
Does Abandonment Trauma Impact Addiction?
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Neurodivergent individuals—those with ADHD, autism, dyslexia, and other neurological differences—face distinct challenges when navigating substance use disorder recovery. Finding effective neurodivergent rehab is critical because research indicates that people living with attention-deficit/hyperactivity disorder are 2-3 times more likely to develop dependencies on alcohol or drugs compared to neurotypical individuals. Studies show that approximately 25% of adults seeking treatment for substance use disorders have ADHD.
Many use these substances to self-medicate symptoms like restlessness, impulsivity, or difficulty concentrating. Similarly, autistic individuals face elevated risks, with research suggesting rates of substance use disorders up to twice that of the general population, often linked to managing anxiety and sensory challenges.
"The goal isn't to force neurodivergent individuals into neurotypical frameworks, but rather to build pathways toward sobriety that work with their unique neurological wiring."
The intersection of neurodivergence and addiction creates a complex landscape. Traditional recovery programs typically follow a one-size-fits-all approach designed with neurotypical brains in mind. For someone with autism who struggles with sensory overload, a crowded group therapy session might be overwhelming rather than healing. For those managing ADHD symptoms, sitting still through lengthy lectures on recovery principles may prove nearly impossible, leading to feelings of failure before recovery even begins.
Understanding this foundation is crucial because neurodivergent brains process information, regulate emotions, and respond to stress differently. These differences aren't deficits—they're variations that require tailored approaches. When recovery programs acknowledge and adapt to these neurological differences, outcomes improve dramatically.
What you'll learn: This section unpacks the unique reasons neurodivergent adults—particularly those with autism or ADHD—are at greater risk for addiction. By the end, you'll recognize the core biological, psychological, and societal factors that raise these risks.
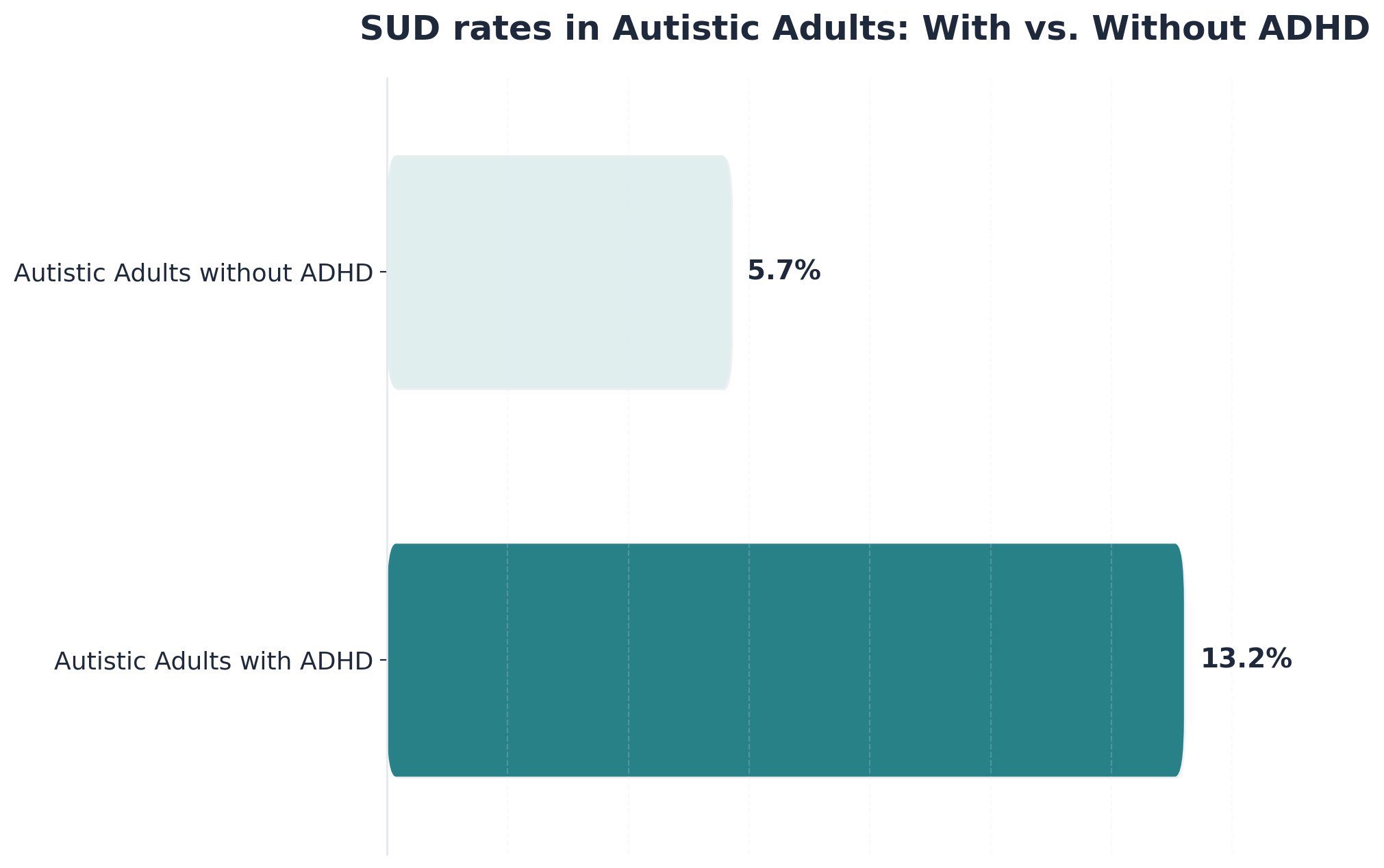
Addiction risk isn't just about willpower or choices. For neurodivergent adults, the odds are stacked higher due to a mix of brain-based differences and life experiences. Research finds that autistic adults with average or higher IQs are more than twice as likely to develop substance use disorders compared to non-autistic peers. The risk jumps even more when ADHD is present—13.2% of autistic adults with ADHD have SUD compared to just 5.7% without ADHD.1, 4
Why is this the case? It often comes down to three big issues:
Social exclusion and misunderstanding can add extra pressure, making the need for specialized support even clearer.
Practice This: Write a paragraph explaining to someone new to the topic why neurodivergent adults need addiction prevention strategies tailored to their needs. You're ready for the next level when you can list at least two reasons why standard addiction prevention doesn't always work for neurodivergent adults.
