
Addiction Therapy Near Me: Accessible, Stigma-Free Therapy from Home with Pathfinder Recovery
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Medicaid serves as a vital resource for individuals seeking mental health and addiction treatment, providing comprehensive coverage that can make care accessible and affordable. Finding online therapy that takes medicaid is a crucial step for many in Vermont, Massachusetts, Connecticut, and New Hampshire who need flexible support. This guide will help you understand exactly what services are covered, how to verify your eligibility, and the practical steps to access the care you need—whether you're seeking therapy for depression, treatment for substance use disorder, or integrated care for both.
Under the Mental Health Parity and Addiction Equity Act, Medicaid plans must cover mental health and addiction services at the same level as medical and surgical benefits. This means that enrollees have access to a wide range of therapeutic services, including outpatient therapy, psychiatric evaluations, medication management, and in many cases, intensive outpatient programs. For example, individual therapy sessions that might cost $150-$200 out-of-pocket are typically covered with minimal or no copay under Medicaid.
Coverage specifics can vary by state, as each state administers its own Medicaid program within federal guidelines. Some states offer more extensive mental health and addiction benefits than others, and the types of providers covered may differ. Most Medicaid plans cover services from licensed therapists, psychiatrists, psychologists, and clinical social workers. Many states also cover telehealth services, which has expanded access significantly for people in rural areas or individuals with transportation challenges.
When mental health conditions exist alongside addiction—known as co-occurring disorders—Medicaid coverage becomes particularly important. Integrated treatment that addresses both conditions simultaneously has proven most effective for long-term recovery. Medicaid typically covers these coordinated care approaches, recognizing that mental health and addiction recovery are often interconnected.
Medicaid covers a broad range of mental health therapy services for eligible individuals, whether the care is provided in-person or through online therapy that takes medicaid. Covered services typically include individual, group, and family therapy delivered by licensed professionals. Most state Medicaid plans pay for evidence-based treatments like cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), and trauma-focused approaches8.
