
Substance Abuse Counseling: Accessible, Stigma-Free Therapy from Home with Pathfinder Recovery
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Neurodivergence encompasses a range of neurological differences, including autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), dyslexia, and other variations in how the brain processes information. Navigating addiction recovery for neurodivergent adults requires understanding that these individuals face significantly higher rates of addiction compared to the general population.
Studies indicate that adults with ADHD are approximately twice as likely to develop dependencies on alcohol or drugs, while autistic individuals also show elevated rates of addiction. The relationship between neurodivergence and addiction is complex and multifaceted. Many neurodivergent individuals turn to substances as a form of self-medication, seeking relief from sensory overwhelm, social anxiety, challenges with planning and organization, or the constant demands of navigating a neurotypical world.
"Substances may temporarily ease the exhaustion of masking—the practice of suppressing natural neurodivergent traits to fit societal expectations—or provide a sense of calm in an overstimulating environment."
Traditional addiction treatment programs often fail to recognize these unique underlying factors, focusing solely on chemical dependency without addressing the neurological differences that may contribute to it. This gap in understanding can lead to ineffective treatment approaches and higher relapse rates among neurodivergent individuals. Recognizing the intersection of neurodivergence and addiction is essential for developing effective, compassionate treatment strategies that address the whole person.
What You’ll Learn: This section explains the factors behind the higher risk of substance use disorder among neurodivergent adults. You’ll know you’ve learned it when you can identify at least three reasons why neurodivergent traits contribute to increased vulnerability.
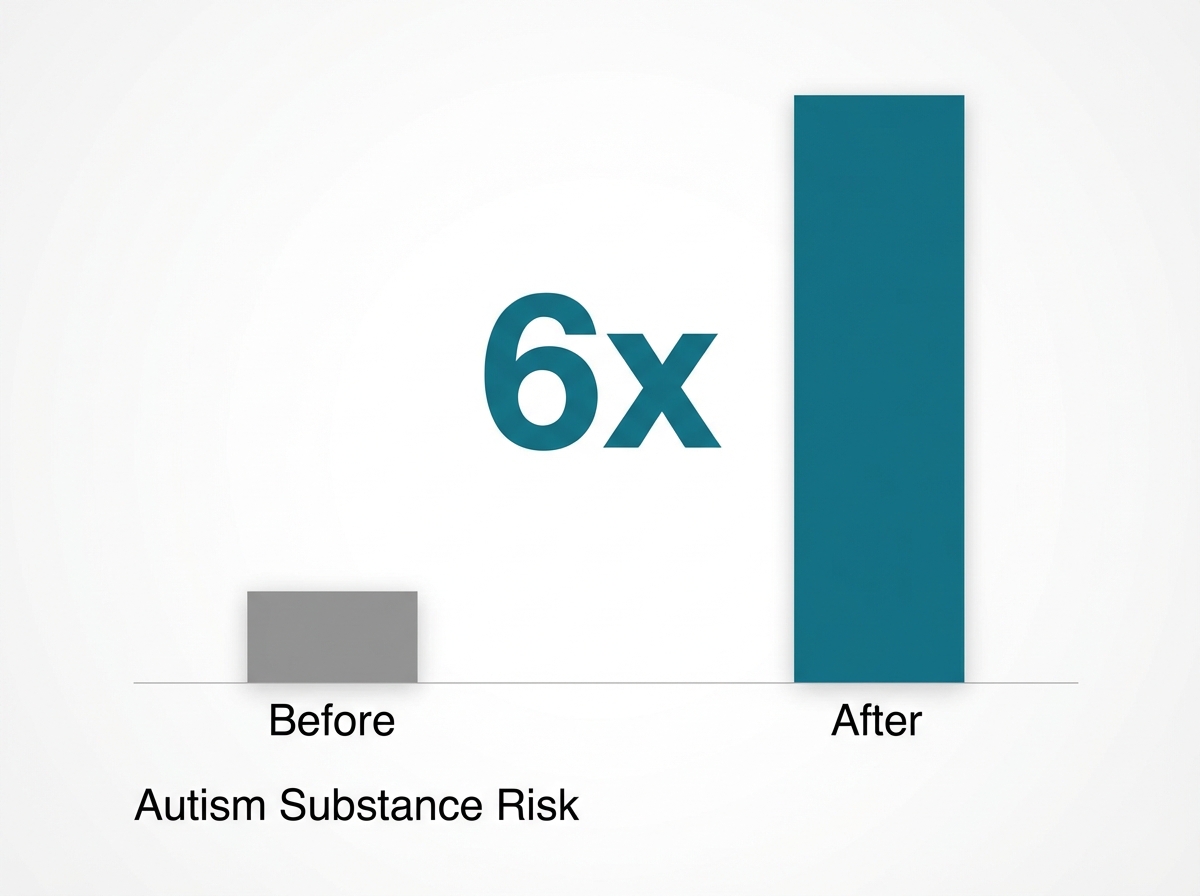
Neurodivergent adults—including those with autism or ADHD—are statistically far more likely to develop substance use challenges compared to neurotypical peers. Researchers have found that autistic individuals face a sixfold increase in risk for substance use disorder, while people with ADHD or behavioral differences also see elevated rates7. Several factors drive this vulnerability:
Practice This: Create a short paragraph describing how one neurodivergent trait (such as impulsivity or social anxiety) might influence substance use risk.
