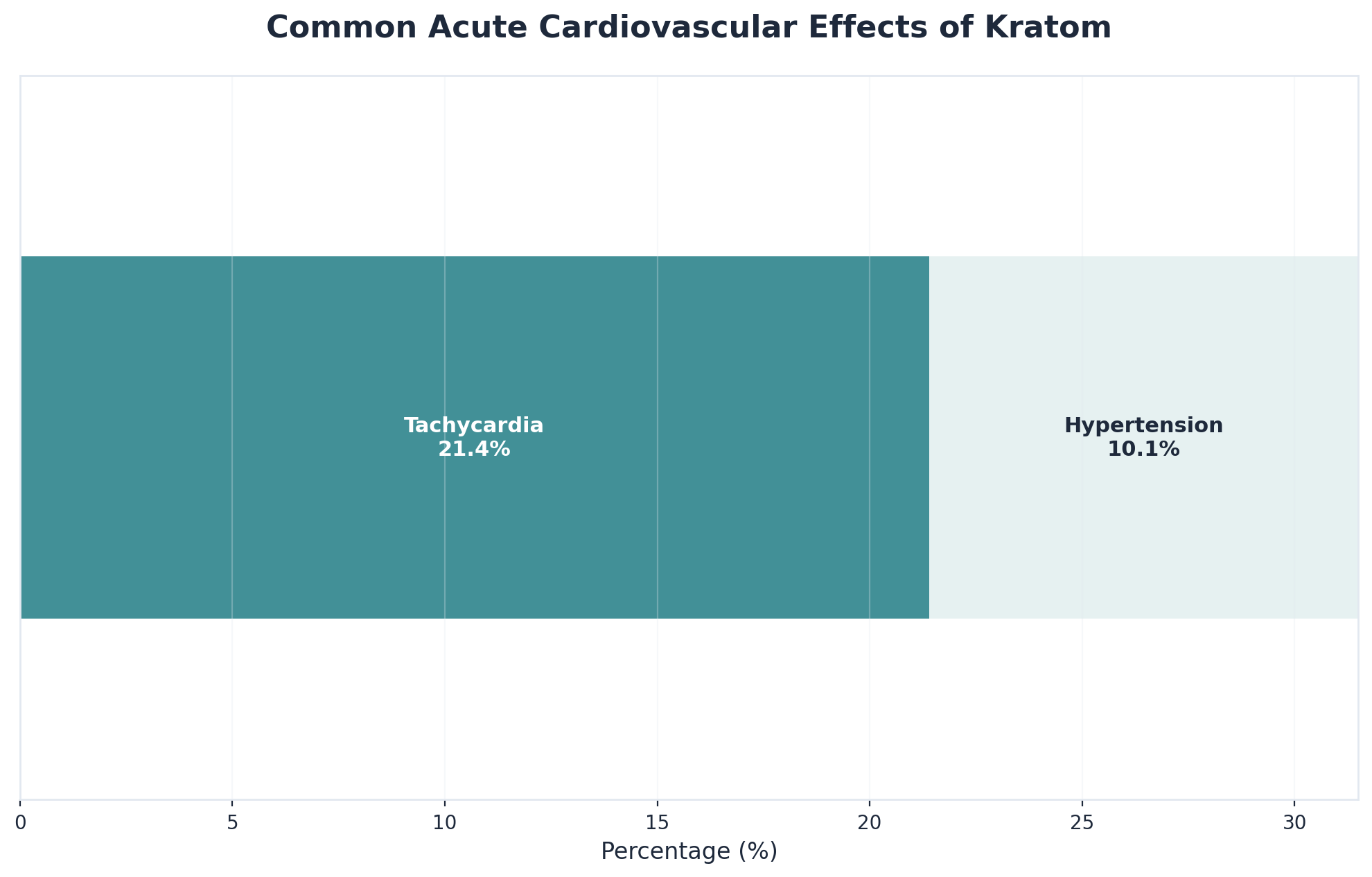
Cardiovascular symptoms present another serious concern. Individuals frequently report rapid heartbeat, elevated blood pressure, and chest discomfort. Some have experienced more severe cardiac events, particularly when combining this potent alkaloid with other substances or using higher doses. The strain on the cardiovascular system accumulates with continued use, potentially causing lasting damage.
Neurological effects manifest through persistent headaches, dizziness, and cognitive fog that lingers even between doses. Many people describe difficulty concentrating, memory problems, and a general sense of mental sluggishness that interferes with work and personal responsibilities. Sleep disturbances are equally prevalent, with individuals cycling between insomnia and excessive drowsiness.
