
The Power of Virtual Peer Coaching in Recovery
May 19, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
The concept of Dry January began in 2013 as a public health initiative encouraging people to abstain from drinking for the first month of the year. What started as a simple challenge has evolved into a global movement, with millions of participants discovering the profound benefits of taking a break from alcohol. For some, it's a reset button after holiday celebrations. For others, it's an opportunity to examine their relationship with drinking and explore what life might look like without it.
The power of this month-long commitment lies in its structured timeframe and collective participation. Having a defined 31-day period creates a manageable goal, while knowing others are on the same journey provides built-in accountability. Research shows that participants often experience:
Many report feeling more emotionally balanced and discovering new ways to socialize and unwind without relying on alcohol. For individuals in recovery or those questioning their drinking patterns, the January sobriety challenge can serve as a gateway to longer-term abstinence. It offers a socially acceptable framework to explore life without alcohol, free from the pressure or stigma that sometimes accompanies the decision to stop drinking.
While the January challenge provides an excellent starting point, many participants discover they need ongoing support to maintain their progress. Building sustainable habits requires more than willpower alone—it demands structure, community, and professional guidance. Virtual services have made this support more accessible than ever, removing traditional barriers like transportation and scheduling conflicts. Pathfinder Recovery offers this type of accessible online support throughout the New England region, spanning VT, MA, CT, and NH. Through integrated behavioral health treatment alongside addiction support, individuals can access the resources they need from the comfort and privacy of home.
Think of a month without alcohol as a diagnostic tool. By pausing alcohol use, you often notice patterns—such as reaching for a drink to manage stress or out of habit during social gatherings—that were previously automatic. Studies reveal that these insights are common experiences among those practicing mindful sobriety and exploring an alcohol-free lifestyle1. It acts like holding up a mirror, making it easier to see emotional triggers and social pressures that influence your choices.
Create a personal journal entry outlining when you most wanted to drink. Check if any of these were present:
You're ready for the next level when you can recognize two distinct triggers or routines tied to your drinking habits. Next, let's dig into the science behind what happens to your body and brain during 30 days of abstinence.
When you stop drinking, your brain starts to rebalance its reward systems. Alcohol artificially spikes dopamine, and over time, the brain relies on it to feel "normal." During a break, these pathways begin to heal, helping you enjoy regular activities again instead of relying on alcohol for pleasure10. At the same time, the body’s stress response and mood regulation mechanisms begin to stabilize, leading to that "clear-headed" feeling many participants report.
Practice This: Write down one noticeable change in your motivation, mood, or enjoyment of daily life since beginning your alcohol-free month.
Think of the body like a reset button—when alcohol is paused, many people quickly notice more restful sleep, clearer skin, and increased daily energy. Research shows that a single month of abstinence leads to measurable benefits2.
| Timeline | Physical Benefit | Impact on Daily Life |
|---|---|---|
| Week 1 | Improved Hydration & Sleep | Waking up feeling refreshed rather than groggy. |
| Week 2 | Reduced Acid Reflux | Better digestion and less stomach discomfort. |
| Week 4 | Liver Fat Reduction | Improved energy and metabolic function. |
Practice This: Track your sleep, energy, or physical changes in a daily log for one week. Which improvement stands out the most? You're ready for the next step when you can name two physical benefits you’ve experienced and explain how they motivate you.