Skill Checkpoint: You’re ready for the next level when you can list three specific reasons neurodivergent adults have an increased risk of developing substance use disorder.
What You’ll Learn: This section unpacks how sensory processing differences shape substance use patterns in neurodivergent adults, and why self-medication often becomes a coping tool.
Many neurodivergent adults—particularly those with autism or sensory processing disorder—experience the world through a heightened or muted sensory lens. Imagine sitting in a crowded room where every sound is painfully loud, or where bright lights feel overwhelming. For some, these sensory challenges can make day-to-day life exhausting.
Studies reveal that autistic adults with pronounced sensory processing difficulties are more likely to use substances like alcohol as a way to dull overwhelming input or, in some cases, to seek out stimulation when feeling under-stimulated7.
Practice This: Write a short reflection on how a specific sensory experience (like discomfort with loud noises) might lead someone to use substances to cope.
Skill Checkpoint: You’re ready for the next level when you can explain how sensory processing issues might drive self-medication behaviors in addiction recovery for neurodivergent adults.
Traditional addiction treatment models often rely on approaches that can inadvertently create barriers for neurodivergent individuals. Neurodiversity-affirming care recognizes that different neurotypes require tailored strategies that work with, instead of against, natural cognitive patterns.
This approach begins with comprehensive assessment that identifies specific challenges with planning, organization, and self-regulation, along with sensory sensitivities and communication preferences. Treatment plans are then customized to accommodate these differences instead of expecting individuals to conform to neurotypical standards.
| Treatment Component | Traditional Model | Neurodiversity-Affirming Model |
|---|---|---|
| Session Structure | Rigid 50-minute blocks; verbal-heavy. | Flexible lengths; movement breaks; visual supports. |
| Communication | Verbal processing expected immediately. | Written summaries; advance notice of changes; chat options. |
| Goal Setting | Standardized behavioral compliance. | Collaborative strategies (e.g., body doubling, visual systems). |
By honoring neurological differences as variations and not deficits, this approach creates a foundation where individuals can build sustainable recovery skills that genuinely work for their unique brain.
What You’ll Learn: In this section, you’ll discover how therapy models can be adapted to support the unique needs of neurodivergent adults in addiction recovery.
Standard talk therapy can feel like trying to solve a puzzle with the wrong pieces for many neurodivergent adults. People with autism, ADHD, or sensory processing differences may struggle with traditional group sessions that rely heavily on verbal communication or ignore sensory needs. That’s where adapted therapy models come in.
For example, cognitive behavioral therapy (CBT) can be redesigned with visual supports, written prompts, or flexible pacing to help a person process ideas in their preferred style. Some therapists use social stories, infographics, or quiet spaces to reduce anxiety and sensory overload. Research shows that when CBT is tailored this way, autistic adults see clinical improvement rates jump from 29% to 79%—a dramatic difference compared to standard approaches7.
Practice This: Create a simple worksheet or visual map that could help someone track their emotions or triggers in a way that feels comfortable for them.