Medicaid also covers therapy for co-occurring substance use and mental health conditions, supporting individuals with complex needs. Copayment amounts and session limits vary by state, but many plans keep out-of-pocket costs low to reduce barriers for people seeking care9.
Medicaid covers a range of evidence-based therapy modalities for individuals who qualify. The most commonly approved approaches include:
Medicaid does not pay for alternative treatments such as acupuncture or life coaching, focusing instead on therapies that have strong scientific backing. Studies reveal that most state Medicaid plans also allow for individual, group, and family therapy sessions, giving people flexibility in how they receive care8.
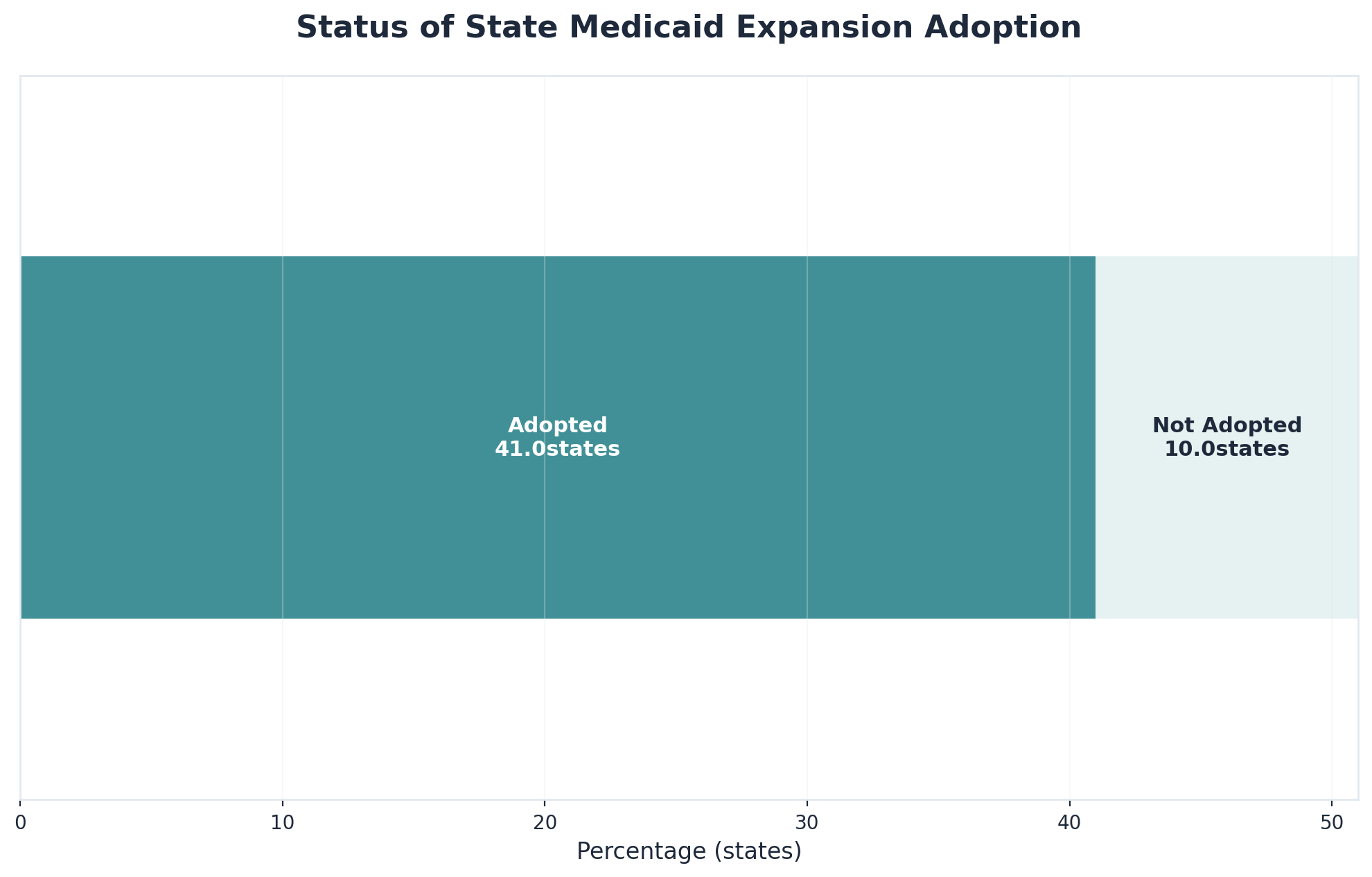
Medicaid therapy coverage looks different depending on where someone lives. Some states offer expanded Medicaid for adults with incomes up to 138% of the federal poverty level, while others have stricter eligibility rules7. Covered therapy services, session limits, and copayment amounts are set at the state level.
| State Medicaid Expansion | Typical Session Limit | Copayment Range |
|---|---|---|
| Expansion (VT, MA, CT) | 20-30/year | $0-$25/session |
| Non-Expansion (varies) | 10-20/year | $0-$4/session |
State budgets, local policies, and provider networks all play a role in shaping coverage8. Medicaid enrollees should check their state’s plan and talk to providers to confirm which telehealth mental health services are available.
Telehealth parity means that Medicaid must treat online therapy the same as in-person care. Over the past few years, most state Medicaid programs have adopted policies that reimburse online therapy at the same rate as face-to-face visits, which has made online therapy that takes medicaid widely available in Vermont, Massachusetts, Connecticut, and New Hampshire4.
"The number of mental health facilities offering telemedicine jumped from 38% to 68% in just one year, showing how quickly telehealth services became mainstream for Medicaid enrollees."4
Federal law sets the baseline for what Medicaid must offer regarding virtual mental health care. The Centers for Medicare & Medicaid Services (CMS) requires that all online therapy covered by Medicaid must meet the same standards as in-person care, both in quality and in privacy protections4. This means that online therapy that takes medicaid must be delivered by qualified, licensed professionals and use secure, HIPAA-compliant platforms.