What you'll learn: This section explores how self-medication looks different for adults with ADHD and autism. By the end, you'll be able to identify common patterns and motivations behind substance use in these neurotypes.

Many neurodivergent adults turn to substances not just for recreation, but to manage daily struggles that others might not see. For example, studies reveal that autistic adults are nearly nine times more likely than non-autistic peers to use recreational drugs as a way to cope with sensory overload, manage anxiety, or quiet a busy mind.5 Those with ADHD may seek substances to boost focus or regulate mood when their brains feel scattered.
Unlike typical substance use patterns, self-medication among neurodivergent individuals often centers on finding relief from overwhelming internal experiences—whether that's calming constant sensory input, easing emotional distress, or gaining a sense of control.
Practice This: Think of a situation where you or someone you know used a strategy (healthy or not) to manage stress or discomfort. Write down what the trigger was and what helped most—then imagine how this might look different for someone with ADHD or autism. You're ready for the next level when you can describe at least one unique reason a neurodivergent person might use substances for self-medication.
Once you understand why neurotype-informed recovery matters, the next step is learning how to adapt standard approaches to match your brain's natural patterns. This means translating general principles into specific modifications you can implement immediately.
| Standard Approach | Neurodivergent Adaptation |
|---|---|
| 60-90 minute group meetings | 15-20 minute check-ins, 2-3 times weekly |
| Verbal instructions | Visual schedules and written action items |
| "Just do it" willpower | Body doubling and external accountability |
| Sitting still for focus | Movement breaks every 20-30 minutes |
For people who have ADHD, traditional long meetings may trigger restlessness and disengagement. Instead, try check-ins of 15-20 minutes rather than 60-90 minute sessions, scheduled two to three times weekly rather than once. Each meeting should end with 2-3 concrete action items written down immediately. Visual schedules—whether a color-coded calendar, a kanban board with "To Do/Doing/Done" columns, or even a simple whiteboard with the week's tasks—make abstract plans tangible.
Body doubling (working alongside another person, either in-person or via video call, even if you're doing different tasks) provides external accountability that helps initiate and sustain difficult recovery work. Movement breaks every 20-30 minutes prevent the restlessness that derails focus.
Autistic individuals frequently benefit from predictable routines and explicit communication about recovery expectations. Sensory considerations matter deeply—fluorescent-lit group rooms or crowded spaces can create unnecessary barriers. Written communication channels and advance notice about changes reduce anxiety and support consistent participation.