Skill Checkpoint: You’re ready for the next level when you can explain why adapted therapy models are more effective for addiction recovery for neurodivergent adults.
What You’ll Learn: This section focuses on how medication-assisted treatment (MAT) can be thoughtfully integrated into addiction recovery, with special attention to unique risks and benefits.

Medication-assisted treatment—using medications like buprenorphine or methadone along with counseling—has been shown to reduce opioid-related deaths by more than 50%9. For neurodivergent adults, MAT can provide a stable foundation for recovery, especially when co-occurring conditions (like ADHD or anxiety) are managed alongside substance use disorder.
However, research shows that success with MAT hinges on adapting medication plans to account for sensory sensitivities, communication differences, and the possibility of co-occurring medications for neurodevelopmental conditions1. Some individuals may experience strong reactions to medication side effects or need extra support with medication routines, so clear communication and ongoing assessment are essential.
Practice This: Create a medication log that includes space for tracking how medications make you feel physically and emotionally. Try color-coding or using visual icons if that’s helpful.
Skill Checkpoint: You’re ready for the next level when you can describe one reason why adapting MAT is especially important in addiction recovery for neurodivergent adults.
Many neurodivergent individuals in recovery from addiction experience challenges with executive function—the mental processes that help with planning, organization, impulse control, and decision-making. For those with ADHD, autism, or other neurodevelopmental differences, these difficulties often existed before substance use began, though prolonged drug or alcohol use can further impact these skills.
Addressing executive function becomes essential for maintaining long-term recovery while honoring each person's neurological differences. Neurodiversity-affirming treatment programs incorporate strategies specifically designed for different cognitive profiles. Rather than expecting everyone to use the same organizational systems, therapists work with individuals to identify approaches that align with how their brains naturally function.
For someone with ADHD, this might mean using visual timers to create external structure for time awareness, or body-doubling sessions where tasks are completed alongside others for accountability. For autistic individuals, breaking complex tasks into detailed, sequential steps with clear completion criteria can reduce overwhelm and support follow-through.
Example: Reducing Cognitive Load
Recovery benefits from building routines that reduce the cognitive load of daily decisions. Establishing consistent sleep schedules, meal times, and medication routines creates a foundation that supports executive function development.
// Sample Routine for Executive Function Support 1. Morning: Medication + Visual Check-in (Green/Yellow/Red mood) 2. Mid-Day: 15-min "Body Double" session for admin tasks 3. Evening: Set out clothes/items for tomorrow (Visual Cue) For those with co-occurring ADHD or other neurodevelopmental conditions, this integrated approach proves particularly valuable. Treatment teams recognize that executive function challenges and addiction recovery are deeply interconnected, requiring interventions that address both simultaneously.
What You’ll Learn: This section explores what persistent cognitive challenges look like in addiction recovery for neurodivergent adults and introduces practical strategies to address them.
Persistent cognitive challenges—like trouble with focus, memory, or problem-solving—often remain even after someone completes traditional addiction treatment. Studies show that 30–80% of people with substance use disorder still experience executive functioning deficits, including difficulties with planning and self-control, long after treatment ends5. For neurodivergent adults, these issues might be even more pronounced.
A helpful way to think about this is to picture the brain as a traffic control tower. When the signals aren’t clear, it’s easy for things to get delayed or missed entirely. Addressing these issues means building in regular reminders, breaking tasks into smaller steps, and using tools like visual checklists or smartphone alerts. Individualized approaches, such as creating custom planners or practicing new organization strategies, can make a real difference.
Practice This: Choose a daily task you find challenging to remember or complete. Break it down into three smaller steps and set a reminder for each. Notice if this helps you finish the task more easily.
Skill Checkpoint: You’re ready for the next level when you can list two persistent cognitive challenges and match each with a practical support strategy.
What You’ll Learn: This section explores how peer support and lived experience models can help neurodivergent adults strengthen executive function skills on the path to recovery.
Peer support involves connecting with individuals who have personal experience navigating addiction recovery for neurodivergent adults. These peers can model organization skills, share real-world tools for managing routines, and offer encouragement when challenges arise. Studies show that peer recovery support services help bridge the gap between traditional treatment and everyday life, boosting engagement and lowering relapse rates by providing emotional and informational support outside the clinical setting6.