When using online therapy that takes medicaid, most people can expect their out-of-pocket costs to be quite low. Medicaid sets strict limits on cost-sharing, so copayments for virtual mental health sessions usually range from $0 to $25 per session9.
| Cost-Sharing Element | Typical Range | Notes |
|---|---|---|
| Copayment per Session | $0 - $25 | Varies by state, often lower for children/pregnant individuals |
| Annual Session Limit | 10 - 30/year | State-specific; some allow exceptions |
| Deductibles | $0 | Medicaid plans rarely require a deductible |
Before beginning the search for psychiatric and addiction treatment services, confirming active Medicaid coverage is essential. Medicaid eligibility varies by state, and understanding current enrollment status helps avoid unexpected billing issues or service interruptions during treatment.
Most states provide multiple ways to verify coverage. The quickest method involves logging into the state's Medicaid member portal. Members without online access can call the member services number printed on their Medicaid card. Eligibility requirements differ significantly across states; income thresholds, household size calculations, and renewal processes vary depending on location.
To start your search for online therapy that takes medicaid, first confirm you are actively enrolled. Identify which type of Medicaid plan you have—such as managed care or fee-for-service—as this affects which virtual mental health providers you can see. Many states, including Vermont, Massachusetts, Connecticut, and New Hampshire, offer expanded Medicaid to adults with incomes up to 138% of the federal poverty level7.
Expansion states—like Vermont, Massachusetts, and Connecticut—have adopted the Affordable Care Act’s option to provide Medicaid to nearly all adults with incomes up to 138% of the Federal Poverty Level7. This broader eligibility helps more adults qualify for virtual mental health care. In contrast, non-expansion states set tighter rules, often covering only specific groups such as parents or people with disabilities.
Managed care organizations (MCOs) contract with states to provide Medicaid services through their own provider networks. If someone has a managed care plan, they’ll likely need to choose an in-network therapist for virtual mental health services to be covered. Fee-for-service (FFS) plans let individuals see any Medicaid-approved provider who accepts state insurance.
After confirming your Medicaid enrollment, review your plan's specific mental health benefits. Key areas to check include the number of therapy sessions allowed per year, whether you need prior authorization for virtual visits, and which therapy types are covered. Session limits usually fall between 10 and 30 per year8, 9.
Every Medicaid plan sets its own rules for how many online therapy sessions you can have each year. It’s common for plans in Vermont, Massachusetts, Connecticut, and New Hampshire to require your therapist to submit a brief request for more sessions if you reach the annual cap. This step helps ensure ongoing care, but it’s important to plan ahead so you don’t have a gap in support.
People who are enrolled in both Medicare and Medicaid—known as dual-eligible individuals—face some unique steps. In these cases, Medicare is usually the primary payer for covered health services, while Medicaid acts as the secondary payer to help cover costs like copayments. Dual-eligible individuals should check whether their online therapist is approved by both Medicare and Medicaid.
With eligibility confirmed, the search for the right provider begins. This process requires understanding which facilities and clinicians participate in the state's network, as out-of-network care may result in unexpected costs or claim denials.
Several resources streamline the provider search process. SAMHSA's national treatment locator (findtreatment.gov) offers a comprehensive database of facilities nationwide. Most state Medicaid programs also maintain their own online directories—such as Vermont's Green Mountain Care portal—where individuals can search by location, specialty, and accepted insurance plans.
Using your official Medicaid provider directory is a key step in finding online therapy that takes medicaid. Look for options to filter by service type, such as Telehealth or Virtual Therapy. Since about one-third of therapists don’t take insurance, using these search filters is essential3.
| Directory Feature | Why It Matters |
|---|---|
| Telehealth Filter | Narrows list to therapists offering online care |
| Insurance Accepted | Confirms Medicaid plan compatibility |
| Provider Status | Shows if provider is accepting new clients |
| Contact Information | Lets you reach out to confirm details |
State Medicaid websites and managed care organization (MCO) online databases are the most reliable starting points. Each state, including Vermont, Massachusetts, Connecticut, and New Hampshire, maintains its own official Medicaid portal. These websites usually offer searchable databases where individuals can look up mental health providers by location, specialty, and insurance accepted.