The most effective intermediate step involves honest self-assessment: What environmental factors help you focus? When do you experience overwhelm? Which communication styles feel most accessible? These answers inform personalized recovery plans that honor neurodivergent needs while building toward sustainable change.
What you'll learn: This section explores how therapy can be tailored to address the executive function challenges that are common among neurodivergent adults in recovery.
Readers might be wondering why sticking to a recovery plan can feel so difficult, even with strong motivation. Research shows that 30-80% of people living with substance use disorders experience lasting executive functioning difficulties—things like planning ahead, remembering steps, or shifting between tasks.8 For neurodivergent adults, these challenges can be even more pronounced, often turning standard therapy into an uphill climb.
One helpful analogy: Think of executive function as the 'air traffic controller' of the brain. When that controller is overworked or under-supported, it's easy for important tasks to get lost or delayed. Neurodivergent rehab programs address this by using tools like visual schedules, step-by-step checklists, and reminders. Therapists may break goals into smaller, bite-sized pieces, set up regular check-ins, and encourage self-monitoring with simple tracking sheets. These modifications not only reduce overwhelm, but also boost confidence as each small step is achieved.9
Practice This: Create a visual schedule for your week, using colors or symbols to mark therapy sessions, medication times, and daily routines. Notice which cues help you stay on track. You're ready for the next level when you can identify at least one tool or strategy that helps you follow through with recovery tasks—even on challenging days.
What you'll learn: In this section, you'll discover practical ways to create a sensory-friendly environment for virtual neurodivergent rehab.
Sensory needs are a big part of the recovery puzzle for neurodivergent adults, especially those with autism or ADHD. Bright lights, background noise, or even certain clothing textures can make it hard to pay attention or feel safe in virtual sessions. Research shows that autistic adults often use substances to cope with sensory overload, so addressing these needs directly in rehab is essential.5
Think of your virtual treatment space as a "sensory safe zone"—a place where you control the environment. Simple adaptations like dimming your screen, wearing noise-canceling headphones, or using a weighted blanket can help reduce distractions and anxiety. Some people find it helpful to keep fidget tools or calming objects nearby. Therapists in neurodivergent rehab often encourage clients to set up these supports before each session, checking in about sensory comfort as part of the routine.
Practice This: Pause and scan your space. List three things that make you feel calm (or uncomfortable) during a virtual appointment. Try adjusting one element before your next session and note any changes in your focus or mood. You're ready for the next level when you can identify at least one sensory strategy that helps you stay present and regulated during virtual recovery activities.
Once intermediate coping strategies become second nature, the next step involves translating these skills into your daily home environment—creating physical spaces and systems that naturally support recovery without requiring constant willpower. This advanced phase moves beyond individual coping strategies to establish systems that reinforce healthy patterns automatically.
The way you organize your living space significantly reduces decision fatigue during vulnerable moments. Individuals in recovery benefit from removing triggers from their immediate surroundings while adding visible reminders that prompt positive behaviors. This might include setting up a medication station directly beside your coffee maker so taking morning medications becomes part of your caffeine routine, placing recovery affirmations or meaningful quotes on your bathroom mirror where you'll see them daily, or keeping a gratitude journal on your nightstand with a pen already attached.
Consider reorganizing living spaces to facilitate morning routines, establishing a specific corner with a cushion and candle for mindfulness practices, or creating physical barriers between work and rest zones. Technology integration can strengthen accountability without adding burden. Medication management apps, recovery tracking tools, and scheduled check-ins with support networks create reliable external support during vulnerable moments. These systems work particularly well when customized to match personal neurotype—those who thrive on structure might benefit from detailed scheduling apps, while others may prefer simple reminder systems.
Building backup options into recovery plans ensures resilience during high-stress periods. For example, if your primary coping strategy is calling your sponsor but they're unavailable during a crisis, having a predetermined list might include:
This approach means identifying backup support contacts, maintaining multiple coping strategies for common triggers, and establishing clear protocols for when primary plans fail. The goal is creating a recovery ecosystem where no single point of failure can derail progress, allowing individuals to navigate challenges while maintaining forward momentum toward lasting wellness.
What you'll learn: This section breaks down how virtual detox can be made safer and more supportive for neurodivergent individuals.
Virtual detox means managing withdrawal at home, often with daily check-ins from a care team. For neurodivergent adults, safety depends on more than just physical health—it also means planning for sensory sensitivities and executive functioning needs. Studies show that home-based detox is safe and effective for most people, as long as there's a stable environment and frequent monitoring.7
In neurodivergent rehab, this can look like using clear step-by-step routines, visual reminders for medication, and regular video calls to check progress. Some programs help individuals set up a 'comfort zone' with sensory supports, like dim lighting or weighted blankets. These adaptations reduce overwhelm and help people stick with the process, especially if their brains are wired for routine or need extra structure.