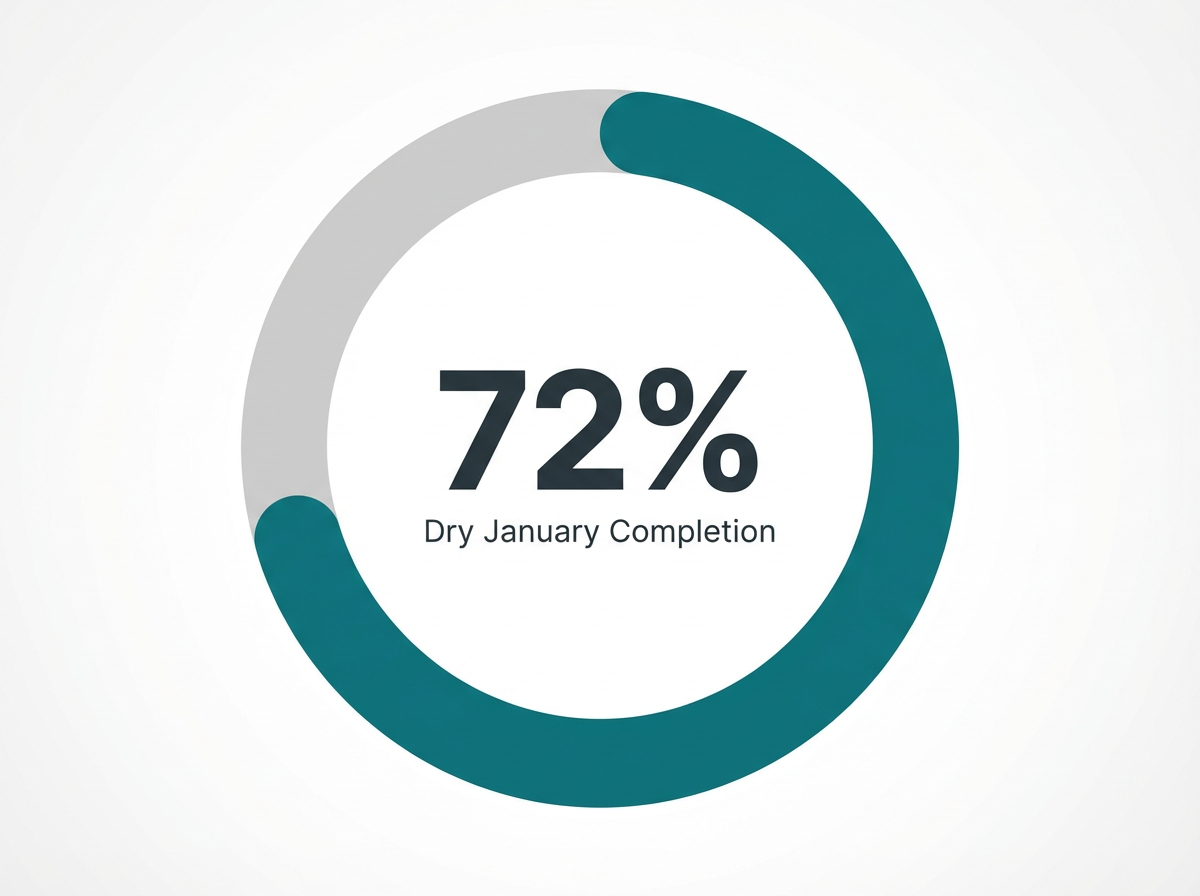
The momentum of Dry January can spark lasting transformation beyond just a single month. Building on early wins like improved sleep and mood helps shift your mindset from a temporary "challenge" to a sustainable lifestyle change. Research shows that while 72% of participants complete Dry January, only a smaller portion continue long-term, highlighting the gap between short-term success and lifelong recovery5.
Practice This: List two habits or routines that supported your success during the month and brainstorm how you could carry them into the months ahead.
Why do so many people finish the month but struggle to keep going? After the initial excitement fades, daily routines and old social cues often creep back in.