Think of it like learning a new game: having someone at your side who knows the rules—and the common obstacles—makes it easier to practice and improve. For neurodivergent adults, seeing executive function strategies in action from a peer who has "been there" can turn abstract concepts into usable habits.
Practice This: Reach out to a recovery peer or support group, and ask about one executive function tool that helped them in daily life. Try applying their advice to your own routines.
Skill Checkpoint: You’re ready for the next level when you can describe how peer support models make executive function skill-building more accessible during recovery.
For neurodivergent individuals, the clinical environment itself can present unexpected barriers to treatment. Bright fluorescent lighting, unfamiliar waiting rooms, and the sensory complexity of traditional treatment settings may create overwhelming experiences for autistic individuals. Those with ADHD-related executive function challenges often struggle with rigid appointment schedules and the multi-step process of getting to in-person sessions.
Virtual care addresses these neurodivergent-specific needs while simultaneously removing the traditional barriers that affect everyone seeking addiction treatment. Traditional addiction treatment often requires people to navigate rigid schedules, transportation challenges, and geographic limitations that can prevent them from getting help when they need it most. Virtual care fundamentally changes this equation by bringing evidence-based treatment directly to individuals wherever they are—in environments they control and find comfortable.
For people balancing work responsibilities, family obligations, or living in rural areas with limited treatment options, telehealth removes the need to commute hours for appointments or take extended time away from daily life. Consider these scenarios:
Virtual platforms also create opportunities for more consistent engagement. Instead of attending weekly sessions constrained by office hours, individuals can access support more frequently through video sessions, secure messaging, and digital resources. The privacy of virtual care also reduces stigma barriers, making it easier to take that crucial first step toward recovery.
What You’ll Learn: This section explains the specific reasons why remote treatment is especially effective for neurodivergent adults seeking addiction recovery.
Remote treatment offers a customized pathway for addiction recovery for neurodivergent adults by addressing barriers that often go unrecognized in traditional settings. Many find in-person clinics overwhelming due to sensory triggers—like fluorescent lights or crowded waiting rooms—which can make attending regular sessions nearly impossible. Virtual care allows individuals to participate from their own comfortable environments, controlling sensory inputs and reducing anxiety or distraction.
Research shows that satisfaction and retention rates for virtual addiction treatment programs exceed 80% for neurodivergent adults, likely because these platforms can be adapted for individual communication preferences and sensory needs10. The ability to use text, video, or even visual supports during sessions lets each person engage in ways that suit their brain best.
Practice This: Imagine your ideal therapy environment—what sensory aspects would you adjust to make it more comfortable? List two ways remote care could help you create that space.
Skill Checkpoint: You’re ready for the next level when you can explain two reasons remote care is a strong fit for addiction recovery in neurodivergent adults.
What You’ll Learn: This section explores how virtual care empowers neurodivergent adults to build sustainable recovery routines right at home.
Developing lasting recovery habits often means weaving new routines into daily life, not just attending therapy appointments. For neurodivergent adults, home-based virtual care makes it easier to practice skills like medication tracking, self-care, and healthy coping in the same environment where triggers and supports live side by side. Industry experts highlight that integrating therapy into daily home life—using reminders, visual checklists, or real-time coaching—can boost retention and make progress stick10.
Because virtual programs are designed for flexibility, individuals can set up their space, schedule sessions when energy is highest, and receive personalized feedback in real-world situations. This approach helps transfer new skills from the screen to daily routines, supporting sustainable change in addiction recovery for neurodivergent adults.
Practice This: Design a daily self-care checklist for your home routine. Include reminders for therapy sessions, medication, meals, and one activity that brings you calm or joy.
Skill Checkpoint: You’re ready for the next level when you can share two ways virtual care has helped you maintain healthy habits outside of appointments.
Recovery looks different for everyone, which is why effective treatment must be flexible enough to meet individuals where they are. Pathfinder Recovery provides specialized addiction treatment grounded in neurodiversity-affirming principles, offering personalized support that recognizes how neurodivergent minds process recovery differently.