Physical dependence develops quickly, often catching people off guard. Early warning signs include needing the substance to feel normal, experiencing discomfort when doses are delayed, and requiring increasingly larger amounts to achieve desired effects. The body adapts to the compound's presence, making cessation progressively more difficult without professional support.
Complication Checklist: Are You at Risk for Heart or Lung Emergencies?
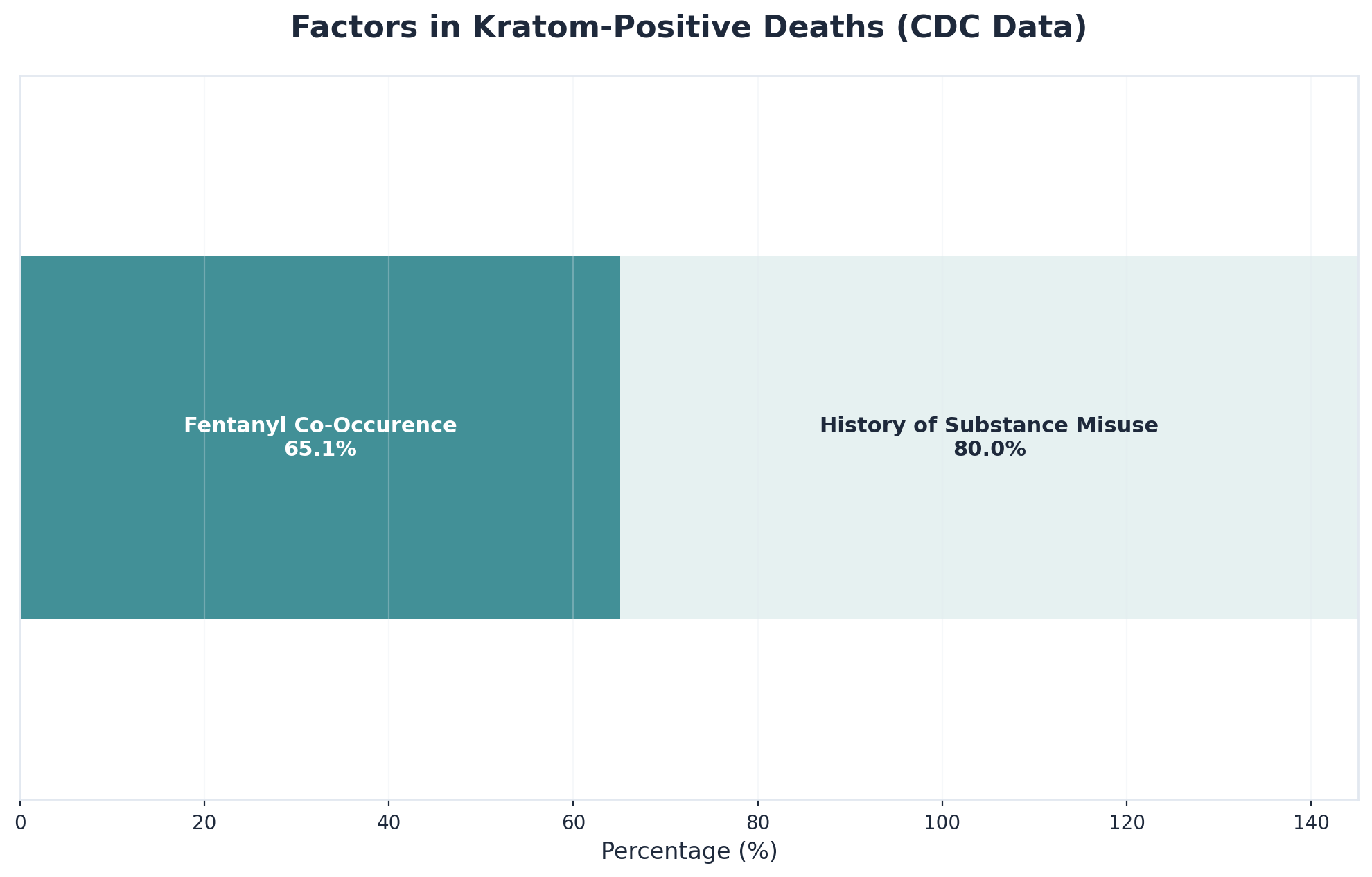
Cardiovascular and respiratory complications are among the most serious 7-OH kratom effects. National poison data show that tachycardia (rapid heartbeat) occurs in over 21% of kratom exposures, and hypertension (elevated blood pressure) in about 10%5. Concentrated 7-OH can also cause life-threatening respiratory depression, mirroring the dangers seen with prescription opioid overdoses1.