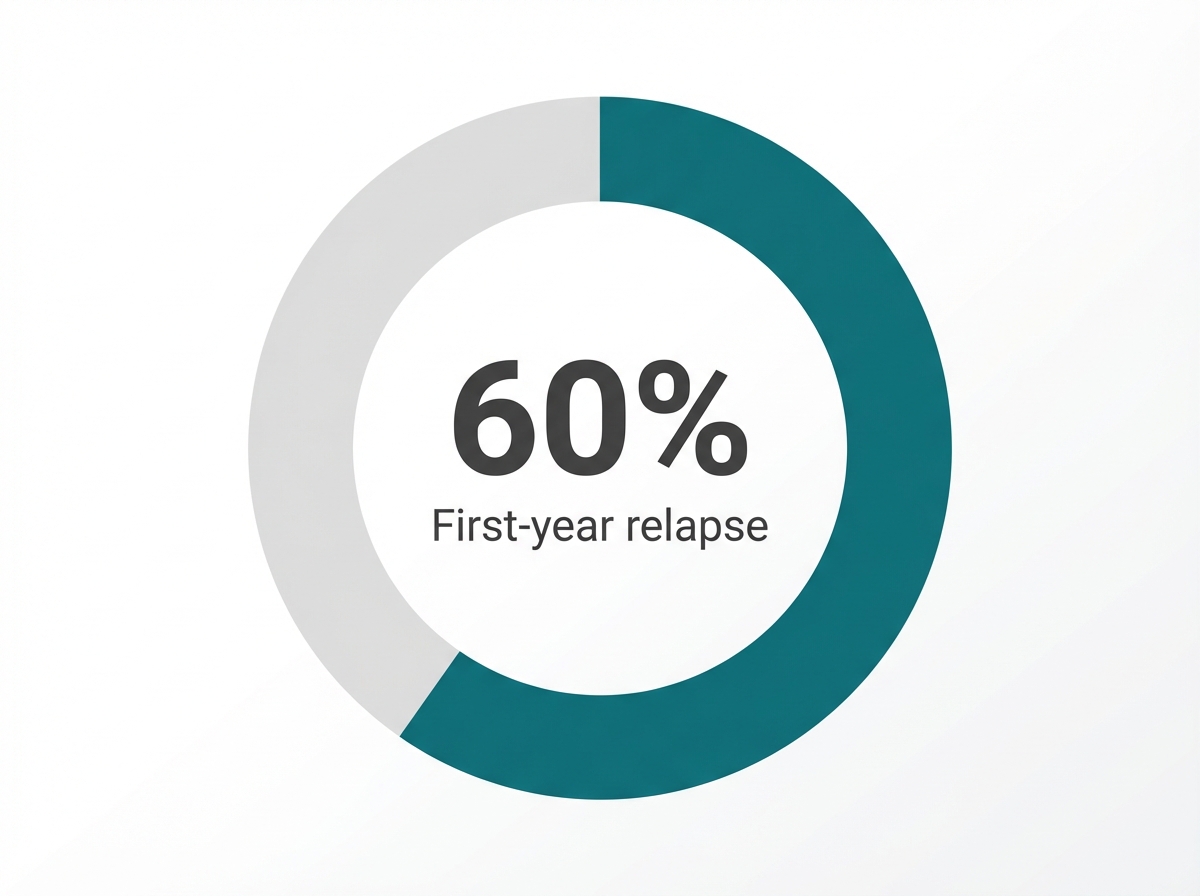
"Research indicates that more than 60% of individuals will return to drinking within a year of finishing treatment or a structured break." 5
Without ongoing support or new habits to replace drinking, it’s easy to slip into previous patterns. This doesn't mean short-term success is pointless. It simply means that alcohol-free living is a journey, and setbacks are manageable with the right strategies.
