
Therapist Near Me That Accept Medicaid: Virtual Care That Breaks Barriers and Builds Futures
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Many people wonder why methadone can't be prescribed through telehealth when other medications for opioid use disorder can be accessed remotely. The answer lies in methadone telehealth restrictions, which operate under a distinct regulatory framework because of the medication's unique pharmacological profile and historical context.
Unlike buprenorphine or naltrexone, methadone is a full opioid agonist with a 24-36 hour half-life that accumulates in the body over 3-5 days of daily dosing. This means it carries both significant therapeutic benefits and potential risks when not properly monitored. The medication requires precise dosing adjustments based on individual metabolism.
"What seems safe on day one or two may become dangerous by day four or five without clinical oversight due to methadone's gradual accumulation in the body."
Federal regulations require methadone for opioid dependency to be dispensed through specially certified Opioid Treatment Programs, commonly known as methadone clinics. These programs must provide observed dosing, particularly during the stabilization phase when patients are most vulnerable to complications. This structure exists because methadone-related overdoses historically occurred when the medication was diverted or used without appropriate medical supervision.
The face-to-face requirement also serves a clinical purpose beyond safety monitoring. Methadone treatment works best within a comprehensive care model that includes counseling, medical evaluation, and regular check-ins that assess both progress and potential complications. The daily or frequent clinic visits create natural touchpoints for providers to identify warning signs, adjust treatment plans, and ensure individuals receive the full spectrum of support needed for sustainable recovery.
Responsible telehealth providers recognize these protective boundaries and work within them rather than around them. While telehealth has expanded access to medications like buprenorphine that allow for safe remote prescribing, methadone's regulatory structure reflects decades of clinical experience showing that certain medications require hands-on oversight.
Methadone’s unique chemistry—its variable metabolism, potential for overdose, and heart risks—calls for extra monitoring. Methadone’s effects on the body can differ greatly from person to person, so careful oversight is required.
Its narrow therapeutic window means that a small change in dose can make the difference between a helpful effect and a dangerous one, especially for heart rhythm problems6, 2.
| Feature | Methadone | Buprenorphine |
|---|---|---|
| Telehealth Eligibility | Restricted (Hybrid/OTP only) | Fully Permitted |
| Overdose Risk | Higher (No ceiling effect) | Lower (Ceiling effect) |
| Dispensing Location | Certified OTP Clinic | Local Pharmacy |
Unlike most medications, methadone’s half-life—the time it takes for half of the drug to leave the body—can range from as little as 8 hours to as much as 59 hours depending on the person2. This unpredictability means methadone can build up in the body and cause overdose if not carefully monitored.
Because of this, clinicians must see patients frequently, especially when starting or adjusting doses, making fully remote prescribing risky for this medication.
The narrow therapeutic index—the slim gap between a safe and a toxic dose—makes even minor errors risky6, 2. Methadone can also prolong the QT interval on an EKG, raising the risk of a dangerous heart rhythm known as torsades de pointes.
Research shows that when the QTc interval reaches 500 milliseconds or more, the risk of sudden cardiac death jumps fourfold6. These cardiac dangers are a major reason for methadone telehealth restrictions and for requiring in-person EKGs during treatment.
Federal certification demands that OTPs meet strict standards for medication storage, dosing, staff training, and patient monitoring to reduce diversion and serious health risks8, 4. By enforcing these protocols, the system supports safe, supervised methadone treatment—even as telehealth options expand.
OTPs must meet federal certification standards for medication storage, staffing, monitoring, and diversion control—requirements not imposed on standard clinics8, 4. This structure ensures rigorous oversight for medications with higher risks of misuse and overdose.
In contrast, office-based care allows more flexibility and virtual prescribing, but is typically reserved for medications like buprenorphine with a wider safety margin. Terms such as 'federally certified' and 'diversion control' highlight why OTPs remain central for methadone, while office-based telehealth is more common for other MAT medications.
Studies reveal that integrated treatment combining medications for opioid use disorder with behavioral health support leads to better outcomes and lower relapse rates9. This comprehensive approach is a key reason why methadone telehealth restrictions remain stricter than for medications like buprenorphine.