When searching for online therapy that takes medicaid, it’s helpful to use the filter tools in your provider directory to see only telehealth-enabled practitioners. By enabling filters like Virtual Visits, you can easily narrow the list to therapists who actually provide remote counseling.
Once you have a shortlist of therapists, contact providers directly for up-to-date verification. Ask if the provider is actively accepting Medicaid for telehealth sessions and if there are any restrictions based on your specific plan or location. Direct contact gives you a chance to confirm details like provider availability, session formats, and what to expect with scheduling or paperwork.
When reaching out to a provider, it helps to have a list of clear, focused questions. Important questions include:
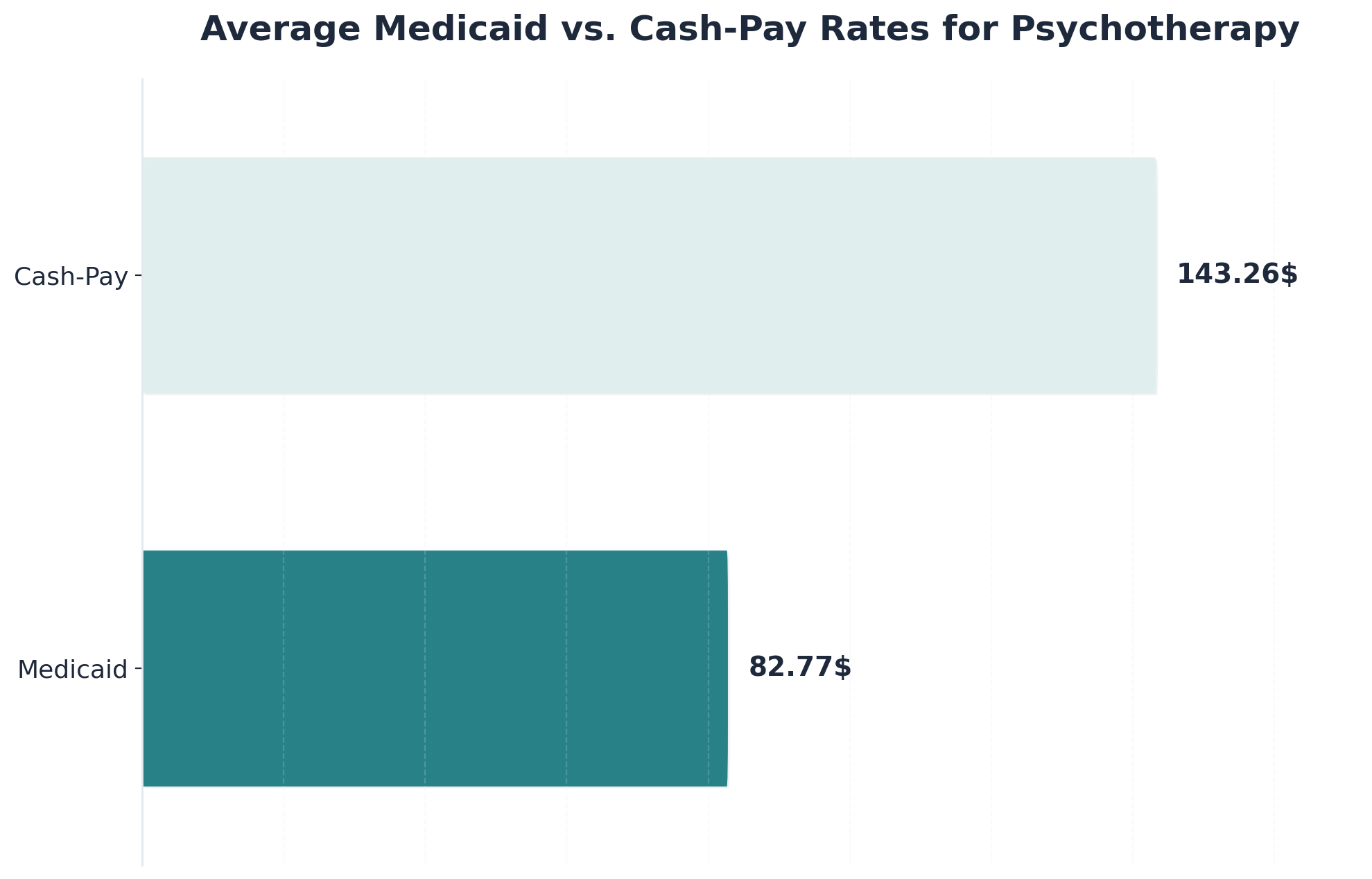
Understanding why some therapists do not accept online therapy clients with Medicaid often comes down to provider reimbursement gaps. Medicaid typically reimburses therapists about 40% less than what they would earn from cash-pay clients3. This large difference means some providers, especially those in private practice, may choose not to join Medicaid networks.
Finding an in-network provider is only half the battle—several practical obstacles often emerge between initial contact and actually beginning treatment. Understanding these barriers beforehand helps create strategies to overcome them.
Wait times represent the most common challenge. Many quality providers have waitlists extending weeks or months. When contacting providers, ask about current availability and request to be placed on cancellation lists. Transportation poses another significant barrier, particularly in rural areas. Telehealth has expanded access considerably, with many providers now offering virtual appointments through platforms like Doxy.me or SimplePractice that eliminate travel requirements entirely.
Finding online therapy that takes medicaid can be tough in areas with provider shortages. Strategies that help include seeking out master's-level clinicians, community health centers, or organizations specializing in co-occurring mental health and substance use support. Using telehealth provider directories and reaching out to clinics directly can also increase the chances of finding virtual counseling that accepts Medicaid.