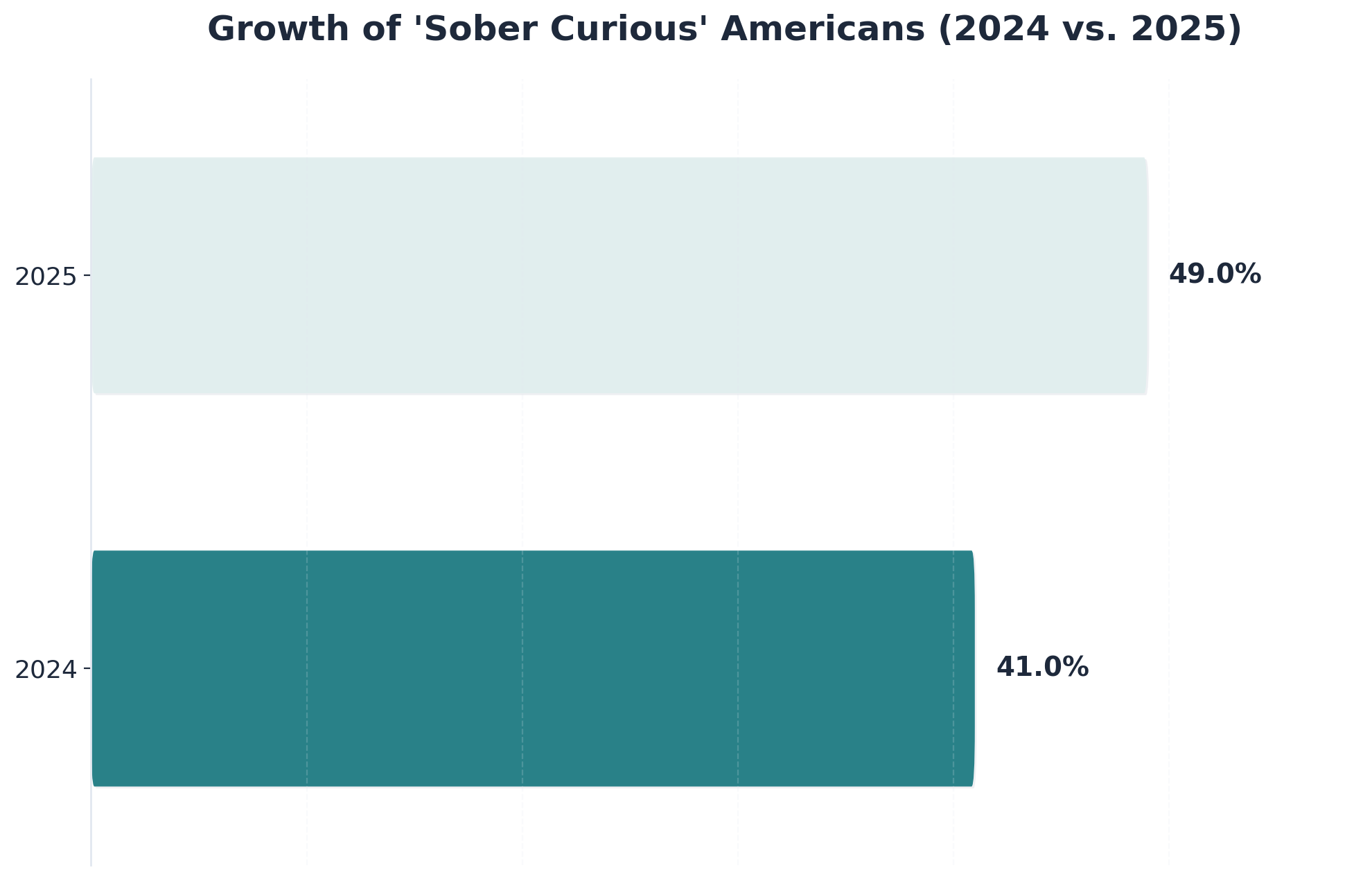
The first step to lasting change is recognizing your unique starting point. Everyone’s relationship with alcohol, triggers, and motivation levels are different. Research shows that nearly half of Americans are now exploring alcohol-free living, with 65% of Gen Z planning to reduce their drinking in 20257.
Practice This: Complete a self-check by listing your reasons for starting Dry January, your biggest challenge, and what support has helped you most so far. You’re ready for the next level when you can clearly describe your top motivator, main risk factor, and one resource you can depend on.
The transition from temporary abstinence to permanent change represents one of recovery's most critical junctures. Building sustainable habits requires more than willpower—it demands a structured approach that addresses both the behavioral patterns and underlying factors that influence drinking behaviors.
The key to enduring success lies in replacing old routines with new, healthier alternatives. This means identifying your triggers—whether they're social situations, stress from work, or evening boredom—and developing specific strategies to manage them.
Accountability structures play an essential role in maintaining momentum. Daily text check-ins with an accountability partner or weekly video calls with a recovery coach help reinforce your commitment during vulnerable moments. Pathfinder Recovery understands that sustainable sobriety requires ongoing support tailored to individual needs. Through virtual services available throughout the New England region—spanning Vermont, Massachusetts, Connecticut, and New Hampshire—individuals can access addiction treatment and integrated behavioral health support from the comfort of their own homes.