Practice This: Make a list of three things you'd need in your space to feel safe and calm during a challenging week. Think about what helps you stay regulated—then note one way a friend or support person could help if things get tough. You're ready for the next level when you can describe one safety adaptation you'd request in a virtual detox plan tailored to your needs.
What you'll learn: This section explains how medication-assisted treatment (MAT) can be provided safely and effectively through telehealth for neurodivergent adults in recovery.
Medication-assisted treatment combines FDA-approved medications with counseling and behavioral therapies to support recovery from substance use disorder. For individuals in neurodivergent rehab, telehealth MAT offers extra flexibility: appointments, medication management, and follow-ups can happen from home, reducing the stress of travel, unfamiliar environments, or overwhelming clinics. This is especially helpful for those sensitive to sensory input or who need structured, predictable routines.
Recent updates from the HHS and DEA have formally extended telehealth prescribing flexibilities through 2026, making it easier for qualified providers to initiate and manage MAT remotely while maintaining safety standards.10
Practice This: Write down two ways virtual MAT could make recovery more manageable for you or someone you know (think: sensory comfort, easier scheduling, or more privacy). You're ready for the next level when you can describe one benefit of telehealth-based MAT that helps address a specific neurodivergent need.
Even with home systems in place, challenges arise. Individuals with neurodivergent conditions often encounter specific obstacles during recovery. Executive function challenges can make it difficult to remember appointments, follow through on treatment plans, or maintain consistent routines. These aren't failures of willpower—they're neurological differences that require adapted support systems. This is why the redundancy strategies and visual management tools discussed in Building Your Home System prove essential.
Sensory sensitivities frequently create barriers in traditional treatment settings. Fluorescent lighting, crowded group rooms, or unexpected sounds can trigger overwhelm that makes participation nearly impossible. When environments aren't designed with neurodivergent needs in mind, people may avoid seeking help altogether rather than endure sensory distress. The environmental modifications outlined in Advanced Applications—creating quiet spaces and controlling sensory input—directly address these accessibility needs.
Communication mismatches between providers and clients also derail progress. A person with autism spectrum disorder might interpret instructions literally, missing implied expectations. Those experiencing attention regulation challenges might struggle to process lengthy verbal directions without written reinforcement. These disconnects often get misread as non-compliance when they're actually accessibility issues. The communication frameworks and written reinforcement techniques from earlier sections help bridge these gaps.
Social anxiety and rejection sensitivity can prevent people from speaking up about what isn't working. Past experiences of being misunderstood or dismissed create hesitancy to advocate for needed accommodations. Building trust takes time, and recovery programs must create psychologically safe spaces where questions and feedback are genuinely welcomed. Use this script to advocate for yourself:
"I want to succeed in this program, but I'm having trouble processing verbal instructions. Could we try using a shared written checklist for my weekly goals instead?"Recognizing these patterns helps shift the focus from "fixing" the person to adapting the approach—a fundamental distinction that opens pathways to sustainable recovery. The following resources provide additional support for navigating these common barriers and implementing the strategies discussed throughout this guide.
What you'll learn: This section highlights why standard cognitive behavioral therapy (CBT) often misses the mark for autistic adults and how neurodivergent rehab adapts to meet these needs.
Standard CBT is built around talking through thoughts, emotions, and behaviors. But for autistic individuals, this style can feel confusing or even inaccessible. Studies reveal that autistic adults benefit most from therapy sessions that use more structure, clear language, and visual supports—like charts or step-by-step guides—because these adjustments match their communication and processing preferences.9
Imagine being given directions with lots of abstract language when you’re used to maps and checklists; it’s easy to get lost. When CBT is adapted—using concrete examples, visual aids, and repeated routines—autistic clients are more likely to understand, participate, and see lasting results.
Practice This: Write down one way you prefer to receive instructions (visual, written, spoken, or hands-on). Then, think of how modifying therapy in that style might help you or someone you know engage better in recovery. You're ready for the next level when you can spot at least one sign that a therapy approach isn’t fitting your needs and suggest a change—like asking for more visuals or clearer steps.
What you'll learn: This section uncovers how interoceptive support can help prevent relapse for neurodivergent adults—especially those who may struggle to notice or interpret internal body cues.
