
Addiction Therapy Near Me: Accessible, Stigma-Free Therapy from Home with Pathfinder Recovery
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
When seeking rehab in Vermont, individuals face a critical decision regarding the delivery of their care. Traditional residential treatment centers have long been the standard, offering structured environments with face-to-face interactions and immediate availability of medical staff. These facilities excel at providing intensive monitoring and creating separation from triggering environments, which can be crucial during early recovery stages.
Conversely, digital treatment platforms have emerged as a powerful alternative, breaking down barriers that previously prevented countless individuals from receiving care. Online therapy services deliver proven therapies through secure video conferencing, allowing participants to engage in individual counseling, group therapy, and educational sessions from their own homes. This approach maintains therapeutic effectiveness while offering unprecedented flexibility when balancing work commitments, childcare needs, or geographic limitations.
The accessibility advantages of remote services are particularly significant in rural areas where treatment facilities may be hours away. Transportation challenges, which affect numerous individuals seeking recovery support, become irrelevant when sessions are conducted online. Telehealth programs serving regions like Vermont, Massachusetts, Connecticut, and New Hampshire have demonstrated how digital platforms can extend specialized care to underserved communities. Additionally, online treatment options often reduce the financial burden associated with residential care by eliminating housing costs and allowing participants to maintain employment during their recovery journey.
When individuals have established support systems at home, online treatment offers the advantage of maintaining those connections while building new recovery skills. Participants learn to navigate real-world challenges in their actual living environments, practicing coping strategies where they'll ultimately need to apply them. Many telehealth services, such as those offered by Pathfinder Recovery, integrate comprehensive addiction treatment with behavioral health support, recognizing that those in recovery often face interconnected challenges requiring coordinated care.
In-person rehab in Vermont provides individuals with a structured environment where recovery can happen face-to-face with a team of professionals. This treatment model often includes residential stays, intensive outpatient programs, and on-site group or individual sessions tailored to support substance use and co-occurring mental health needs. For many, being physically present in a treatment facility helps establish routine, accountability, and immediate access to support—especially when managing complex substance use challenges.
Research highlights that intensive outpatient and residential settings may be especially effective for those with high-acuity needs or severe co-occurring disorders, making this type of addiction treatment a vital option for some individuals6.
Residential and intensive settings deliver around-the-clock care, providing a stable and supportive atmosphere for people facing severe substance use disorders or complex co-occurring mental health challenges. These programs offer:
Industry leaders note that such environments can be especially beneficial for those with recent suicidal thoughts or repeated relapses, as the immersive care model strengthens accountability6. For individuals who need high-level supervision or are stepping down from inpatient care, residential addiction treatment centers in Vermont can bridge the gap between crisis and ongoing recovery.
Face-to-face therapeutic approaches provide a unique opportunity for individuals to build trust and connection with their treatment team. Sharing space with peers and counselors in real time allows for immediate feedback, emotional support, and the subtle cues that come from body language and presence. Many addiction treatment centers in Vermont offer group therapy and individual counseling as core components, drawing on evidence-based practices like cognitive behavioral therapy and motivational interviewing.
Research shows that matching the therapy format to individual preferences—whether group or one-on-one—can improve engagement and outcomes for people with substance use disorders10. These in-person experiences can foster a strong sense of community, which is especially valuable for those who thrive on direct social interaction during recovery.
Virtual rehab in Vermont uses secure video conferencing, phone calls, and digital tools to bring addiction treatment and co-occurring mental health support directly to people’s homes. Instead of traveling to a treatment center, individuals connect with licensed professionals for therapy, counseling, and medication management online. Many virtual addiction treatment programs follow structured schedules similar to in-person care—including group sessions and one-on-one meetings—but with the added flexibility of remote access.
Industry leaders find that telehealth can reduce barriers like transportation, work conflicts, and childcare needs, making support more practical for many1. Studies reveal that virtual care is just as effective as in-person treatment for intensive outpatient and medication-assisted programs, offering a reliable option for those who need flexibility without sacrificing quality1.
Telehealth delivery models are designed to make substance use and co-occurring mental health care flexible and accessible. Most virtual addiction treatment programs use secure video calls, phone check-ins, and digital messaging for therapy and medication management. Programs typically mirror in-person schedules, offering both individual and group sessions online to support continued engagement and accountability.
