
Addiction Relapse Prevention Program: Virtual Treatment that Meets You Where You Are
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Mental health literacy goes far beyond simply knowing the names of different conditions or recognizing symptoms in yourself or others. It encompasses a comprehensive understanding of mental health information that empowers individuals to make informed decisions about their well-being and recovery journey.
At its core, this literacy includes four key components: recognizing when emotional or psychiatric challenges are developing, understanding their causes and available treatments, knowing how to seek appropriate help, and reducing the stigma that often prevents people from accessing care. This knowledge base becomes particularly crucial for individuals navigating both addiction and concurrent psychiatric disorders, where the interplay between these challenges requires nuanced understanding.
"Research consistently demonstrates that higher psychological literacy correlates with earlier intervention, better treatment outcomes, and reduced feelings of shame or isolation."
When someone understands that depression, anxiety, trauma-related conditions, and other psychiatric challenges are legitimate medical concerns with evidence-based treatments, they are more likely to pursue help without delay. This literacy also involves understanding the recovery process itself. This means recognizing that healing isn't linear, that setbacks don't equal failure, and that integrated treatment approaches often yield the strongest outcomes.
For those managing dual diagnoses, this knowledge helps contextualize why addressing both addiction and emotional well-being simultaneously proves more effective than treating either in isolation. Perhaps most importantly, psychological literacy includes knowing what questions to ask providers, understanding treatment options available in your region, and recognizing the difference between various levels of care.
Mental health information literacy is the skill set that enables a person to find, understand, and use reliable resources about emotional well-being, mental illnesses, and treatment options. In plain terms, it’s about more than memorizing symptoms—it means knowing how to identify trustworthy information, ask the right questions, and make informed choices for yourself or a loved one.
Industry experts describe this as the ability to "learn about mental health," including recognizing signs and symptoms, understanding risk factors, and knowing what support resources exist1. Mental health information literacy focuses specifically on the unique aspects of mental well-being, such as stigma, emotional language, and the often hidden nature of symptoms. As digital platforms expand access, being able to critically evaluate mental health resources has become essential for navigating both professional and self-help pathways4.
To build strong mental health information literacy, it helps to know the six key components experts highlight:
Each element strengthens a person’s ability to navigate emotional wellness and mental illness, especially when faced with substance use challenges. For instance, being able to spot early signs of anxiety or depression and knowing where to find accurate resources can make a significant difference in seeking support quickly. This approach is ideal for anyone looking to make informed decisions about their own care or to support a loved one1.
Positive mental health literacy focuses on understanding how to maintain well-being—not just how to spot problems. This aspect of mental health information is crucial because it empowers people to build resilience, cope with stress, and form healthy habits before crises occur.
Studies reveal that positive mental health literacy explains 41% of the difference in mental well-being among adolescents, showing its real-world impact on daily life3. This solution fits individuals and families aiming to prevent issues, not just react to them. By learning skills like emotional regulation and self-care, people can reduce the risk of developing mental health conditions or relapsing in recovery.
Many people seeking mental health information for both substance use disorder (SUD) and co-occurring mental health conditions face a significant information gap. Even with digital resources more available than ever, a large portion of adults with co-occurring conditions struggle to find, understand, or act on relevant details about integrated care.