Think of your recovery architecture as building a new daily blueprint—each routine acts like a brick, reinforcing your choice to avoid alcohol. Research shows that people who layer in structured habits and supportive environments after Dry January are far more likely to maintain mindful sobriety9.
Practice This: Map out your day, noting which old drinking patterns you’ll swap for positive routines (like exercise or cooking). Then, add one environmental change—such as removing alcohol from your space or adding reminders of your goals.
Replacing alcohol routines isn’t about losing pleasure—it’s about swapping one set of patterns for another that actually supports well-being. Habit experts liken this to changing the tracks a train runs on: once the new rails are in place, the ride becomes much smoother.
Practice This: Identify one time of day you used to drink and plan a new activity for that slot—such as joining an online cooking class, preparing a favorite alcohol-free beverage, or scheduling a check-in with a peer. Try it for three days and note your mood or cravings afterward.
Triggers are like hidden switches: a stressful day, a certain place, or even a celebratory mood can all spark cravings. Research shows that understanding your own patterns is one of the strongest predictors of long-term success9.
Practice This: Write down three moments in the past week when you felt tempted to drink. Next to each, jot a simple plan—such as texting a friend, taking a walk, or practicing mindful breathing—to use the next time that trigger appears.
Building lasting sobriety often requires more than willpower or new routines. Studies reveal that over 60% of people relapse within their first year of recovery, showing that ongoing support is critical9. Professional resources—such as therapy for substance use disorder, co-occurring mental health treatment, or peer recovery coaching—offer proven strategies and accountability.
Evidence-based therapies are like a tailored toolkit for overcoming substance use. Here is how different approaches support your journey:
| Therapy Type | How It Helps |
|---|---|
| Cognitive Behavioral Therapy (CBT) | Helps you spot and change unhelpful thinking patterns that lead to drinking. |
| Trauma-Informed Care | Recognizes the role of past experiences and builds trust and safety. |
| Integrated Treatment | Addresses substance use and co-occurring mental health issues together3. |
Practice This: Research one evidence-based therapy and write down one way it could support your journey after an alcohol-free month.
Imagine if seeing a recovery specialist was as easy as joining a video call from your living room. Virtual care turns that idea into reality, helping individuals across Vermont, Massachusetts, Connecticut, and New Hampshire receive substance use disorder treatment and co-occurring mental health care from home. Studies reveal that virtual programs reduce major obstacles like stigma, travel, and limited provider options9.
As individuals progress beyond the initial months of sobriety, the focus shifts from simply avoiding alcohol to building a life where recovery becomes an integrated part of daily existence. Sustained abstinence requires developing sophisticated coping mechanisms that address the complex challenges life presents—from managing stress during career transitions to navigating relationships and processing grief without turning to alcohol.
Advanced recovery practices often include identifying and addressing underlying patterns that contributed to addiction in the first place. This might involve working through trauma with specialized therapists, developing emotional regulation skills that extend beyond basic mindfulness, or creating detailed relapse prevention plans.
Pathfinder Recovery provides virtual support throughout the Northeast region, offering individuals across Vermont, Massachusetts, Connecticut, and New Hampshire the ability to continue their recovery work from home. For those managing dual diagnoses—addressing both psychiatric conditions and addiction—having accessible professional care creates a safety net that helps prevent relapse during vulnerable moments.
Relapse can feel like taking a wrong turn, but industry leaders find it’s actually a normal part of most recovery journeys. Research shows that over 60% of people experience a relapse in their first year after treatment or a period of abstinence9. By understanding your personal patterns, you can build a proactive plan to catch warning signs early.
Research shows that relapse is not a sign of failure but a common stage in the recovery journey, heavily influenced by factors like stress, low self-confidence, and returning to old environments8. For many, the excitement and structure of temporary abstinence fade over time, making it easier to slip back into old habits unless new routines and supports are in place.