Industry experts note that these telehealth models help reduce barriers like travel and long wait times, which over half of individuals cite as major obstacles to starting treatment5. Many addiction recovery programs in Vermont now use a hybrid approach, blending scheduled virtual sessions with on-demand digital support to keep people connected to care between appointments.
Participating in virtual rehab means having access to a reliable internet connection, a smartphone, tablet, or computer, and enough digital literacy to use video conferencing platforms. Most addiction treatment programs recommend broadband internet for smooth therapy sessions, as interruptions or lags can disrupt care.
Yet, about 22% of rural areas in the U.S. lack high-speed broadband, which can make accessing virtual addiction treatment difficult for some residents8. Many telehealth platforms are designed to be user-friendly, and some offer support for people newer to technology. Addiction recovery programs may also guide individuals on setting up devices or finding local resources to boost internet access.
Research demonstrates that both conventional residential treatment and digital recovery services can achieve positive outcomes for individuals in recovery, though their effectiveness varies based on individual circumstances and program quality. Conventional residential treatment has long been the gold standard, with studies showing completion rates between 40-60% for structured interventions. These settings provide organized environments with immediate medical support and face-to-face therapeutic interactions that many patients find essential during early recovery.
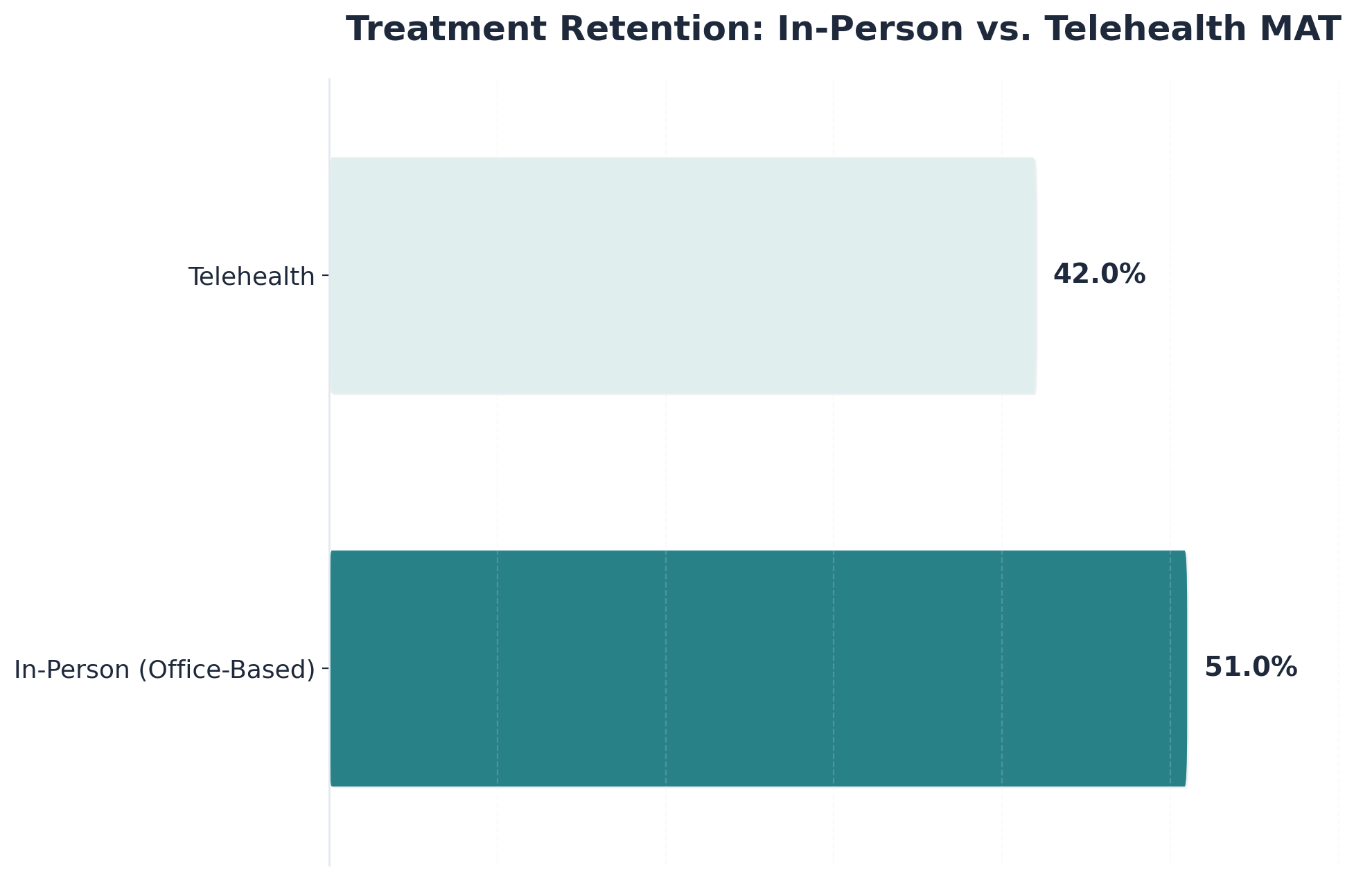
Virtual rehabilitation has emerged as a clinically validated alternative, with recent studies indicating comparable outcomes to traditional settings when programs maintain rigorous clinical standards. A 2022 study published in the Journal of Substance Abuse Treatment found that telehealth-based treatment showed retention rates of 45-65% similar to in-person care, with some participants reporting higher engagement due to reduced logistical barriers. A 2023 analysis in Addiction Science & Clinical Practice further confirmed that virtual treatment completion rates ranged from 42-58% across multiple programs, closely mirroring traditional facility outcomes.
| Metric | In-Person Residential | Virtual / Telehealth |
|---|---|---|
| Completion Rates | 40% - 60% | 42% - 58% |
| Retention (MAT) | Standard Baseline | Comparable or Higher |
| Primary Benefit | Intensive Monitoring | Continuity of Care |