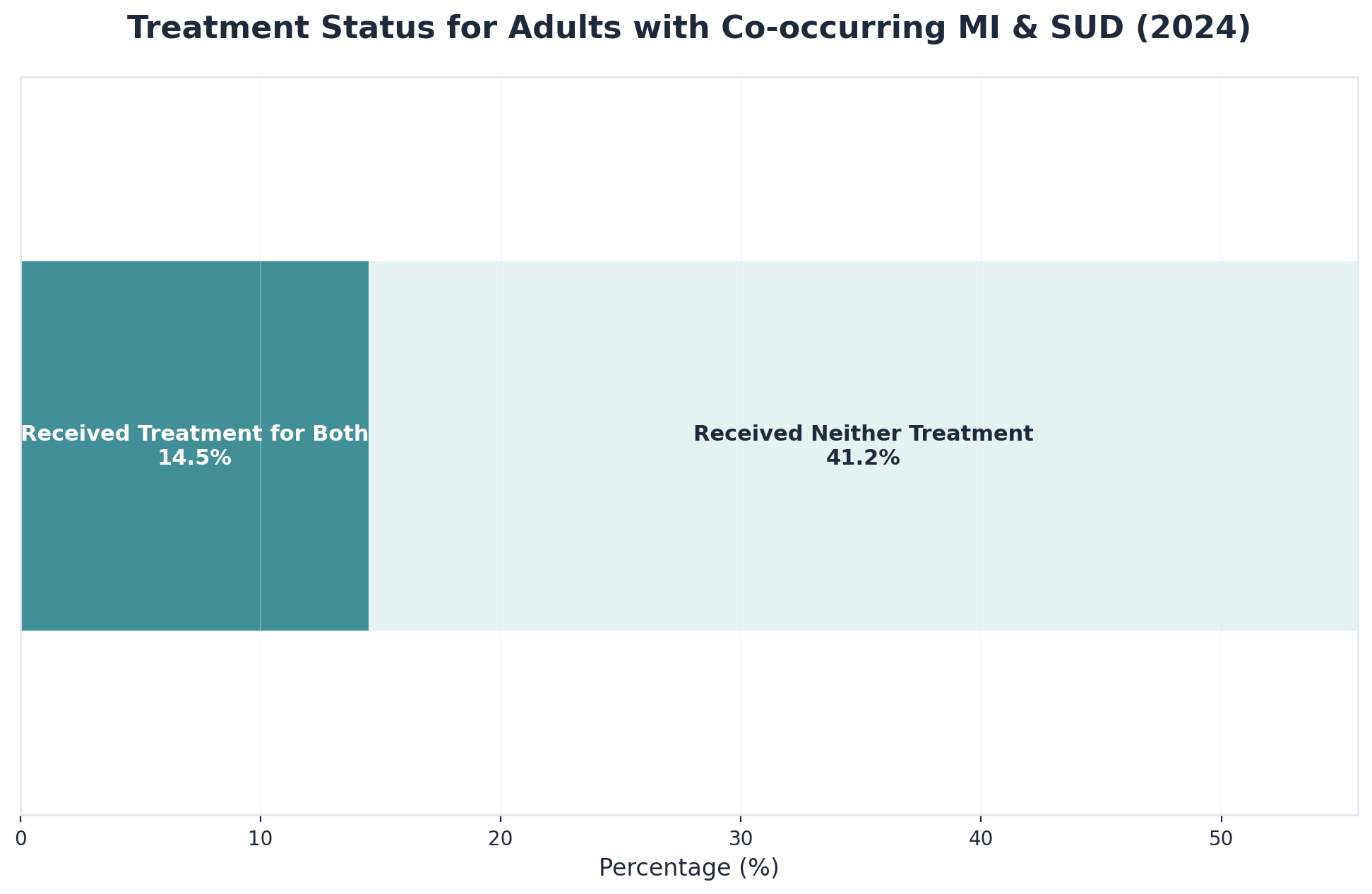
Recent data highlights that out of 21.2 million adults with both a mental illness and SUD, only 14.5% received treatment for both, while 41.2% received no treatment at all—underscoring a real disconnect between available resources and actual access to care10. This approach works best when mental health resources address the complex overlap of addiction and emotional wellness, not just one or the other.
A striking 41.2% of adults living with both a mental illness and substance use disorder received no formal treatment for either condition in 2024, despite the surge in digital mental health information and integrated treatment information online10. This treatment gap is not just a statistic—it reflects the real struggle many face in translating available mental health resources into actionable care.
Industry leaders find that the challenge often lies in navigating fragmented systems and unclear guidance, especially for those dealing with co-occurring disorders. For small organizations or families trying to support a loved one, the lack of unified, actionable mental health information can lead to confusion or missed opportunities for timely intervention.
Stigma—meaning negative attitudes or discrimination toward people with mental health or substance use conditions—remains a major barrier to accessing mental health information and co-occurring disorder resources. For many, the fear of being judged or misunderstood discourages even the first step of searching for support or learning about integrated treatment information.
Research shows that more than half of individuals living with mental illness do not seek help, often due to concerns about social rejection or job loss2. This path makes sense for organizations and individuals aiming to reduce disparities: addressing stigma can open doors to accurate, life-changing information, especially for those with co-occurring disorders.
Before diving into specific resources or programs, take a moment to identify where you currently stand with psychological wellness knowledge. This self-assessment helps you choose learning pathways that match your actual needs rather than following a one-size-fits-all approach.