Cardiac complications are among the most frequently reported 7-OH kratom effects, especially with concentrated or synthetic extracts. National poison control data show that tachycardia—an abnormally rapid heartbeat—occurs in over 21% of kratom exposures, while hypertension (elevated blood pressure) is seen in about 10%5. These cardiovascular events can escalate to more serious issues like arrhythmias or, in rare cases, even heart attack, particularly in people with underlying risk factors.
Respiratory depression—meaning dangerously slowed or shallow breathing—is a hallmark of severe 7-OH kratom effects, particularly with concentrated or synthetic products. Research shows that these opioid-like compounds can suppress the brain’s respiratory centers, creating a risk profile similar to prescription opioid overdose1. Emergency departments have reported cases where individuals required immediate intervention due to life-threatening respiratory suppression following 7-OH exposure.
Liver & Organ Health Checklist: Are You Noticing These Red Flags?
When it comes to 7-OH kratom effects, liver toxicity is a major concern—especially with concentrated or synthetic forms. Medical case series have documented drug-induced liver injury (DILI) linked to kratom products, often showing a cholestatic pattern, which means bile flow is impaired and harmful substances can build up in the body6. Symptoms can appear within just a few weeks of use, with some cases requiring hospital care.
Clinical reports reveal that 7-OH kratom effects can trigger drug-induced liver injury (DILI) with a cholestatic or mixed injury pattern, meaning bile flow from the liver becomes blocked or impaired6. In recent case series, most individuals developed symptoms within about three weeks of using kratom extracts or synthetic 7-OH—often presenting with jaundice, abdominal pain, and abnormal liver enzymes6.
For those using concentrated or synthetic 7-OH kratom, recognizing physical warning signs is essential. Symptoms like jaundice, abdominal pain, and abnormal urine color often signal liver toxicity or broader organ damage, especially when 7-OH kratom effects are involved6. Medical case series reveal that drug-induced liver injury (DILI) can start within just a few weeks of use, and prompt attention can make a major difference.
7-Hydroxymitragynine dependence develops through neurological adaptation as the brain's opioid receptors become increasingly reliant on the compound's effects. As a partial opioid agonist, 7-OH creates tolerance similar to traditional opioids—individuals often find themselves using larger amounts more frequently to achieve the same pain relief or euphoric sensation. This escalation can occur within weeks of regular use, particularly given the compound's high potency at mu-opioid receptors.
Withdrawal from 7-OH follows patterns consistent with opioid-like substances rather than stimulants. Physical symptoms typically include muscle aches, restlessness, sweating, dilated pupils, and gastrointestinal distress including nausea and diarrhea. Psychological effects manifest as anxiety, irritability, insomnia, and dysphoria. These symptoms generally emerge within 12-24 hours of last use, peak around days 2-4, and gradually subside over 7-10 days, though psychological symptoms may persist longer.
The physical discomfort and psychological distress that emerge during early recovery can feel overwhelming, which is why professional support becomes essential. Evidence-based treatment approaches for opioid-like dependence combine medication-assisted treatment options with behavioral therapies such as cognitive-behavioral therapy and contingency management. For those managing co-occurring mental health conditions alongside their 7-OH dependency, integrated treatment addresses both challenges simultaneously rather than treating them as separate issues.
Recovery pathways vary considerably based on individual circumstances, severity of dependence, and available support systems. Some people benefit from intensive outpatient programs that provide structure while allowing them to maintain work and family responsibilities. Others may require medically-supervised detoxification initially, particularly for heavy use. The key is finding a treatment approach that addresses the whole person—not just the addiction—and provides the tools necessary for sustained recovery. Virtual treatment options have expanded access considerably, allowing individuals to receive evidence-based care regardless of geographic location.
Substance Use Disorder Self-Assessment: Are You at Risk?
Understanding 7-OH substance use disorder begins with recognizing how 7-OH kratom effects fuel rapid and persistent dependency. Unlike traditional kratom, concentrated or synthetic 7-OH products act as full opioid agonists, binding to brain receptors in ways that mirror prescription opioid addiction9. This interaction can drive compulsive use, powerful cravings, and a cycle of withdrawal and relapse that is difficult to break without support.
The abuse potential of 7-OH is driven by its action as a full opioid agonist, binding powerfully to the brain’s mu opioid receptors—much like prescription painkillers or heroin. This interaction explains why 7-OH kratom effects are so much more reinforcing and habit-forming than those of traditional kratom leaf9. Research shows that repeated use of concentrated or synthetic 7-OH rapidly builds tolerance, causing individuals to escalate their dose and deepen dependency.