These comparable outcomes stem from shared clinical foundations across both modalities. The clinical effectiveness of either approach ultimately depends on the comprehensiveness of services provided. Effective interventions—whether virtual or center-based—share common elements: research-supported therapies, qualified clinical staff, individualized treatment planning, and integrated support for concurrent psychiatric conditions.
Treatment outcomes and retention rates are essential for anyone weighing options for rehab in Vermont. When comparing traditional in-person and virtual substance use disorder programs, research shows that both approaches can lead to significant improvements in symptom reduction and quality of life, especially for intensive outpatient and medication-assisted treatment1. Many addiction treatment centers now see similar retention rates between telehealth and face-to-face models, meaning people are just as likely to stay engaged in care regardless of the delivery method9.
That said, some individuals with complex needs or repeated relapses may benefit more from the direct oversight offered by in-person addiction recovery programs6. Studies reveal that matching the treatment setting to a person’s specific needs, including co-occurring mental health support, is key to long-term recovery.
Evidence for virtual care success is clear. Multiple studies confirm that virtual addiction treatment programs—especially intensive outpatient and medication-assisted treatment—deliver clinical outcomes on par with traditional in-person recovery programs1. This means individuals can achieve similar reductions in substance use symptoms and improvements in quality of life, regardless of whether care is delivered face-to-face or online.
Research also highlights that retention rates for medication-assisted treatment provided via telehealth are comparable to, and sometimes even slightly better than, in-person office-based care9. For many, the flexibility of online addiction treatment removes common barriers like travel, scheduling conflicts, and stigma.
In-person care stands out as the superior choice for individuals who have high-acuity needs, recent suicidal thoughts, or a history of repeated relapse. Research confirms that residential and intensive outpatient programs provide a level of oversight, routine, and immediate crisis support that virtual care cannot always match, especially when safety or stabilization is a concern6.
Addiction treatment centers are uniquely equipped to offer 24/7 monitoring, hands-on interventions, and direct access to multidisciplinary teams—benefits that are critical for those facing severe substance use or complex mental health needs. For some, the physical environment and daily structure of in-person addiction recovery programs make all the difference in preventing setbacks and building lasting change.