Start by asking yourself what prompted this search for emotional and behavioral health literacy. Are you supporting someone on their recovery journey who experiences dual diagnosis challenges? Perhaps you work in a field where understanding trauma responses or mood disorders would strengthen your effectiveness. Or maybe you're building your own foundation of knowledge to better navigate personal experiences.
| Assessment Area | Key Questions to Ask Yourself |
|---|---|
| Knowledge Baseline | Can you name three evidence-based treatments? Do you know the difference between a psychiatrist and a psychologist? |
| Warning Signs | Can you identify at least two signs of a crisis (e.g., sudden withdrawal)? Do you recognize how SUD and mood disorders intersect? |
| Learning Style | Do you prefer clinical research articles, interactive workshops, or peer discussion groups? |
| Time Commitment | Realistically, can you dedicate 2 hours or 10 hours weekly to building this literacy? |
Your learning goals matter just as much as your starting point. Some people need practical skills for supporting loved ones through crisis moments. Others seek deeper understanding of how psychological disorders develop and progress. Healthcare professionals or social workers might require specialized knowledge about concurrent disorders and integrated treatment models.
Begin your self-assessment with these diagnostic questions: What specific mental health information are you seeking—general wellness tips, signs of co-occurring disorders, or integrated treatment information? Are you comfortable distinguishing between reliable resources and social media opinions?
Research highlights that excess information, especially from digital sources, can amplify confusion and make it harder to move forward with care decisions9. This approach works best for individuals who want clarity on their unique needs before sifting through countless online articles or forums. By reflecting on your current confidence level and pinpointing where you feel uncertain, you’ll be better equipped to target your search.
A quick way to evaluate your current knowledge level is to list what you already understand about mental health information and where you feel unsure. Try this checklist:
Studies reveal that excess digital content can cloud judgment, so it helps to clarify what topics you grasp and which ones create confusion9. This approach is ideal for those aiming to avoid overwhelm from integrated treatment information or mental health stigma.
To pinpoint your barriers to finding and using mental health information, use this checklist: Are you overwhelmed by too much digital content? Do you feel unsure about which sources are reliable? Are concerns about mental health stigma or privacy holding you back from seeking co-occurring disorder resources?
Studies reveal that excess information, especially online, can actually cause confusion and make it harder to reach decisions about care9. This solution fits individuals who want to avoid digital mental health over-literacy—a state where an overload of advice and opinions creates more anxiety than clarity.
To help you cut through the noise, use this simple decision tree: First, ask yourself if the source is from a recognized authority such as a government health agency, respected research institution, or licensed clinical provider. Then, check whether the mental health information is current (published or reviewed within the past two years) and focused on evidence-based practices.
This path makes sense for anyone feeling lost in a sea of online content, especially when evaluating co-occurring disorder resources. Studies reveal that excess digital information can actually cloud judgment, making it hard to identify trustworthy integrated treatment information9. For example, if you’re comparing a peer-reviewed article about substance use and mental illness with advice from a social media influencer, prioritize the one with professional review and clear references.
Use this quick checklist when evaluating any mental health information:
Evidence-based mental health resources, such as those from the National Institute of Mental Health, consistently update their materials and cite recent studies4. This method works when you want to cut through digital clutter and avoid misinformation about co-occurring disorders or integrated treatment options.
To steer clear of digital over-literacy traps, start with this quick self-check: How often do you find yourself scrolling through endless articles, forum threads, or social media posts about mental health information, only to feel more anxious or confused? Digital mental health over-literacy happens when the sheer amount of content—especially algorithm-driven and emotionally charged material—overwhelms your ability to sort facts from speculation.
Studies reveal that excess information can actually lead to confusion, fear, and even identity destabilization, instead of providing clarity or support9. This solution fits anyone who feels caught in a cycle of searching for answers but never feeling satisfied. Limiting your daily intake of integrated treatment information, setting boundaries around digital consumption, and choosing a few trusted sources can help you avoid the pitfalls of overexposure.
Your pathway to strengthening mental health literacy depends on your relationship to mental health and your specific learning goals. Different roles require different knowledge depths and resource types, though everyone benefits from foundational understanding of mental health concepts and support strategies.
For family members and caregivers supporting loved ones with mental health conditions, prioritize resources that combine emotional support with practical guidance. Family-to-family education programs offered by organizations like NAMI provide structured curricula alongside peer connection with others navigating similar experiences. Online support communities and caregiver-specific workshops offer ongoing learning while addressing the isolation many supporters feel.