Withdrawal from concentrated or synthetic 7-OH kratom effects can follow a pattern that is less physically intense than classic opioid withdrawal but may last much longer.
Clinical evidence shows that symptoms such as insomnia, anxiety, and muscle pain often persist for a week or more, with some individuals experiencing a drawn-out period of low mood and poor focus that extends beyond the acute phase10.
Decision Guide: Should You Seek Treatment for 7-OH Use?
Deciding when to seek treatment for 7-OH kratom effects can be challenging, especially as withdrawal and dependency patterns often develop quickly with concentrated products9. If physical withdrawal has become disruptive, or if you’re experiencing medical complications like seizures or respiratory problems, prioritizing treatment becomes urgent9.
A structured severity assessment helps clarify when 7-OH kratom effects have crossed into substance use disorder territory. Research shows that rapid escalation, withdrawal, and health impacts signal higher addiction severity and urgent need for intervention9.
Implementation of a recovery plan for 7-OH kratom effects depends on withdrawal severity, health risks, and personal circumstances.

Outpatient virtual care works well for those with mild to moderate symptoms and strong home support, offering flexibility and privacy through telehealth programs available in Vermont, Massachusetts, Connecticut, and New Hampshire. For individuals facing more pronounced cravings, repeated relapse, or co-occurring health conditions, a combination of virtual medical management and regular monitoring is recommended9.
Understanding this concentrated alkaloid and recovery options often raises important questions. Here are answers to some common concerns people have when considering treatment.
Stopping 7-OH products on your own is possible for some, but medical supervision is highly recommended—especially if you’re using concentrated or synthetic forms, have a history of seizures, or notice severe withdrawal symptoms. 7-OH kratom effects are significantly stronger than traditional kratom, and withdrawal can bring anxiety, insomnia, muscle aches, or even breakthrough seizures in vulnerable individuals79. This solution fits people with mild symptoms and strong support at home, but if you experience complications like confusion, chest pain, trouble breathing, or intense cravings, prioritize medical oversight—virtual or in-person. Virtual treatment options in Vermont, Massachusetts, Connecticut, and New Hampshire can provide safe, flexible monitoring for most people in recovery.
To tell if you’re using traditional kratom or concentrated 7-OH, start by checking the product label—traditional kratom is usually sold as loose leaf, powder, or capsules and does not list "7-hydroxymitragynine" or "7-OH" as a main ingredient. In contrast, concentrated 7-OH products are often labeled as "extracts," "enhanced," or specifically mention 7-OH, and are sold as gummies, vapes, or flavored edibles. Traditional kratom contains less than 0.02% 7-OH, while extracts and synthetics can have much higher, opioid-like potency, greatly increasing the risks associated with 7-OH kratom effects12.
Most major health insurers now cover virtual treatment for substance use disorder (SUD), including support for those experiencing 7-OH kratom effects, especially in states like Vermont, Massachusetts, Connecticut, and New Hampshire. Coverage may vary depending on your specific plan, but telehealth-based SUD treatment is increasingly recognized as medically necessary by both private and government insurers9.
Withdrawal from 7-OH kratom effects usually lasts longer but is less physically severe than withdrawal from prescription opioids. While classic opioid withdrawal symptoms (such as nausea, cramps, and chills) often peak within 2–4 days and mostly resolve in a week, 7-OH withdrawal can stretch out with lingering symptoms like insomnia, anxiety, and low mood that persist for 10 days or more in some cases10.
Yes, many people are able to continue working—often with minimal disruption—while receiving treatment for 7-OH use, especially when choosing virtual care options. Virtual substance use disorder programs for 7-OH kratom effects are tailored for busy professionals, offering flexible scheduling, after-hours sessions, and privacy safeguards so you can attend appointments outside of work hours or during breaks9.
At-home detox is self-managed in your own environment and fits people experiencing only mild symptoms, who have reliable support at home and no serious health risks. Ambulatory (outpatient) withdrawal support offers scheduled virtual or in-person sessions with clinical supervision—ideal if withdrawal is moderate, symptoms are unpredictable, or you have a history of seizures or medical complications. This approach uses regular check-ins, medical monitoring, and sometimes medication assistance to reduce risks linked to concentrated kratom extract use9.
Yes, there are medications that can help ease withdrawal symptoms from 7-OH kratom effects, especially when symptoms are moderate to severe. While the FDA has not approved a specific medication for 7-OH withdrawal, clinicians often use medicines developed for opioid withdrawal—such as buprenorphine for craving and stabilization, or clonidine to reduce anxiety, sweating, and agitation9.