Medication-assisted treatment (MAT) is a key component of many rehab programs in Vermont—delivering medications like buprenorphine alongside counseling to support recovery from opioid use disorder. In-person MAT services often involve direct visits to a clinic, where individuals can receive medical supervision and hands-on support from a treatment team.
Virtual MAT programs, by contrast, allow people to connect with licensed prescribers and counselors through secure video or phone visits, making it easier for those in rural or remote areas to stay engaged in their treatment plan4. Research shows that telehealth-based MAT produces retention and abstinence rates comparable to, and sometimes even better than, traditional in-person models, especially when it comes to ongoing engagement and convenience9.
Virtual medication-assisted treatment (MAT) programs in Vermont are transforming how individuals access opioid use disorder support. Instead of needing to visit a clinic in person, people can connect with medical providers and counselors through secure video calls or phone visits, allowing for prescription management and therapy from the comfort of home. This approach is especially helpful for those in rural communities or anyone facing transportation or scheduling barriers.
Research shows that telehealth-based MAT leads to retention and abstinence rates that are just as strong, and sometimes even better, than traditional office-based care4, 9. Many addiction treatment programs now use digital tools to monitor progress, provide real-time support, and streamline communication, making recovery more accessible.
Vermont’s hub-and-spoke model is a unique system that has expanded access to medication-assisted treatment (MAT) for opioid use disorder across the state. In this approach, specialized "hubs"—often large addiction treatment centers—provide intensive services such as initial assessments and stabilization, while "spokes" are community healthcare providers or medical practices that offer ongoing support and maintenance.
This integrated model allows individuals in rehab in Vermont to transition smoothly from intensive to ongoing care, ensuring continuity and flexibility. Research shows that Vermont now has one of the highest rates of opioid use disorder treatment capacity in the nation, directly linked to the success of the hub-and-spoke system2.
Beyond the basic question of treatment location lies a complex web of practical barriers that determine whether individuals can access and sustain recovery support. While geographic distance matters, the real-world obstacles often involve intersecting challenges: the single parent who cannot arrange overnight childcare for residential treatment, the hourly worker whose schedule changes weekly, or the individual in early recovery who lacks a driver's license due to past DUI convictions.
Research indicates that approximately 74% of U.S. counties have no addiction treatment facilities offering medications for opioid use disorder, creating what researchers term "treatment deserts." These gaps disproportionately affect rural populations, where the nearest qualified provider may be 50+ miles away. In mountainous regions of New England, winter weather compounds this challenge—a single snowstorm can mean missing critical therapy sessions or medication management appointments during vulnerable early recovery periods.
Telehealth platforms have emerged as one solution to these access gaps, though they introduce their own requirements. Effective virtual treatment depends on reliable internet connectivity (minimum 3-5 Mbps for video sessions), private space for confidential conversations, and basic digital literacy. These prerequisites can themselves become barriers: rural areas often have limited broadband infrastructure, individuals in unstable housing may lack privacy, and older adults or those without smartphone access may struggle with technology platforms.
The practical advantages of remote care extend beyond convenience when these technological prerequisites are met. Participants can attend therapy sessions from safe, comfortable environments without navigating stigma associated with entering treatment facilities. When managing concurrent psychiatric conditions alongside addiction, web-based platforms provide consistent delivery of integrated care without the logistical complexity of coordinating multiple on-site appointments across different locations and providers.
Financial accessibility varies significantly between modalities. While residential programs typically cost $5,000-$30,000+ for 30-day stays, intensive outpatient programs range from $3,000-$10,000 for similar durations, and telehealth options often fall at the lower end of this spectrum. Insurance coverage patterns differ too—some plans impose stricter limitations on residential benefits while offering better coverage for outpatient services. Beyond direct treatment costs, participants in on-site programs face indirect expenses: lost wages during treatment, transportation costs for family visits, and potential job loss from extended absences.
Overcoming barriers is crucial for anyone seeking rehab in Vermont, especially when practical obstacles threaten to delay or derail recovery. Studies reveal that over half of individuals identify long wait times as a major barrier to entering substance use treatment, while others face challenges like lack of reliable transportation and geographic isolation—issues that are especially common in rural parts of Vermont5, 3.