Many therapists choose not to participate in Medicaid due to financial and administrative reasons. Research shows that Medicaid typically reimburses therapists significantly less than private pay rates. Along with lower payments, providers also face extra paperwork and longer wait times for approval of claims.
| Payment Type | Average Reimbursement (per session) | Typical Paperwork Burden |
|---|---|---|
| Medicaid | $82.77 | High |
| Cash-Pay | $143.26 | Low |
Expanding your options to include alternative provider types can make a real difference. Many master's-level therapists—such as licensed clinical social workers (LCSWs) and licensed mental health counselors (LMHCs)—are more likely to accept Medicaid than doctoral-level psychologists3.
| Provider Type | Medicaid Acceptance | Typical Services Offered |
|---|---|---|
| Master's-Level Clinicians | High | Individual, family, group therapy |
| Community Mental Health Center | High | Behavioral health, crisis support |
| Telehealth Clinics | Moderate-High | Virtual therapy, co-occurring care |
The Mental Health Parity and Addiction Equity Act (MHPAEA) requires Medicaid plans to cover mental health and substance use disorder services on equal footing with medical or surgical benefits5. This means Medicaid cannot set stricter limits on therapy visits, higher copayments, or extra approval steps for behavioral health care compared to other covered health services.
MHPAEA ensures that limits on therapy visits or approval steps for behavioral health care can’t be stricter than what’s required for other types of medical care. For example, if your Medicaid plan allows unlimited doctor visits but caps therapy sessions at 12 per year, that could be a parity violation.
If coverage for online therapy that takes medicaid is denied, you have the right to file an appeal. Start by reviewing the denial notice from your Medicaid plan. Submit a written appeal to your Medicaid plan or managed care organization, including any supporting documentation from your provider. If the first appeal isn’t successful, you may request a state fair hearing.