Interoception is our ability to sense what’s happening inside our bodies—like hunger, pain, or emotional shifts. For many neurodivergent people, especially autistic adults, interpreting these signals can be difficult. This means early warning signs of stress, cravings, or emotional overwhelm might go unnoticed until they become too strong to manage. Studies reveal that differences in interoceptive awareness and high rates of alexithymia (difficulty identifying feelings) are linked to higher substance use, as individuals turn to substances to regulate or even create sensations and emotions they struggle to feel naturally.6
Neurodivergent rehab programs can help by including occupational therapy, body scan exercises, or simple emotion-mapping tools to build awareness of internal cues. These supports give people more chances to catch triggers early and use healthier coping strategies. Over time, growing interoceptive skills makes it easier to recognize when help is needed—reducing the risk of relapse.
Practice This: Try a daily body check-in. Pause for a minute and ask: Where do I feel tension or calm? What’s one word for how my body feels right now? Jot it down each day and look for patterns. You're ready for the next level when you can name one internal cue that signals stress or craving for you—and describe a step you’d take to address it.
Recovery from addiction looks different for neurodivergent individuals because our brains are wired differently—and that's exactly why adapted approaches matter. Throughout this article, we've explored how understanding your neurotype isn't just helpful; it's essential for building recovery strategies that actually stick.
The key takeaways are straightforward: First, understanding whether you have ADHD, autism, or other neurodivergent traits fundamentally changes which recovery tools will work for you. Second, adapting evidence-based strategies to match your brain's wiring—rather than forcing yourself into neurotypical frameworks—creates sustainable change instead of constant struggle. Third, building systems that work with your executive function, sensory needs, and processing style transforms recovery from an uphill battle into a manageable path forward.
Whether you're considering medication-assisted treatment, exploring abstinence-based recovery, or finding a middle path that works for your life, these neurodivergent-adapted principles can guide you toward approaches that honor how your brain actually functions.
If you're in Vermont, Massachusetts, Connecticut, or New Hampshire and seeking support for addiction, Pathfinder offers virtual treatment services that meet you where you are. The team provides evidence-based care for dependency issues, including support for co-occurring mental health conditions that may be part of your recovery journey.
Your recovery doesn't have to look like anyone else's. It just needs to work for your neurodivergent brain. Start by identifying one environmental adaptation from the Advanced Applications section to implement this week—that single change could be the foundation of your sustainable recovery journey.
Yes, traditional recovery programs can work for neurodivergent individuals—when properly adapted. Evidence shows that people with ADHD, autism, or other neurodivergent conditions achieve successful recovery outcomes when treatment addresses both their addiction challenges and their unique neurological needs. The key is finding programs that modify their approach rather than expecting neurodivergent participants to simply "fit in" to standard formats.
Medication-assisted treatment (MAT) is not only safe for neurodivergent individuals—it's often essential for successful recovery. When properly prescribed and monitored, MAT can address both substance dependence and co-occurring conditions simultaneously. Healthcare providers experienced in neurodivergent care can develop medication protocols that support recovery without compromising treatment for ADHD, autism, or related conditions.
Treatment duration for neurodivergent individuals is typically the same as standard programs—generally 30, 60, or 90 days for initial treatment, followed by ongoing support. However, the pacing may differ. Some neurodivergent individuals benefit from extended processing time, modified scheduling, or different session structures. The timeline should be individualized based on both recovery progress and neurological needs.
Research confirms that virtual addiction treatment produces comparable outcomes to in-person programs when properly structured. For many neurodivergent individuals, telehealth offers distinct advantages: reduced sensory overwhelm from travel and waiting rooms, the comfort of familiar environments, and greater schedule flexibility. The effectiveness depends on choosing providers who understand how to deliver adapted care through digital platforms.
Look for programs that explicitly offer co-occurring disorder treatment and have experience with neurodivergent populations. The most effective providers understand that different brains require different approaches—not lesser care, but tailored care. Ask potential programs specific questions about their experience with ADHD, autism, or your particular neurological profile, and how they modify their standard protocols to accommodate different processing styles and sensory needs.