The platform's approach combines evidence-based therapies with specific accommodations for neurodivergent needs. For clients with ADHD, this might mean offering flexible session lengths that align with attention patterns rather than rigid 50-minute appointments. Autistic clients receive written session summaries after each meeting, providing a reference point that reduces the cognitive load of remembering verbal discussions and supports executive function challenges common in both autism and addiction recovery.
What sets this model apart is its neurodiversity-informed adaptability. Treatment plans adjust not just for progress and setbacks, but for sensory sensitivities, communication preferences, and the processing differences discussed throughout this article. Because neurodivergent recovery rarely follows neurotypical timelines, the level of engagement shifts to match individual neurological needs rather than standardized protocols.
This specialized virtual care means accessing expert support that understands the intersection of neurodivergence and addiction—treatment that respects each person's unique neurological path forward rather than expecting conformity to traditional recovery models.
Many people wonder how addiction treatment differs for neurodivergent individuals. Treatment approaches are tailored to work with neurodivergent thinking patterns rather than against them. This means therapists might use more structured sessions for those with ADHD, incorporate visual supports for autistic individuals, or adjust communication styles to match how neurodivergent brains process information. Virtual care platforms can be particularly effective because they allow for customization of the treatment environment to reduce overstimulation.
Another common question involves whether virtual care can accommodate sensory sensitivities. Online treatment actually offers significant advantages for people with sensory processing differences. Individuals can control their environment—adjusting lighting, reducing background noise, wearing comfortable clothing, and taking breaks as needed. This flexibility helps neurodivergent people engage more fully in treatment without the sensory overwhelm that clinical settings can create.
People also ask what to do if they don't have an official ADHD or autism diagnosis but suspect they're neurodivergent. Many treatment providers welcome clients who are exploring whether neurodivergence plays a role in their substance use, even without formal diagnosis. Therapists can help identify patterns and adapt treatment approaches accordingly. Additionally, most insurance plans in Vermont, Massachusetts, Connecticut, and New Hampshire now cover telehealth appointments, making it easier to access specialized care that understands the neurodivergent experience.
Recognizing if your substance use is connected to your neurodivergence often starts with looking at your reasons for using and the patterns you notice. Many neurodivergent adults—those living with autism, ADHD, or sensory processing differences—report using substances to cope with challenges like sensory overload, social anxiety, or difficulty managing emotions7. If you find yourself reaching for substances when you’re overwhelmed by noise, bright lights, or stressful social situations, your neurodivergence may be a contributing factor. Another signal can be if traditional coping strategies don’t work as well for you, or if you notice your substance use increases in situations that trigger your sensory or emotional sensitivities. Addiction recovery for neurodivergent adults often means untangling these connections and finding healthier ways to manage discomfort. A specialist familiar with neurodiversity-affirming care can help you explore these patterns and create a plan that fits your unique needs.
Most people do not need to stop taking their ADHD or autism-related medications during addiction recovery—especially when care is tailored to neurodivergent needs. In fact, research shows that continuing appropriate psychotropic medication for conditions like ADHD or autism can actually help stabilize mood, reduce impulsivity, and lower the risk of substance use disorder relapse1. At Pathfinder Recovery, any decisions about medication are made in partnership with you and your prescribing provider. The care team will regularly review your medication plan to ensure safety, manage possible interactions, and support your unique recovery goals. Stopping or adjusting medications is only considered if there are clear medical reasons, and always happens with your informed consent. Open communication about your prescriptions is key to a safe, effective recovery process that respects both your neurodivergence and your well-being.
If traditional therapy approaches haven’t worked for you in the past, you’re not alone—and it doesn’t mean recovery is out of reach. Many neurodivergent adults find that standard talk therapy or group sessions don’t fit their communication style, sensory needs, or way of processing information. Research highlights that adapted therapy models—like visual supports, flexible pacing, or written communication—can dramatically improve outcomes for neurodivergent individuals, with clinical improvement rates rising to 79% when therapy is tailored to the person’s needs7. At Pathfinder Recovery, the focus is on neurodiversity-affirming care that meets you where you are, adapting strategies until you find what works. If you’ve struggled with therapy before, specialized addiction recovery for neurodivergent adults may offer a better path, using approaches designed for your brain and your lived experience.