Think of a relapse protocol as your recovery emergency kit. Studies reveal that people who map out their responses in advance are better equipped to maintain mindful sobriety9.
Your Protocol Checklist:
Long-term sobriety thrives on connection. Research consistently demonstrates that individuals with strong family support experience better treatment outcomes and lower relapse rates than those without it6. Alcohol-free living becomes more sustainable with a network of encouragement—think of it as a team sport.
Family involvement is like adding extra reinforcements to your recovery foundation. When family members are included, they can encourage healthy routines, celebrate wins, and help spot early signs of struggle. Programs like CRAFT (Community Reinforcement and Family Training) teach families how to support recovery without enabling substance use6.
Peer recovery coaches are individuals in long-term recovery who offer guidance, encouragement, and honest feedback based on their own journeys. Unlike traditional counselors, peer coaches draw from personal experience with substance use disorder. Research shows that people who receive peer support alongside clinical treatment have higher engagement and better recovery outcomes4.
The insights gained from an alcohol-free January often reveal a deeper truth: temporary challenges can illuminate the path to permanent change. Whether a month-long alcohol break sparked a realization about drinking patterns or a desire to build healthier habits, sustainable recovery begins with accessible, evidence-based treatment tailored to individual needs.
Building lifetime sobriety means developing new coping mechanisms, addressing underlying challenges, and creating routines that support sustained wellness. This process involves understanding triggers, learning to navigate social situations without alcohol, and establishing meaningful connections with others who understand the recovery journey. Research consistently shows that individuals with ongoing support systems maintain sobriety at significantly higher rates than those attempting recovery alone.
Pathfinder Recovery provides virtual outpatient treatment for addiction throughout the New England region, including Vermont, Massachusetts, Connecticut, and New Hampshire. This telehealth approach removes common barriers to treatment—no commute, no waiting rooms, and no disruption to work or family responsibilities. Participants can access individual therapy, group sessions, and medication-assisted treatment from the privacy and comfort of their own homes.
For those managing both addiction and behavioral health concerns, Pathfinder offers integrated dual diagnosis treatment. This coordinated approach addresses both conditions simultaneously, recognizing that lasting recovery requires treating the whole person rather than isolated symptoms.
If the clarity gained during a month without alcohol has revealed concerns about your relationship with drinking, now is the moment to act on that awareness. Schedule a confidential consultation with a recovery specialist, assess your drinking patterns using evidence-based screening tools, or connect with others who have successfully transformed temporary sobriety into lasting freedom. The momentum built during a challenge like Dry January creates a unique window of opportunity—one that, when paired with professional support, can mark the beginning of profound and permanent transformation.
Many people have questions about January sobriety challenges and what they mean for their sustained relationship with alcohol.
Yes, you can participate in virtual recovery support if you live in Vermont, Massachusetts, Connecticut, or New Hampshire. Pathfinder Recovery is specifically designed to serve individuals in these states through secure telehealth platforms, offering substance use disorder care and support for co-occurring mental health needs. Virtual recovery makes it easier to access help from home—whether you’re continuing mindful sobriety after dry January, exploring alcohol-free living, or seeking ongoing support. Research shows that virtual treatment removes barriers like travel and stigma, making recovery more accessible and effective for many people pursuing a sober curious lifestyle9. If you’re looking for flexible, confidential support from your own space, virtual options can fit seamlessly into your recovery journey.
Yes, Pathfinder Recovery offers medication-assisted treatment (MAT) as part of its virtual substance use disorder services for individuals in Vermont, Massachusetts, Connecticut, and New Hampshire. MAT combines FDA-approved medications with evidence-based therapies to support recovery and reduce cravings, making it a valuable tool for those working to maintain alcohol-free living or mindful sobriety after dry January. Research shows that integrating medications with counseling and behavioral support improves treatment outcomes and helps people stay engaged in long-term recovery9. Pathfinder’s telehealth approach makes MAT accessible from home, providing flexibility and ongoing support for those seeking sustainable change.