Services typically mandated at an OTP include:
Given methadone's unique federal requirements, the question becomes: how did regulators respond to these constraints when the pandemic demanded greater treatment flexibility? The 2024 regulatory landscape provides a clear answer, one that expanded access for some medications while maintaining methadone's distinct pathway.
The Consolidated Appropriations Act of 2023 (enacted December 29, 2022, with provisions effective through 2024) extended telehealth flexibilities for buprenorphine and other medications, allowing providers to prescribe these treatments after virtual consultations without requiring a face-to-face visit. This represented a significant shift in how medication-assisted treatment could be delivered.
However, methadone remained subject to stricter oversight under SAMHSA regulations codified in 42 CFR Part 8. The regulations require that individuals receiving methadone for opioid dependency must still obtain their medication from certified Opioid Treatment Programs. While SAMHSA guidance issued in March 2024 clarified provisions allowing for take-home doses under specific circumstances—particularly for stable patients—the initial assessment and ongoing monitoring standards remain more rigorous than for other medications used in recovery.
The 2024 rule change made telehealth options for methadone treatment a permanent part of Opioid Treatment Programs (OTPs). Previously, strict federal regulations meant most patient visits had to happen in person—now, OTPs in Vermont, Massachusetts, Connecticut, and New Hampshire can use secure video calls for key steps in care1.
Thanks to the 2024 SAMHSA rule, Opioid Treatment Programs (OTPs) can now conduct initial evaluations for methadone through secure video calls, giving people in Vermont, Massachusetts, Connecticut, and New Hampshire more flexibility in starting treatment1.
Ongoing counseling and medical check-ins can also be managed virtually, reducing transportation barriers. However, certain steps—like urine drug screens or EKGs for cardiac safety—often still require clinic visits, maintaining appropriate oversight for methadone’s risks.
The latest update allows Opioid Treatment Programs (OTPs) to give up to 14 days of take-home methadone to less stable patients and up to 28 days for those considered stable, based on the provider’s judgment—not just rigid timelines1.
This policy shift helps reduce travel and work disruptions, especially for people living far from clinics. Still, methadone telehealth restrictions ensure that decisions about take-home doses are guided by careful clinical review, ongoing monitoring, and periodic in-person visits to prevent misuse.