Virtual addiction treatment programs and telehealth-based care have expanded access for many, minimizing the need for travel and making support available from nearly anywhere with an internet connection. Still, the digital divide remains a real concern, as about 22% of rural areas lack adequate broadband, limiting access for some residents8. Addiction recovery programs are increasingly focused on flexible delivery and community partnerships to help bridge these gaps for those who need it most.
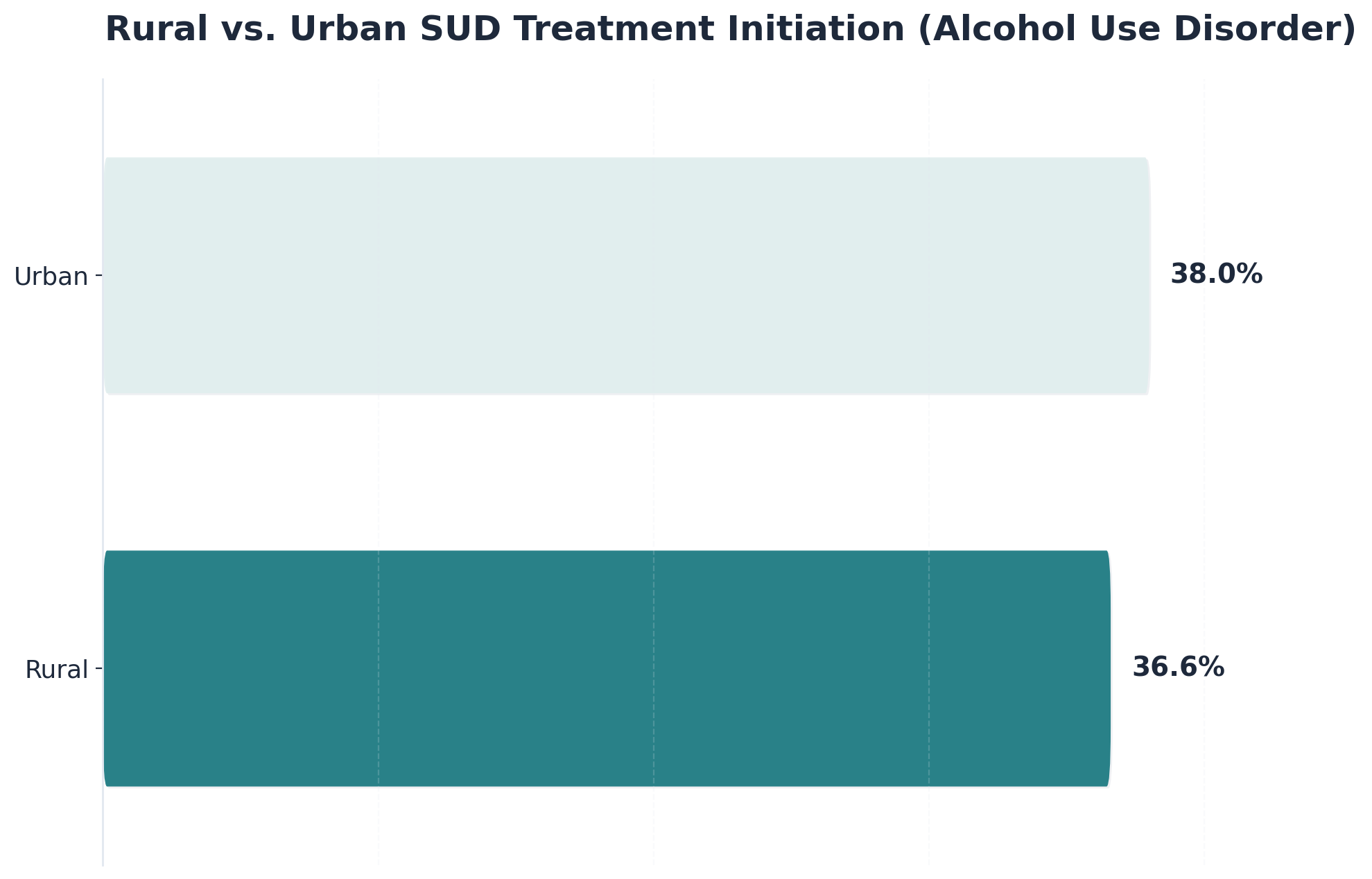
Geographic and transportation challenges remain a major hurdle. Individuals living in rural regions often travel long distances to reach addiction treatment centers, and reliable public transportation can be scarce or nonexistent. Studies reveal that people in rural areas have lower rates of treatment initiation for substance use disorders compared to those in urban settings—36.6% versus 38% for alcohol use disorder, for example—highlighting a measurable access gap3.