Yes, you can receive substance use disorder treatment and co-occurring mental health support from home—without needing to take time off work. Virtual recovery programs are built for flexibility, allowing you to schedule appointments around your daily routine, including work or family commitments. Studies reveal that telehealth removes traditional barriers like travel, time off, and stigma, making it much easier for people to maintain alcohol-free living or mindful sobriety after completing dry January9. This remote approach is especially helpful for individuals in Vermont, Massachusetts, Connecticut, and New Hampshire who need convenient, confidential support. With virtual care, you can keep building on your sober curious or alcohol-free lifestyle while balancing work and recovery—all from the comfort of your own space.
Pathfinder Recovery uses a range of evidence-based therapies to support individuals with substance use disorder and co-occurring mental health needs. Their core approaches include cognitive behavioral therapy (CBT), which helps people identify and change thought patterns that drive substance use, and trauma-informed care, designed to build trust and address the impact of past experiences. For those with both substance use and mental health challenges, Pathfinder offers integrated treatment that addresses both at the same time—a method proven to improve outcomes3, 9. Peer recovery coaching is also part of their toolkit, providing real-world support from those with lived experience. These therapies work together to help people maintain mindful sobriety, continue alcohol-free living after dry January, and build resilience for lifelong recovery.
Wondering if your drinking is problematic enough to seek professional help is a common and important question—especially for those reflecting after dry January or exploring mindful sobriety. You don’t need to wait for a crisis or hit a specific “low” to reach out. Signs you might benefit from support include drinking more or longer than planned, trouble cutting back, using alcohol to cope with stress or emotions, or having it affect your health, relationships, or work. Research shows that many people who try an alcohol-free month already sense their drinking may be a concern, even if they haven’t sought formal help before1. If you feel uncertain, a self-assessment or conversation with a professional can clarify your next steps. Participating in the sober curious movement or alcohol-free living is a valid reason to seek guidance—early action makes lasting change more likely.
Peer recovery coaching plays a vital role in long-term sobriety by offering practical, ongoing support from someone with lived experience in substance use recovery. These coaches aren’t just advisors—they’ve walked the path themselves, which helps build trust and a sense of partnership that many find missing in traditional care. Research shows that individuals who receive peer support alongside clinical treatment are more likely to stay engaged with their recovery plan and experience better outcomes—especially after completing an alcohol-free month like dry January4. Peer coaches can help with accountability, encouragement during setbacks, and sharing real-world strategies for alcohol-free living or mindful sobriety. Their understanding and guidance make it easier to overcome obstacles and maintain progress, making peer recovery coaching a powerful addition to sustainable recovery.
Yes, many virtual treatment programs for substance use disorder and co-occurring mental health needs are covered by insurance—including both private plans and Medicaid in Vermont, Massachusetts, Connecticut, and New Hampshire. Coverage can vary by provider and plan, so it’s a good idea to confirm details with your insurance company or the treatment provider before starting care. Research shows that expanding insurance coverage for telehealth has made alcohol-free living and mindful sobriety support much more accessible, especially for those continuing their recovery after dry January9. If you’re interested in virtual care, ask providers about their accepted insurance and any out-of-pocket costs so you can make an informed decision for your recovery journey.
Virtual care offers many of the same evidence-based therapies and recovery supports as traditional in-person rehab programs, but with greater accessibility and flexibility. Instead of requiring travel or time away from home, individuals can join sessions from anywhere in Vermont, Massachusetts, Connecticut, or New Hampshire. Research shows that virtual treatment removes barriers like stigma and transportation, and can be just as effective for supporting alcohol-free living and mindful sobriety after dry January9. While in-person rehab may provide more structure for some, virtual models empower people to fit recovery around their lives—making long-term change more realistic for many. If privacy, convenience, or ongoing access are priorities, virtual care could be a strong fit for sustainable recovery.
Virtual treatment platforms are designed with privacy in mind, so your employer or colleagues will not be notified if you seek help. All telehealth services for substance use disorder and co-occurring mental health care are protected under strict confidentiality laws, including HIPAA, which means your participation remains private unless you choose to share it. Research shows that concerns about stigma and workplace discovery can be major barriers to seeking support, but virtual care offers a discreet way to practice mindful sobriety and continue alcohol-free living after dry January9. If you use personal devices and secure connections, your recovery journey stays confidential and under your control.