The cost of virtual treatment for 7-OH kratom effects can vary widely based on insurance coverage, program intensity, and specific services offered. While some individuals may pay only a standard specialist copay with insurance, others might face out-of-pocket costs for sessions if coverage is limited—especially for telehealth-based substance use disorder care9. Many virtual programs in Vermont, Massachusetts, Connecticut, and New Hampshire will verify your insurance and discuss any expected costs before you begin.
If you’ve experienced relapse after previous treatment, a virtual program can still be highly effective—especially for individuals facing ongoing challenges with 7-OH kratom effects. Virtual substance use disorder care offers flexible scheduling, regular check-ins, and rapid access to professional support, which studies show can improve engagement and reduce the risk of future relapse9.
Pathfinder currently offers virtual support for individuals in Vermont, Massachusetts, Connecticut, and New Hampshire who are seeking help with 7-OH kratom effects. If you reside in one of these states, you can access specialized substance use disorder (SUD) treatment that also addresses co-occurring mental health needs, all through confidential telehealth sessions. Pathfinder does not provide primary mental healthcare but does offer co-occurring support alongside SUD services.
Experiencing anxiety or depression alongside 7-OH kratom effects is common, as these potent extracts can disrupt mood-regulating brain chemistry and intensify emotional symptoms49. Virtual treatment programs in Vermont, Massachusetts, Connecticut, and New Hampshire are designed to address both substance use disorder and co-occurring mental health needs, so you can receive support for anxiety or depression while managing withdrawal or dependency.
Virtual treatment for 7-OH kratom effects is highly private, with strict federal and state laws protecting your health information. Telehealth providers use secure platforms that keep your treatment details confidential—sessions are not shared with employers or family without your explicit written consent. Insurance billing for substance use disorder or co-occurring mental health support is also protected by HIPAA, so claims do not reveal specific diagnoses to non-medical parties.
If you experience seizures or any cardiac symptoms (such as chest pain, rapid heartbeat, or fainting) while using 7-OH products, seek emergency medical help right away. 7-OH kratom effects are linked to both breakthrough seizures—even in people without a prior history—and serious cardiovascular events like tachycardia and hypertension, which can escalate quickly to life-threatening situations57.
Starting a conversation with an adult child who is resistant to help for 7-OH use can feel daunting, but a supportive, non-judgmental approach is most effective. Begin by expressing concern about specific behaviors or symptoms you've noticed, using "I" statements. Avoid ultimatums or lectures, and instead offer information about the real risks of 7-OH kratom effects—such as the potential for dependency, withdrawal, or health complications9. Sharing that virtual support and confidential care are available in Vermont, Massachusetts, Connecticut, and New Hampshire may reduce stigma or fear about seeking help.
7-Hydroxymitragynine represents a significant development in the kratom landscape—a concentrated alkaloid that's considerably more potent than traditional kratom products. While marketed as a natural supplement, this compound interacts with opioid receptors in ways that can lead to physical dependence, withdrawal symptoms, and patterns of use that interfere with daily life.
Recognizing the signs of dependency matters. When someone finds themselves needing increasing amounts to achieve the same effects, experiencing uncomfortable symptoms when they try to cut back, or continuing use despite negative consequences, these patterns indicate that professional support may be beneficial. The withdrawal process from 7-OH can be challenging to navigate alone, with symptoms that range from physical discomfort to psychological distress.
The encouraging reality is that recovery from 7-hydroxymitragynine dependence is entirely possible with appropriate support. Treatment approaches that address both the physical aspects of withdrawal and any underlying factors contributing to use have helped many people successfully transition away from reliance on this compound. Modern treatment options have evolved to be more accessible than ever—including virtual care platforms that connect individuals with licensed addiction specialists without requiring travel to distant facilities or disruption to work and family commitments.
Comprehensive care addresses the full picture: managing withdrawal symptoms, developing healthier coping strategies, and addressing co-occurring concerns that may have contributed to problematic use. Whether through in-person services or telehealth options that provide video sessions and medication management when appropriate, quality treatment can fit into daily life while supporting long-term success.
For anyone recognizing that their relationship with this alkaloid has become problematic, taking action represents the most important step. Recovery doesn't require sacrificing privacy, employment, or daily responsibilities—it simply requires acknowledging the need for support and reaching out for professional guidance. With evidence-based treatment and the right resources, building a healthier life free from dependence on 7-hydroxymitragynine is an achievable goal worth pursuing.

November 7, 2025

November 7, 2025

November 6, 2025