Limited car ownership and harsh winter conditions add to these barriers, making it even harder for some to attend consistent in-person sessions. Virtual addiction recovery programs can help bridge these gaps by delivering care directly to people’s homes, but the digital divide—such as inadequate broadband in 22% of rural areas—means not everyone can access remote services easily8.
Wait times can be a deciding factor for people seeking rehab in Vermont, as delays often weaken motivation or lead to missed opportunities for starting recovery. Studies reveal that more than half (53.8%) of individuals identify long wait times as a primary barrier to entering addiction treatment, which means many are left waiting days or even weeks before their first session5.
Virtual addiction treatment programs address this by offering faster intake, flexible scheduling, and sometimes even same-day appointments—all accessible from home with just an internet connection. This rapid access helps people begin their addiction recovery journey when their readiness is highest, reducing the chances of disengagement. However, for those without dependable broadband or devices, these benefits can be harder to reach, highlighting the need for more inclusive technology solutions8.
Cost and insurance considerations can play a big role in choosing between in-person and virtual rehab in Vermont. Research shows that virtual addiction treatment is more cost-effective for both individuals and society, largely because it reduces travel expenses, time away from work, and other indirect costs9. Many addiction recovery programs now accept Medicaid, Medicare, and private insurance for both in-person and telehealth services, creating more flexibility for those seeking help.
Industry experts report that reimbursement rates for telehealth are reaching near parity with in-person care, especially for medication-assisted treatment and intensive outpatient programs9.
Societal cost-effectiveness is a key factor when comparing in-person and virtual rehab. Research shows that telehealth addiction treatment delivers equivalent clinical outcomes to in-person care but with lower overall costs to society. For example, office-based treatment for opioid use disorder incurs an additional $3,750 per one percent increase in retention compared to telehealth, even though both approaches yield similar results9.
This cost advantage comes from reduced travel, less time off work, and fewer indirect expenses for individuals and communities. Addiction recovery programs that offer virtual options help maximize the impact of every healthcare dollar while still providing evidence-based care.