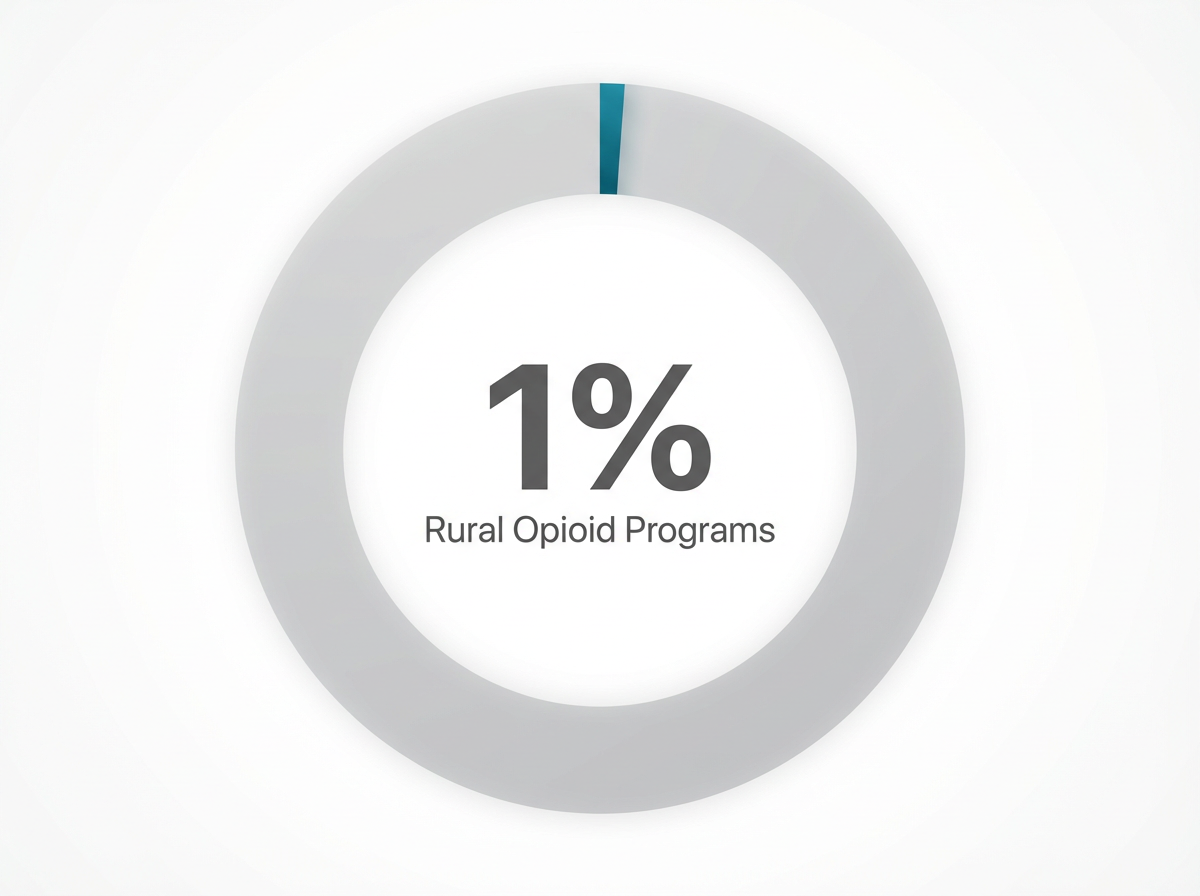
Less than 1% of Opioid Treatment Programs (OTPs) are located in rural areas, making in-person care a major challenge for many people3, 7. The latest regulations now allow mobile OTP units to bring medication and support directly to areas with limited resources, helping to overcome some of the longstanding barriers created by methadone telehealth restrictions.
This shortage means that patients in rural Vermont, Massachusetts, Connecticut, and New Hampshire often travel hours for in-person care. Mobile OTP units, now authorized under the 2024 SAMHSA rule, bring medication and essential services directly to outlying regions. These mobile clinics help address what industry leaders call a 'critical access gap' for rural populations.
The 2024 SAMHSA rule explicitly calls for person-first language in all communications and care settings, reflecting research that shows stigma can be a major barrier to treatment engagement and retention1.
Instead of labeling individuals by their condition, providers are encouraged to use terms like "person with opioid use disorder" or "person receiving methadone treatment," which supports dignity and recovery. Common phrases like "integrated care" and "stigma reduction" are now central to methadone telehealth restrictions, as these efforts go hand-in-hand with expanding geographic access.
While 2024 regulations expanded some flexibilities, they left unresolved fundamental barriers that continue to prevent many people from receiving timely treatment. Geographic limitations remain particularly challenging in rural areas, where patients travel an average of 40 miles to reach the nearest opioid treatment program—compared to 5 miles in urban settings.
The requirement for on-site visits at opioid treatment programs creates a substantial burden for people already managing the complexities of recovery. Daily clinic visits for methadone administration can conflict with employment, making it difficult for individuals to maintain jobs while pursuing treatment. This structural barrier disproportionately affects lower-income communities, where flexible work arrangements are less common and job security may prove more fragile.
These equity concerns expose a genuine tension at the heart of addiction treatment policy: regulations protecting patient safety exist for important clinical reasons, yet they can inadvertently create hardships for the very people they aim to help. The methadone dispensing requirements that prevent diversion also force working parents to choose between treatment and employment.