If you experience a relapse during your first year of recovery, you’re not alone—research shows that over 60% of individuals return to substance use at least once in the first year after treatment or a structured break like dry January9. A relapse isn’t a sign of failure; it’s a common and manageable part of the recovery journey. What matters is how you respond: acknowledging the slip, reaching out for support, and revisiting your recovery plan are key steps. Many people practicing mindful sobriety or alcohol-free living find that identifying triggers and using relapse response strategies—like connecting with a peer coach or adjusting daily routines—can help them get back on track. Every setback is an opportunity to learn and strengthen your long-term progress.
Yes, Pathfinder Recovery can help if you are experiencing both a substance use disorder and challenges like anxiety or depression. While Pathfinder does not offer primary mental healthcare, the team specializes in treating co-occurring mental health conditions alongside substance use disorder—all through accessible telehealth for residents of Vermont, Massachusetts, Connecticut, and New Hampshire. Research shows that substance use and mental health issues are deeply connected, often creating a cycle where one impacts the other. Integrated care, which addresses both at the same time, is proven to improve outcomes for people seeking long-term recovery and alcohol-free living after dry January3, 9. Pathfinder’s approach combines evidence-based therapies and support, helping you build stability and confidence in your recovery journey.
Family can play a powerful role in your recovery journey after dry January. Research consistently shows that individuals with strong family support are more likely to achieve lasting alcohol-free living or maintain mindful sobriety, with better treatment outcomes and lower relapse rates6. Your family can help by encouraging new routines, offering accountability, celebrating your wins, and even spotting early warning signs if challenges arise. Many people find it helpful to set up regular check-ins, involve family in shared activities that don’t center on alcohol, or invite loved ones to learn about healthy support strategies. Programs such as CRAFT (Community Reinforcement and Family Training) also guide families in providing encouragement without enabling substance use. Including family creates a team mentality, making the transition from dry January to long-term sobriety much more sustainable.
Yes, virtual recovery support can be effective for people with ADHD or autism, especially when tailored to individual needs. Many neurodivergent individuals benefit from the flexibility and reduced sensory demands of telehealth, which can make it easier to build alcohol-free living routines after dry January. Research shows that customizing recovery strategies—like using visual reminders, shorter check-ins, or sensory-friendly environments—increases success rates for those with ADHD or autism9. Virtual programs allow for more personalized scheduling and can adapt resources to fit unique learning styles, supporting mindful sobriety and the sober curious lifestyle. If standard routines feel overwhelming, virtual care offers creative options so you can experiment and discover what works best for your recovery journey.
If you’ve tried traditional rehab before and didn’t find lasting results, you’re not alone—and your recovery path isn’t over. Research shows that more than 60% of individuals experience a relapse within the first year after treatment, highlighting how common it is to need additional or different support9. Many people discover that a single approach doesn’t fit everyone, especially when building alcohol-free living or mindful sobriety after dry January. Virtual care and evidence-based therapies—like cognitive behavioral therapy and peer recovery coaching—offer new options that can be tailored to your needs. These flexible, accessible supports allow you to experiment, learn from past attempts, and build a recovery plan that addresses your unique challenges and strengths. Progress isn’t always linear; each experience adds insight and resilience for your next steps toward sustainable sobriety.
You can start receiving support almost immediately after completing Dry January—often within days, sometimes even the same week. Virtual recovery programs serving Vermont, Massachusetts, Connecticut, and New Hampshire make it easy to connect with substance use disorder specialists and peer support without waiting for lengthy intake processes. Research shows that prompt access to care is vital for maintaining momentum from a temporary alcohol-free challenge and reduces the risk of early relapse9. Whether you’re looking to continue your mindful sobriety journey or need help with alcohol-free living, quick enrollment in virtual programs means you don’t have to lose the progress you’ve made. After finishing Dry January, taking that next step right away helps turn a month-long effort into lasting change.

May 19, 2025

December 12, 2025

November 6, 2025