Scheduling your first virtual appointment is an exciting step. After finding an in-network provider, reach out to their office to request a telehealth session. Make sure to have your Medicaid ID handy, as the provider will need to verify your insurance before confirming the appointment.
Before starting your first session, make sure your technology is ready. Most virtual therapy appointments require a device with a camera and microphone and a stable internet connection. Many therapy providers use secure video platforms that are accessible through common web browsers or mobile apps.
Virtual sessions are required by federal law to be conducted through HIPAA-compliant platforms. This means your personal health information is encrypted and securely stored. Therapists must use video services that meet strict privacy standards—no public apps or unsecured video calls are allowed for Medicaid-covered telehealth4.
Staying on top of your Medicaid benefits is essential. Each Medicaid plan has its own session limits, authorization steps, and renewal timelines. Most plans in Vermont, Massachusetts, Connecticut, and New Hampshire allow between 10 and 30 sessions per year, but some individuals may qualify for more sessions if they have complex needs8.
It’s a good idea to use a simple calendar or your patient portal to mark each completed virtual mental health session. If your plan requires a new authorization after a certain number of visits, ask your provider to submit the paperwork early to prevent interruptions in support.
Medicaid plans across Vermont, Massachusetts, Connecticut, and New Hampshire support integrated treatment, which means therapy and substance use support can be provided together. For those using Medicaid-approved online counseling, it’s helpful to let both your mental health and substance use treatment providers know about your dual needs so they can coordinate authorizations.
Even when following these steps carefully, coverage issues may arise. Prior authorization denials represent the most frequent obstacle beneficiaries encounter. These often occur when documentation doesn't demonstrate medical necessity according to the state's criteria. If a treatment request is denied, providers can submit additional clinical information showing why the recommended intensity level is appropriate.
If you cannot find a suitable therapist through your plan’s directory, you still have options. One approach is to contact your Medicaid plan and ask about out-of-network exceptions. Another valuable option is to reach out to community mental health centers or local clinics, which often have more flexible intake processes.
| Option | How It Helps |
|---|---|
| Out-of-Network Exception Request | May grant access to external therapists for virtual care |
| Community Mental Health Centers | Higher Medicaid acceptance, flexible intake, virtual care |
| Local Nonprofit Clinics | Often specialize in behavioral health and telehealth |
Requesting an out-of-network exception allows you to ask your Medicaid plan for special permission to see a therapist who isn’t normally covered. Call your Medicaid plan’s member services and explain that you cannot find an in-network provider for the type of online counseling you need. Be prepared to document your search efforts.
Community mental health centers are often designed to serve people with Medicaid and typically offer a wider range of virtual behavioral health services. People in Vermont, Massachusetts, Connecticut, and New Hampshire can usually find a local center by searching their state Medicaid website or calling their health plan’s member services for a referral.
Coverage denials or delays can feel discouraging, but there are clear steps to help resolve these issues. First, review the denial letter carefully. If your therapy was denied due to missing information, reach out to your provider. For denials that seem unfair, you have rights under the Mental Health Parity and Addiction Equity Act (MHPAEA)5.
Prior authorization means your Medicaid plan wants to review and approve certain therapy services before they start. This is common for virtual mental health care, especially if you need more sessions than your plan usually allows. If you’re waiting for approval, check in with your provider to make sure all documents are submitted.
If your appeal is denied or delayed, you have the right to request a state fair hearing. This right is available in Vermont, Massachusetts, Connecticut, and New Hampshire. The hearing process starts by submitting a written request, usually within 60 days of your denial notice. During the hearing, you’ll have the opportunity to present your situation and share why you believe the denial is unfair.
Access to quality addiction services shouldn't depend on where someone lives or their insurance coverage. Virtual care has transformed how people receive support, breaking down traditional barriers that often prevented individuals from getting help when they needed it most.