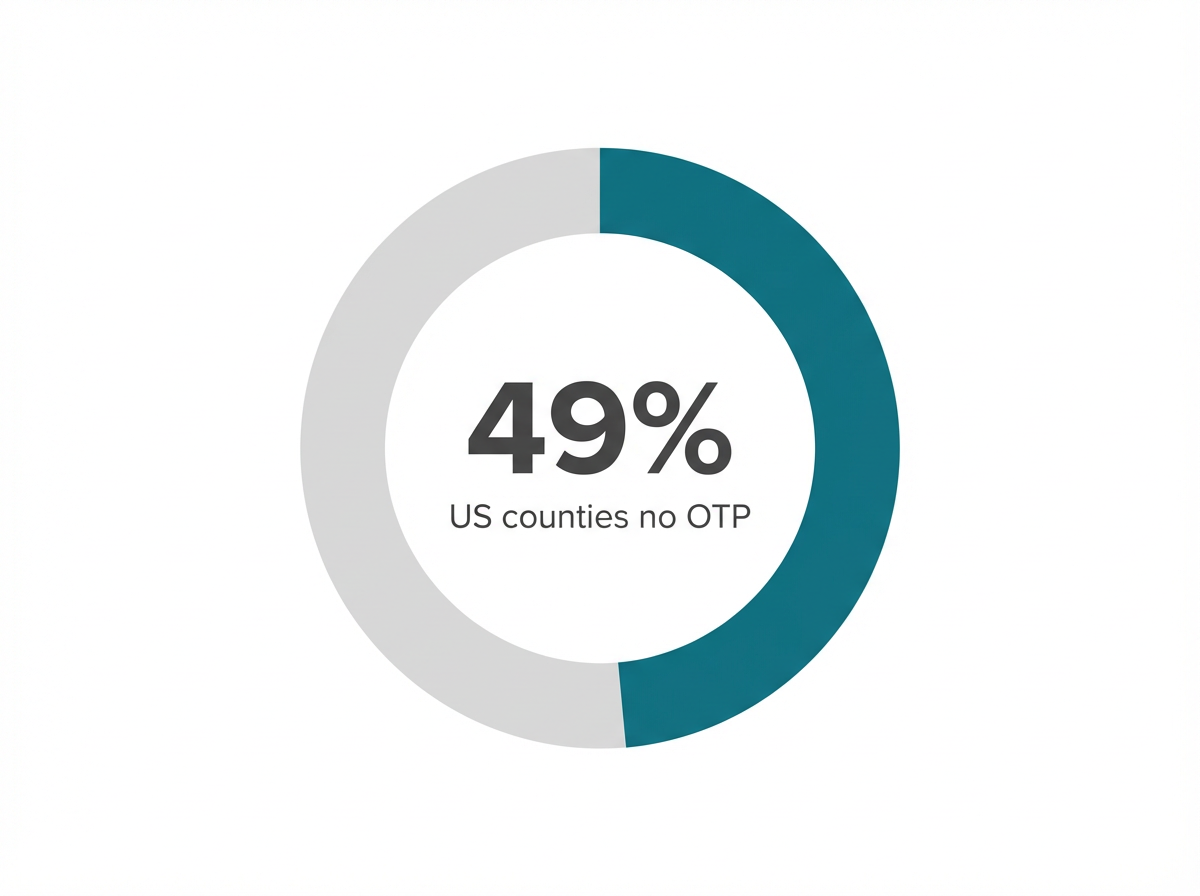
Research shows that 49% of US counties do not have an Opioid Treatment Program (OTP) that accepts Medicaid, and fewer than 1% of OTPs are found in rural areas3, 7. These insurance and geographic disparities mean that many people—especially those living in Vermont, Massachusetts, Connecticut, and New Hampshire—face travel burdens, out-of-pocket costs, or outright lack of access.
Studies reveal that 49% of counties do not have a Medicaid-accepting OTP, which means that even with updated methadone telehealth restrictions, people without private insurance may face travel, waitlists, or high out-of-pocket costs3.
If someone in Vermont, Massachusetts, Connecticut, or New Hampshire relies on Medicaid, their options for methadone treatment may be extremely limited. Terms like 'insurance barriers' and 'Medicaid exclusion' are frequently discussed alongside telemedicine policy changes because these financial hurdles persist regardless of new technology.
Data shows that fewer than 1% of OTPs nationwide are located in rural areas, leaving many people to travel long distances or face waitlists, even with updated methadone telehealth restrictions7. Terms like 'geographic disparities' and 'OTP shortages' are common when discussing these gaps.
Studies reveal that, among people for whom both medications are equally appropriate, Black and Hispanic individuals are more likely to receive methadone, whereas buprenorphine is disproportionately provided to white patients10. This creates what many experts call a “two-tiered MAT system,” where telehealth access and flexibility depend not only on clinical need but also on race and location.
Black and Hispanic patients are more likely to be offered methadone—requiring regular clinic visits—while buprenorphine is more often provided to white patients, who benefit from flexible telehealth and pharmacy options10. This split means that telemedicine access and medication choice can depend as much on race and geography as on clinical need.