Yes, many people continue working while participating in virtual addiction recovery for neurodivergent adults. Virtual care is designed for flexibility, allowing you to schedule therapy and support sessions around your job and daily responsibilities. Research shows that telehealth models boost engagement and retention for neurodivergent adults, in part because appointments can be arranged outside of typical work hours or during breaks in your day10. This means you don’t have to choose between your livelihood and your recovery. You can attend sessions from a quiet space at work, from home, or wherever you feel comfortable—no commuting or extra stress required. Pathfinder Recovery will help you build a routine that fits both your employment and your treatment goals, so you can keep moving forward on both fronts.
Pathfinder Recovery is highly attentive to sensory sensitivities during virtual sessions, recognizing that many neurodivergent adults can be easily overwhelmed by certain sights, sounds, or other sensory inputs. Clients are encouraged to choose their own comfortable environment for sessions, which means you can control lighting, background noise, and other sensory details. Therapists offer flexible communication methods, such as using text chat instead of video, sharing visual supports, or turning off cameras if that feels better. Sessions can be paused if needed, and clients are invited to request breaks or adjustments at any time. Studies reveal that programs offering sensory accommodations and individualized options see higher satisfaction and retention among neurodivergent participants10. This personalized, client-led approach helps make addiction recovery for neurodivergent adults more accessible and less stressful, so you can focus on healing in a way that feels right for you.
Yes, Pathfinder Recovery accepts insurance for neurodivergent-focused treatment, making specialized addiction recovery for neurodivergent adults more accessible in Vermont, Massachusetts, Connecticut, and New Hampshire. Many people worry about whether their insurance will cover care tailored to neurodivergence, but Pathfinder works directly with a variety of insurance plans to help reduce out-of-pocket costs. Research highlights that insurance coverage is one of the most significant factors in removing barriers to substance use disorder treatment, especially for those needing specialized services10. The Pathfinder team is available to help clients verify benefits, navigate paperwork, and advocate for coverage of co-occurring mental health and substance use support. If you’re considering virtual care, reaching out to Pathfinder for a confidential insurance check is a practical first step to see how your policy can support your recovery journey.
Pathfinder Recovery currently serves adults seeking virtual addiction recovery for neurodivergent adults in Vermont, Massachusetts, Connecticut, and New Hampshire. This means individuals living anywhere in these four states can access specialized, insurance-supported treatment from the comfort of their homes. The fully remote model removes common barriers like travel, transportation, and sensory discomfort often found in traditional clinics. Research shows that virtual care options make it much easier for neurodivergent adults to engage in consistent treatment by allowing sessions to happen in familiar environments and on flexible schedules10. If you reside in Vermont, Massachusetts, Connecticut, or New Hampshire and are interested in neurodiversity-affirming support, Pathfinder Recovery’s virtual program is designed to meet your needs.
The intersection of neurodivergence and addiction represents a critical area of understanding in mental health and substance use treatment. For individuals with ADHD, autism, and other forms of neurodivergence, addiction often emerges not as a character flaw but as an understandable response to neurological differences—whether through self-medication of challenging symptoms, coping with the exhaustion of masking, or managing the chronic stress of navigating a neurotypical world.
Effective treatment must acknowledge these realities. Neurodiversity-affirming care recognizes that traditional addiction treatment approaches designed for neurotypical individuals may miss essential elements of recovery for neurodivergent people. From addressing executive function challenges that impact treatment adherence to understanding stimming behaviors that might otherwise be misinterpreted, to recognizing sensory sensitivities that affect treatment environments—affirming approaches create space for authentic healing rather than demanding conformity to neurotypical standards.
For neurodivergent individuals seeking co-occurring mental health treatment alongside addiction recovery support in Vermont, Massachusetts, Connecticut, or New Hampshire, Pathfinder provides virtual care that honors neurological differences as natural variations rather than deficits. Virtual treatment offers particular advantages for neurodivergent individuals—reduced sensory overwhelm, familiar environments, and flexible scheduling that accommodates executive function challenges. Recovery doesn't require masking who you are—it begins with treatment that recognizes your neurodivergence as an integral part of your identity and builds support around your actual needs.

November 6, 2025

November 6, 2025