Telehealth platforms now make it possible for people across Vermont, Massachusetts, Connecticut, and New Hampshire to connect with experienced clinicians from their own homes. This approach eliminates transportation challenges and creates a more comfortable environment when beginning a recovery journey.
Medicaid acceptance is particularly important because many people seeking addiction support rely on this coverage. Virtual care specialists that work with Medicaid ensure that financial constraints don't become another obstacle to recovery. When individuals face co-occurring psychiatric conditions alongside addiction challenges, integrated virtual care provides comprehensive support.
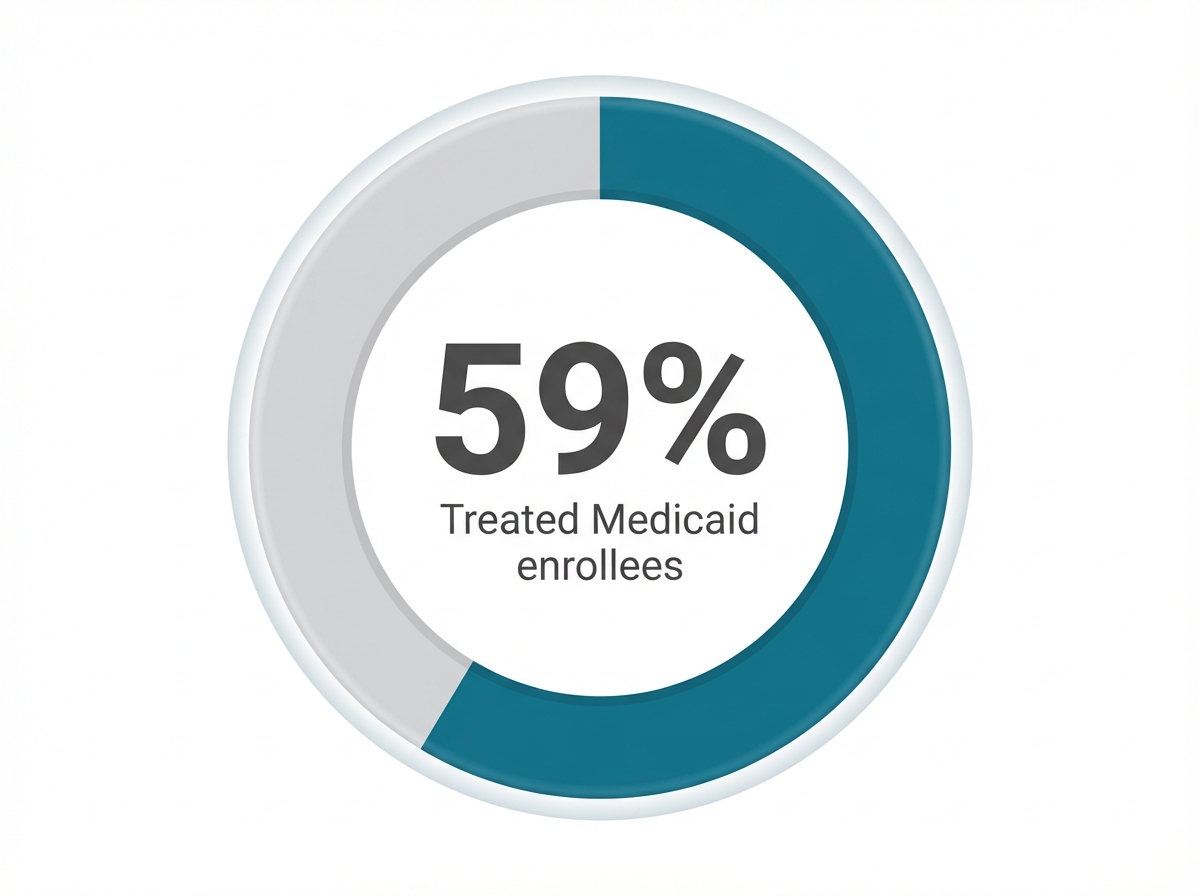
Yes, Medicaid covers online therapy for people who have both substance use disorder (SUD) and mental health concerns, as long as the care is provided by a qualified, in-network provider. This is commonly known as co-occurring or integrated treatment, and it is available in Vermont, Massachusetts, Connecticut, and New Hampshire through telehealth. Medicaid is the largest payer for both mental health and substance use services in the U.S., and state plans are required to treat these services with parity under the law10, 5.