The idea behind pharmacy-based dispensing is to allow community pharmacies—not just specialized Opioid Treatment Programs (OTPs)—to distribute methadone for opioid use disorder. Supporters argue that this model could close gaps caused by access barriers, especially in rural and minority communities, and help move beyond the current two-tiered MAT system10.
MOTAA is a recent legislative proposal aiming to pilot pharmacy-based methadone for opioid use disorder, while maintaining core safety requirements and clinical oversight10. This proposal reflects ongoing efforts to modernize methadone telehealth restrictions and promote greater equity in medication access.
When someone contacts a telehealth provider seeking methadone treatment, the initial conversation typically follows a structured assessment protocol. The intake specialist conducts a preliminary screening to understand the person's substance use history, current opioid dependence, previous treatment attempts, and immediate safety concerns.

Based on this assessment, the provider explains available pathways—which often means directing the individual toward certified opioid treatment programs (OTPs) for methadone while offering immediate support through counseling and care coordination services.
In practice, virtual providers navigate these boundaries through hybrid care models that combine remote and in-person elements. A typical workflow might include:
Responsible telehealth providers design their services around what proves safe and effective in a remote format—focusing on medications like buprenorphine for direct prescribing while building partnerships with OTPs for patients who need methadone. They deliver counseling, peer support, care coordination, and treatment for co-occurring mental health conditions, all critical components of comprehensive recovery support.
Buprenorphine’s safety profile—especially its lower risk of overdose and milder withdrawal symptoms—means it can be prescribed through telehealth without the same in-person requirements that methadone demands2. Industry leaders find that buprenorphine’s ceiling effect (which limits its potential for misuse) allows providers to deliver care via secure video visits, expanding access for people who might otherwise face travel or stigma barriers.
Buprenorphine’s ceiling effect means that after a certain dose, its effects level off, greatly reducing the risk of overdose compared to methadone2. This property, combined with its lower risk for serious heart problems, allows providers to safely prescribe and monitor buprenorphine through secure video visits.
Unlike methadone, which requires frequent in-person monitoring due to its variable metabolism and narrow therapeutic index, buprenorphine is designed for office-based and virtual treatment. Terms like 'ceiling effect,' 'remote prescribing,' and 'virtual MAT' all highlight why buprenorphine is the standard for telehealth-based care.
When methadone is indicated, telehealth providers in Vermont, Massachusetts, Connecticut, and New Hampshire cannot prescribe or manage methadone directly due to federal and state rules2, 8. Instead, they guide patients through timely referrals to certified OTPs, ensuring a smooth transition for in-person evaluation, medication initiation, and safety monitoring.
Throughout this journey, virtual teams continue to offer counseling, peer support, and help with co-occurring mental health needs—services that complement but do not replace OTP-based care. Terms like 'care coordination,' 'hybrid MAT model,' and 'referral pathways' highlight how providers work within prescribing limits while supporting recovery.
Pathfinder’s model centers on flexibility, safety, and whole-person support. Because federal rules prohibit fully remote methadone prescribing, Pathfinder focuses its virtual MAT program on buprenorphine—a medication proven effective and permitted for telehealth initiation2.
If a person’s needs call for methadone, Pathfinder coordinates a warm handoff to a local Opioid Treatment Program (OTP), ensuring that required in-person oversight is in place8. Throughout this process, Pathfinder’s team continues to offer virtual counseling, peer coaching, and support for co-occurring mental health needs alongside substance use disorder treatment.
Pathfinder’s hybrid MAT model connects individuals in Vermont, Massachusetts, Connecticut, and New Hampshire with consistent virtual touchpoints—including counseling sessions, peer coaching, and recovery check-ins. Research shows that ongoing virtual engagement can improve retention in treatment and lower relapse rates, especially when combined with medication and behavioral health support9.
While methadone telehealth restrictions require in-person oversight for certain medications, comprehensive virtual services still play a vital role in reducing isolation, building motivation, and helping people stick with their recovery plan.
Pathfinder’s approach recognizes that successful recovery often requires more than medication alone. By offering virtual counseling, access to psychiatric care for co-occurring mental health needs, and regular peer coaching, Pathfinder creates a supportive network for individuals in Vermont, Massachusetts, Connecticut, and New Hampshire.