Yes, Pathfinder virtually serves adults in recovery who live in Vermont, Massachusetts, Connecticut, and New Hampshire. Their programs are designed for individuals seeking support for substance use disorder (SUD) and co-occurring mental health needs. Because Pathfinder’s care is delivered entirely through telehealth, people across these four states can access neurodivergent rehab without the barriers of travel or in-person scheduling. This approach is especially helpful for those who may benefit from sensory-friendly environments or need flexible routines at home. Research shows that virtual, home-based treatment models improve access and comfort for neurodivergent adults—making it easier to get personalized support no matter where you live within these states.7
Yes, many individuals can continue taking ADHD medication while participating in substance use treatment—especially when care is provided through a neurodivergent rehab program that understands both conditions. Research shows that, among autistic adults with ADHD, those who receive prescribed ADHD medications generally have better overall health outcomes.4 In virtual rehab, providers work closely with clients and their prescribers to assess risks, monitor for misuse, and ensure medications are managed safely. Treatment plans are individualized: some people may need extra supervision or medication adjustments, but stopping ADHD medication suddenly can actually increase relapse risk by making focus and emotional regulation harder. If you have concerns about your prescription, talk openly with your provider—they’ll help you create a plan that supports both your recovery and ADHD needs.
If you have a co-occurring mental health condition alongside your substance use disorder, Pathfinder’s virtual neurodivergent rehab programs are designed to address both together. While Pathfinder does not provide primary mental healthcare, their care teams understand how depression, anxiety, and other mental health concerns can interact with substance use—especially in neurodivergent individuals. Treatment plans are adapted to account for overlapping symptoms, unique sensory needs, and executive function challenges, helping you manage both diagnoses in a coordinated way. Research shows that adapting addiction care for co-occurring conditions and neurodivergence leads to better outcomes, with improved mood, reduced anxiety, and stronger recovery progress.9, 2 You’ll work with a team that can collaborate with your outside mental health providers and tailor recovery tools to fit your specific challenges, ensuring your care is as integrated and supportive as possible.
Virtual neurodivergent rehab programs are designed with sensory sensitivities in mind—especially for those on the autism spectrum. Providers recognize that bright lights, background noise, or unexpected interruptions can trigger discomfort or overwhelm, so virtual sessions allow individuals to control their own environment for maximum comfort. This might include dimming the screen, wearing noise-canceling headphones, or using weighted blankets and fidget tools. Therapists routinely check in about sensory comfort and encourage adjustments before or during each session. Research shows that autistic adults often use substances to manage sensory overload, which makes sensory-friendly adaptations an essential part of effective virtual care.5 When treatment is tailored this way, it becomes easier to stay focused, reduce anxiety, and participate fully from home.
Your privacy is a top priority in virtual neurodivergent rehab programs. Unless you choose to share your participation, your employer or family will not be notified that you are receiving treatment. All care is protected by federal laws like HIPAA, which require your personal health information and treatment details to remain confidential. Appointments and messaging are handled through secure telehealth platforms, so only you and your care team have access to what is discussed or documented. Research shows that privacy protections are a key advantage of virtual, home-based treatment, making it easier for neurodivergent adults to seek help without fear of unintended disclosure.7 If you have specific concerns about privacy or documentation, your care team can walk you through what information remains private and help set boundaries that feel safe for you.
If you’ve tried traditional rehab before and experienced relapse, you’re not alone—and you’re likely wondering what’s different about neurodivergent rehab. Traditional programs often use a one-size-fits-all approach, which can miss the sensory, cognitive, and communication needs that matter most to neurodivergent adults. Instead, neurodivergent rehab is built to adapt: therapy sessions use visual aids, structured routines, and language that makes sense for autistic or ADHD minds. Care teams check in about sensory comfort, help break big goals into small steps, and offer flexibility that fits your daily life. Research shows that when treatment is tailored for neurodivergent needs, outcomes improve for both addiction and co-occurring conditions—meaning more people make meaningful progress and feel truly understood.9, 2
If traditional rehab felt overwhelming, confusing, or just didn’t seem to “get” you, this model is designed to help you finally feel seen and supported.
Yes, many neurodivergent-adapted programs include peer recovery coaches who have lived experience with both substance use and neurodivergence. These coaches offer unique support by sharing firsthand understanding of the challenges faced in recovery, making it easier for participants to feel seen and heard. Studies reveal that working with peer recovery coaches helps individuals feel more confident, reduces isolation, and provides practical, non-judgmental guidance—especially in virtual and home-based neurodivergent rehab settings.2 Peer support can be offered through virtual groups or one-on-one sessions, allowing for flexible and accessible connection from home. This kind of support is especially valued by neurodivergent adults who may have felt misunderstood in traditional care settings. If you’re interested in connecting with a peer recovery coach, ask your program about available options tailored for neurodivergent needs.

November 6, 2025

November 7, 2025

November 7, 2025