If your Medicaid plan directory lists a provider as in-network but the provider says they don’t accept your insurance, contact your Medicaid plan’s member services and report the discrepancy. Ask them to help verify the provider’s current network status and to suggest other in-network therapists offering virtual sessions. In some cases, if you document that no in-network providers are actually available, your plan may grant an out-of-network exception3.
No, your employer and family members will not be notified. Privacy protections are a core part of both Medicaid and telehealth services. Therapists and online therapy platforms that take Medicaid are required by law to follow HIPAA rules, which means your personal health information remains confidential and is not shared with anyone without your written consent4.
Yes, trauma-focused therapies like Eye Movement Desensitization and Reprocessing (EMDR) are covered by Medicaid for online sessions in most states, including Vermont, Massachusetts, Connecticut, and New Hampshire. Medicaid generally pays for evidence-based therapy modalities when provided by licensed, in-network therapists8.
If you reach the session limit, most Medicaid plans allow for additional sessions if your provider submits a request showing that more therapy is medically necessary. This process is called prior authorization. Ask your therapist to contact your Medicaid plan early to request extra visits8.
Yes, you can switch therapists. Medicaid plans let you choose another in-network therapist for virtual sessions. To make the switch, contact your Medicaid plan’s member services or use the provider directory to search for other online therapy options that take Medicaid.
In most cases, you do not need a referral. Many Medicaid plans allow you to schedule virtual mental health sessions directly with an in-network provider. However, some managed care plans may require a referral for certain types of specialty treatment, so it’s a good idea to check your specific Medicaid plan documents.
If you live in a non-expansion state, qualifying for Medicaid is more challenging and usually limited to specific groups like people with disabilities or pregnant individuals. If you do qualify, your plan will still offer mental health coverage, including virtual therapy, though session limits may be stricter7.
Yes, master's-level therapists—such as licensed clinical social workers (LCSWs) and licensed mental health counselors (LMHCs)—are fully qualified to provide online therapy through Medicaid. Both groups are trained to deliver evidence-based therapy for mental health and substance use concerns3, 8.
Yes, you may be able to receive Medication-Assisted Treatment (MAT) prescriptions through online therapy if your provider is authorized and your state allows virtual prescribing. Medicaid plans typically cover both the therapy and medication components of MAT as part of co-occurring disorder treatment10.
Yes, online therapy can accommodate sensory or communication needs. Many Medicaid-approved virtual therapists can tailor sessions using visual supports, chat features, or flexible pacing. Let your provider know about your specific needs so they can adjust their approach.
Yes, Medicaid generally covers family therapy sessions if they are part of an evidence-based treatment plan for the Medicaid-enrolled individual. This is available in Vermont, Massachusetts, Connecticut, and New Hampshire as part of covered behavioral health services8.
Reach out to your provider immediately. Contact your state Medicaid office to check if you qualify for a special enrollment period or can appeal. If you are no longer eligible, ask your provider about sliding scale fees or other resources to continue care.
Yes, Medicaid often covers audio-only therapy sessions when video access is not reliable, especially in rural areas. State Medicaid programs in Vermont, Massachusetts, Connecticut, and New Hampshire have adopted telehealth parity which often includes audio-only options4.
Ask the provider directly about their privacy practices. Look for privacy statements or HIPAA compliance badges on the provider’s website. Platforms like Doxy.me or Zoom for Healthcare are widely recognized as meeting HIPAA requirements.

November 6, 2025
.jpg)
May 28, 2025

May 20, 2025