Research shows that this kind of integrated treatment—combining medication with behavioral health support—improves outcomes and reduces relapse rates for people with substance use and mental health disorders9. Even as virtual prescribing limits for methadone remain, these wraparound services can be delivered remotely, helping people stay engaged between OTP visits and providing ongoing encouragement.
Choosing the right treatment path can feel overwhelming, especially when weighing clinical effectiveness against the practical realities of daily life. For those considering medication-assisted treatment, understanding how regulatory frameworks shape available options isn't just administrative detail—it's essential information that directly impacts which recovery supports will actually be accessible and sustainable over time.
Telehealth practitioners operate under the same federal and state regulations as traditional clinics, ensuring that care decisions prioritize patient safety over convenience. This means conducting thorough assessments, monitoring progress through regular check-ins, and adjusting treatment plans based on individual response. The goal is not simply to prescribe medication remotely, but to deliver comprehensive support that addresses the full spectrum of recovery needs.
For individuals seeking flexibility without compromising clinical rigor, buprenorphine-based telehealth programs can provide access to evidence-based treatment without the barriers of transportation, rigid scheduling, or geographic limitations. These programs combine medication management with counseling and support services, creating a coordinated approach that recognizes recovery as a multifaceted process.
The right path depends on where someone is in their recovery journey. Those requiring daily structure and intensive monitoring may benefit most from facility-based methadone programs. Others who have established stability, maintain employment, or need greater scheduling flexibility often find that remote buprenorphine treatment provides the balance they need. This is precisely why understanding methadone's regulatory boundaries matters: informed decisions require knowing not just what's clinically effective, but what's legally and logistically feasible.
People seeking medication-assisted treatment often have questions about how telehealth fits into their recovery journey. Understanding these specific concerns helps clarify what to expect from remote providers and how regulations shape treatment options across different situations.
No, current methadone telehealth restrictions do not allow you to start methadone treatment completely online without visiting a certified clinic. Federal law requires that methadone for opioid use disorder be dispensed only through federally certified Opioid Treatment Programs (OTPs), not regular clinics or fully remote platforms, due to methadone’s unique risks and the need for close supervision2, 8. While the 2024 rules now let OTPs use telehealth for the initial assessment and some ongoing care, you’ll still need at least one in-person visit to a clinic for medication pick-up, periodic monitoring, and safety checks.
If buprenorphine hasn’t worked for you in the past, you’re not alone—treatment response can vary from person to person. Sometimes, factors like co-occurring mental health needs, medication interactions, or the severity of opioid use disorder mean a different approach is needed. Under methadone telehealth restrictions, switching to methadone requires referral to a certified Opioid Treatment Program (OTP) for an in-person assessment and ongoing supervised care, since methadone can’t be prescribed fully online2, 8. Your provider will help you review your options and coordinate a smooth referral if methadone is clinically appropriate.
Yes, Pathfinder offers mental health support alongside medication treatment for substance use disorder through its integrated, virtual model. While Pathfinder does not provide primary mental healthcare, it does deliver co-occurring mental health services—such as counseling, peer coaching, and psychiatric care—alongside buprenorphine-based MAT or during coordination with Opioid Treatment Programs if methadone is needed. This approach aligns with research showing that combining medication with behavioral health support leads to better outcomes and long-term stability for people in recovery9.
Virtual treatment is designed to be highly private and confidential, often matching or even exceeding the privacy protections of in-person clinic visits. Secure telehealth platforms used by providers like Pathfinder must comply with HIPAA regulations, which safeguard your health information during video sessions, messaging, and record-keeping. Many people appreciate that telehealth reduces the risk of being recognized at a local clinic—an important consideration for those worried about stigma or unwanted disclosure.
Pathfinder currently provides virtual medication-assisted treatment (MAT) services to individuals in Vermont, Massachusetts, Connecticut, and New Hampshire. These states are supported through Pathfinder’s telehealth platform, which focuses on buprenorphine-based care and co-occurring mental health support alongside substance use disorder treatment. While methadone telehealth restrictions mean Pathfinder cannot initiate or manage methadone treatment remotely, the team offers referrals and ongoing support for those who may need in-person care at certified Opioid Treatment Programs (OTPs).