Healthcare workers and helping professionals need more comprehensive training that integrates mental health literacy into their existing practice. Professional development courses through licensing boards, mental health first aid certification programs, and specialty trainings in trauma-informed care build competencies for recognizing and responding to mental health needs.
Individuals in recovery or managing their own mental health conditions often benefit most from peer-led educational opportunities that validate lived experience while building knowledge. Peer support specialist training programs, recovery education courses, and wellness self-management curricula like WRAP (Wellness Recovery Action Plan) combine evidence-based information with experiential learning.
For the general public seeking foundational mental health literacy, accessible entry points include free online courses from universities, public awareness campaigns from mental health organizations, and community education events. These resources typically cover mental health basics, common conditions, help-seeking strategies, and stigma reduction.
For working professionals, privacy and flexibility are often top priorities when seeking mental health information and support. Here’s a simple checklist to guide your decisions:
Research highlights that engagement with digital mental health resources climbs when solutions can be adapted to busy schedules and ensure confidentiality8. This approach is ideal for employees who need discreet support without disrupting work routines. If maintaining workplace boundaries is key, prioritize telehealth programs with secure platforms and clear privacy policies.
Use this three-step guide to access confidential virtual mental health resources:
Digital mental health resources have made it easier than ever to find discreet support—studies show engagement rises when people can access care in ways that fit their schedules and privacy needs8. This method works when privacy is a top concern, such as for employees who want to keep support needs separate from their workplace.
To seamlessly fit mental health care into a working professional’s schedule, start with this practical planner:
Research shows that when care is flexible and can be integrated into daily routines, engagement with mental health information and digital support rises8. This approach is ideal for those balancing demanding jobs and personal responsibilities, as it allows for ongoing emotional wellness without major disruptions.
For families searching for mental health information and co-occurring disorder resources, a structured approach can ease the process. Begin with this quick checklist:
Studies reveal that engagement with mental health resources is higher when families can access current, comprehensive program details tailored to their loved one’s needs8. This path makes sense for caregivers who need to compare multiple treatment centers or virtual care options for a family member.
Use this four-point checklist to evaluate whether a treatment program offers truly comprehensive mental health information:
Industry experts emphasize that families are more likely to engage with programs that present transparent, up-to-date integrated treatment information and openly discuss both mental health and substance use support8. This approach works best when families compare programs using these criteria—helping them avoid fragmented or outdated resources.
Staying informed about telehealth policy changes is essential for families comparing treatment options for substance use and co-occurring mental health conditions. Start with this quick reference tool:
Under updated federal rules, home-based telehealth continues for substance use disorder and co-occurring mental health care, but some services will require an in-person visit every 12 months after an initial six-month window7. This approach works best for families in rural areas or those needing flexible access to integrated treatment information.
Taking action starts with a single commitment. The next 30 days can set the foundation for meaningful change in how you understand mental health and support those navigating these challenges.

During week one, focus on assessment and foundation-building. Identify your current knowledge gaps about mental health conditions, treatment approaches, and support systems. Choose 2-3 reliable educational resources—these might include reputable mental health organizations, evidence-based websites, or educational platforms. Document what you already understand well and which areas need deeper exploration.
Week two shifts to active learning. Engage with foundational content through articles, videos, podcasts, or online courses that address your identified knowledge gaps. Focus on understanding the basics: how different conditions manifest, what evidence-based treatments exist, and how the mental health system functions. This week builds the core knowledge that informs everything else.
In week three, deepen your understanding through interactive learning. Attend webinars or virtual workshops on mental health topics. Join discussion groups or online communities where people share experiences and insights. Consider informational interviews with mental health professionals or advocates. Interactive learning transforms abstract concepts into practical understanding you can apply in real situations.
Week four centers on application and integration. Put your knowledge into practice by having informed conversations about mental health, recognizing early warning signs in yourself or others, or offering more effective support to someone in your life. Reflect on how your increased literacy changes your perspective and interactions. Identify which areas warrant continued learning.
Start your first two weeks with a focused checklist:
Studies reveal that a stepwise, manageable approach helps reduce overwhelm and increases engagement with digital mental health resources8. This method works when you want to build a foundation of reliable knowledge before moving to action. LSI keywords such as evidence-based resources and integrated care information become especially important as you verify each source’s credibility.
To build your trusted source library, use this step-by-step checklist:
Research shows that individuals are more likely to act on information from sources they consider credible and accessible8. This approach is ideal for anyone who wants to avoid digital over-literacy by limiting their library to three to five high-quality references.