Yes, family members can often be involved in your virtual treatment plan if you wish. With your consent, virtual MAT providers like Pathfinder can include loved ones in counseling sessions, recovery planning, or educational meetings—helping build a supportive environment for your recovery. Research shows that family involvement can improve treatment engagement and contribute to better long-term outcomes, especially when combined with medication and behavioral health support9.
If you live in a rural area without an Opioid Treatment Program (OTP) nearby, your medication options may be limited by methadone telehealth restrictions. Only about 1% of OTPs are located in rural regions, making it difficult for many people to access in-person methadone treatment3, 7. However, recent rule changes allow initial assessments and some follow-up for methadone to happen by telehealth, and mobile OTP units can now bring medication and support services to underserved areas1. For many, buprenorphine is a more accessible option because it can be prescribed virtually and picked up at local pharmacies.
Pathfinder does not prescribe methadone through telehealth. Due to federal methadone telehealth restrictions, only certified Opioid Treatment Programs (OTPs) can initiate and dispense methadone for opioid use disorder, and this process requires at least some in-person visits for medication pick-up and monitoring2, 8. Pathfinder’s virtual services focus on buprenorphine, which can be safely prescribed online, while offering ongoing support and referrals to local OTPs if methadone is clinically appropriate.
Both buprenorphine and methadone are proven to help people achieve long-term recovery from opioid use disorder, but they differ in how they are administered and monitored. Buprenorphine can be prescribed and managed through telehealth or office-based care because its safety profile—especially its ceiling effect and lower overdose risk—makes it suitable for virtual treatment2. Methadone, on the other hand, must be dispensed through certified Opioid Treatment Programs (OTPs) due to its variable metabolism and higher risk for respiratory or cardiac complications.
Medicaid coverage for virtual medication-assisted treatment (MAT) through Pathfinder depends on whether your state’s Medicaid program contracts with virtual MAT providers and which services you need. In Vermont, Massachusetts, Connecticut, and New Hampshire, Medicaid often covers buprenorphine-based telehealth MAT, including counseling and peer support, but availability may vary by plan and region. However, nearly half of US counties lack an Opioid Treatment Program (OTP) that accepts Medicaid, which can limit access to methadone even as telehealth options expand3.
If your provider determines that methadone is a better fit than buprenorphine for your recovery, you’ll be referred to a certified Opioid Treatment Program (OTP) due to methadone telehealth restrictions. Only OTPs can legally start and dispense methadone for opioid use disorder, so you’ll need to complete an initial in-person visit at the clinic for evaluation, safety checks, and medication pick-up2, 8. Pathfinder and similar virtual MAT providers support you during this transition by coordinating referrals and continuing to offer counseling, peer support, and help with co-occurring mental health needs.
Yes, many people are able to work full-time while receiving virtual medication-assisted treatment (MAT), especially if they are prescribed buprenorphine, which can be managed through telehealth appointments and pharmacy pick-up. Virtual MAT offers flexible scheduling for counseling and check-ins, allowing you to fit treatment around your job and personal responsibilities. However, if you require methadone, some in-person clinic visits will still be necessary due to methadone telehealth restrictions and federal safety guidelines2.
If you’re taking buprenorphine through a virtual MAT provider, you’ll usually check in with your provider every one to four weeks, especially during the early stages of treatment. The exact schedule depends on your individual needs, your progress, and how your provider monitors things like medication response and overall well-being. Because buprenorphine can be prescribed and managed remotely thanks to its safety profile, virtual check-ins and telehealth appointments are often used instead of frequent in-person visits—unlike the stricter requirements set by methadone telehealth restrictions2.
Virtual medication-assisted treatment (MAT) can be highly effective for many individuals, especially when using buprenorphine, which is designed for remote prescribing and ongoing telehealth follow-up2. Research shows that outcomes like retention and relapse rates for telehealth MAT are similar to those seen in traditional in-person care when behavioral health support and regular monitoring are included9. However, methadone telehealth restrictions mean that people receiving methadone must still attend certified Opioid Treatment Programs (OTPs) for at least some in-person services due to safety oversight requirements.

November 6, 2025

November 7, 2025

November 6, 2025