To clearly document your specific needs, set aside 10-15 minutes to answer these three guiding questions:
Writing down these points helps organize your search and makes it easier to communicate your needs when reaching out for support. Studies reveal that people who define their information needs early engage more effectively with evidence-based resources and avoid digital over-literacy8.
Weeks 3 and 4 center on putting your mental health information into practice with actionable steps. Start by using a daily or weekly checklist:

This strategy suits individuals and families who are ready to move beyond research and begin engaging with integrated care resources. Research highlights that people are more likely to follow through with support when mental health resources are accessed in manageable, stepwise increments that fit their routines8.
To connect with appropriate resources, use this practical action checklist:
Studies show that people are more likely to act on integrated care information when they have a clear, manageable next step and feel confident in the resource’s credibility8. This strategy suits those seeking support for both substance use and mental health conditions, especially when virtual options make care more accessible.
To start your recovery journey remotely, use this action checklist:
1. Set a specific date to attend your first telehealth session. 2. Prepare a short list of questions (symptoms, integrated treatment options). 3. Plan to follow up with your chosen provider at regular intervals.Digital mental health resources and telehealth have made it possible to begin recovery from home, reducing geographic and scheduling barriers and making support for both substance use and mental health conditions more accessible8. This method works when you need flexibility and privacy, or if you live in Vermont, Massachusetts, Connecticut, or New Hampshire, where Pathfinder provides virtual support.
Mental health literacy transforms from abstract knowledge into tangible impact when it shapes real-world decisions and interactions. Understanding the science behind mental health conditions, recognizing evidence-based treatment approaches, and learning to identify warning signs creates a foundation that empowers individuals to navigate their own mental health journeys and support others more effectively.
This knowledge translates into meaningful change in countless everyday situations. When someone understands that medication and therapy often work best together, they can advocate for comprehensive treatment rather than accepting a one-dimensional approach. Recognizing that irritability and sleep changes can signal depression helps people identify concerning patterns in loved ones before a crisis develops. Understanding that recovery isn't linear prepares individuals to view setbacks as part of the process rather than as failures, building resilience during challenging moments.
Mental health literacy also strengthens the critical conversations that shape treatment outcomes. Informed individuals ask better questions during appointments, understand when to seek second opinions, and recognize red flags in treatment recommendations. They can distinguish between normal adjustment periods and concerning side effects, communicate symptoms more precisely to healthcare providers, and make decisions aligned with evidence rather than misconceptions. This knowledge reduces the power imbalance that often exists in clinical settings, enabling more collaborative and effective care relationships.
Beyond personal application, mental health literacy ripples outward to create more supportive communities. When people understand that mental health conditions are medical issues rather than character flaws, stigma loses its grip. Informed individuals become better friends, family members, and colleagues—recognizing when someone needs support, offering appropriate help, and creating environments where people feel safe discussing their struggles. Knowledge doesn't solve every challenge, but it provides the foundation upon which meaningful change, informed decisions, and genuine support are built.
To judge if online mental health information is trustworthy, start with four key checks: 1) Make sure the source is a recognized organization, such as the National Institute of Mental Health or SAMHSA, rather than a personal blog or unverified social media account. 2) Confirm that the content is current—look for a recent publication or review date within the last two years. 3) Check for references to evidence-based research or clinical guidelines, which signal that the information is grounded in science. 4) Look for clear author credentials; reliable mental health resources are typically written or reviewed by licensed professionals4. If the site uses sensational language or makes big promises without proof, it’s wise to be cautious.
If you’re feeling overwhelmed by the sheer amount of mental health information online, you’re not alone. Studies reveal that excess digital content can actually increase confusion and anxiety, leading to something known as digital mental health over-literacy—a state where too much information blurs clarity rather than providing support9. Start by limiting your daily intake: pick just two or three evidence-based resources and set a specific time window for checking them. Consider this route if you notice scrolling through forums or social media makes you more anxious or uncertain.
Yes, virtual treatment can be just as effective as in-person care for co-occurring substance use and mental health conditions—when certain factors are in place. Recent research shows that digital mental health resources, including telehealth sessions, lead to strong engagement and outcomes if professional guidance is provided and treatment is tailored to co-occurring disorders8. This approach suits people who need flexibility, privacy, or live in rural areas where traveling for appointments is difficult. For those in Vermont, Massachusetts, Connecticut, and New Hampshire, virtual providers like Pathfinder make it easier to access coordinated, high-quality care from home.
It can be difficult to know whether you need support for substance use, mental health, or both—especially since symptoms often overlap. A practical approach is to look for patterns: if you notice ongoing sadness, anxiety, or trouble functioning that happens alongside substance use, or if one issue seems to make the other worse, integrated care might be right for you. Research shows that over 60% of adolescents in substance use treatment also have another mental health condition, highlighting how common co-occurring disorders are5.
Seeking mental health information or treatment is protected by privacy laws, and most employers cannot access your health records or know you are receiving support unless you choose to share it. Research shows that fear of stigma or negative job impact is a common barrier, but federal laws like the Americans with Disabilities Act (ADA) and the Health Insurance Portability and Accountability Act (HIPAA) safeguard your confidentiality2. This approach is ideal for working professionals who want to prioritize well-being while maintaining their career trajectory.
Telehealth policy changes coming in October 2025 will affect how people access virtual mental health care, especially for those with substance use and co-occurring mental health conditions. Under new federal rules, home-based telehealth services will continue for individuals seeking treatment for substance use disorder and co-occurring mental health conditions, as well as for general behavioral health services. However, to maintain ongoing virtual care, patients must have at least one in-person visit with their provider within six months of starting telehealth and then once every 12 months after that7.
Supporting a family member who isn’t ready to seek information or treatment for substance use can be challenging, but there are still meaningful steps you can take. Start by focusing on open, nonjudgmental conversations—let your loved one know you’re available to listen and help whenever they’re ready. Research shows that stigma and fear of being judged are leading reasons people avoid mental health information and support, so prioritizing empathy and patience can make a real difference2.
Mental health literacy and having a mental health diagnosis are two very different things. Mental health literacy refers to your ability to recognize symptoms, understand risk factors, know where to find reliable mental health information, and feel confident using resources or seeking help when needed. This knowledge empowers people to make informed choices and reduce stigma—regardless of whether they have a diagnosed condition1. In contrast, a mental health diagnosis is a formal evaluation by a qualified professional confirming the presence of a specific mental health disorder.
Mental health apps and AI tools can be helpful for self-assessment, but their safety and reliability vary widely. Research shows that digital mental health resources are most effective when used as a supplement to evidence-based care and with some form of professional guidance8. While many apps offer screening tools or mood trackers, not all are reviewed by licensed professionals or based on current clinical guidelines. This approach is ideal if you use apps to track symptoms or gather mental health information, but you should avoid relying on them for diagnosis or treatment decisions.
Many people with substance use disorders do not receive treatment due to a mix of stigma, lack of accessible mental health information, and fragmented care systems. Research shows that in 2024, about 80% of individuals needing substance use disorder treatment did not get it, and 41.2% of adults with both substance use and mental health conditions received no care for either10. Stigma remains a powerful barrier—worries about being judged or facing discrimination often prevent people from seeking help or even looking for integrated treatment information2.
Pathfinder does not offer primary mental health care as a standalone service. Instead, Pathfinder specializes in supporting people with co-occurring needs—providing integrated care for substance use disorders (SUD) alongside mental health treatment. This approach is ideal for individuals who are experiencing both substance use and mental health concerns, as research shows integrated treatment information leads to better outcomes for co-occurring conditions5.
The time it takes to move from researching treatment options to actually starting care for substance use and co-occurring mental health conditions can vary. On average, individuals who use a focused plan—such as building a trusted source list, clarifying their needs, and reaching out to a virtual provider—often progress from research to their first appointment in two to four weeks. Studies reveal that digital mental health resources and telehealth platforms increase speed and access, especially when people are guided by evidence-based mental health information and integrated care information8.
Pathfinder currently offers virtual mental health and substance use disorder treatment for individuals residing in Vermont, Massachusetts, Connecticut, and New Hampshire. These states are fully supported through telehealth, allowing people in recovery to access integrated care for co-occurring substance use and mental health needs from the convenience and privacy of home.
Reducing the stigma you feel about seeking mental health information starts with self-compassion and small, intentional steps. Research shows that stigma—whether internal (self-stigma) or external (fear of others’ judgment)—is a major reason why more than half of people living with mental health conditions avoid reaching out for support2. To counter this, try reframing your perspective: remind yourself that seeking mental health resources is a sign of strength, not weakness, and that mental health is just as important as physical health.

November 6, 2025

June 16, 2025

November 6, 2025