Vermont has seen a steady increase in telehealth use for addiction treatment and mental health support, especially since the pandemic. Recent data highlight that total professional services—including both in-person and telehealth—covered by Medicare in Vermont rose from 11,090,900 in 2020 to 13,603,900 in 2022, reflecting a clear upward trend in virtual care utilization8.
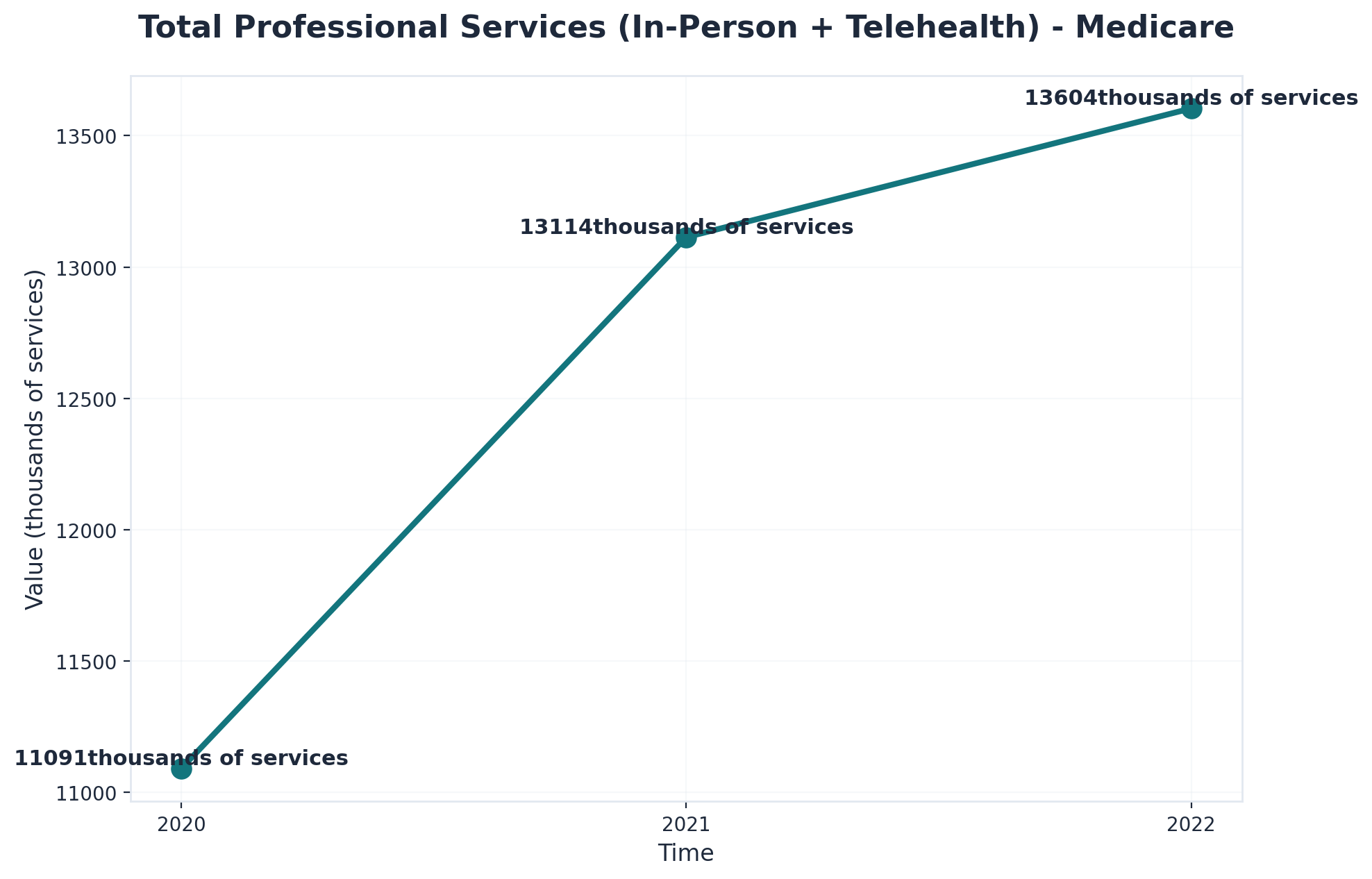
Medicaid figures show similar growth, with total services rising from 12,134,700 in 2020 to 14,597,100 in 2022. For rehab in Vermont, this means more people are accessing addiction recovery programs and co-occurring mental health care remotely, thanks to expanded coverage and evolving technology.
The psychological and social dimensions of treatment environment significantly influence recovery outcomes. Where someone receives care affects not only their comfort level but also their willingness to engage fully in the recovery process and their ability to practice new skills in realistic contexts.
Privacy considerations represent a substantial barrier to treatment access. Many individuals delay or avoid seeking help due to concerns about being seen entering a treatment facility, explaining extended absences to employers, or having their struggles become known within their communities. These concerns aren't merely about vanity—they reflect legitimate worries about professional consequences, strained relationships, and social stigma that persists despite growing awareness of addiction as a medical condition.
Remote treatment addresses these privacy concerns directly. Participants can engage in clinically proven care without visible markers of treatment attendance. They avoid the need to explain gaps in their work history or sudden lifestyle changes to colleagues, extended family, or community members. This discretion often enables individuals to seek help earlier in their addiction progression, before circumstances become severe enough to require more intensive intervention.
The treatment environment also shapes how individuals develop and practice recovery skills. Residential settings provide controlled environments where triggers are minimized and support is immediately available—an approach that offers safety during acute phases of recovery. However, this protective structure can create challenges when individuals transition back to their regular environments, where they must navigate real-world triggers, relationships, and stressors without the same level of insulation.
Telehealth programs like Pathfinder Recovery—serving Vermont, Massachusetts, Connecticut, and New Hampshire—take a different approach by embedding treatment within participants' actual living environments. Individuals learn to manage cravings, resolve conflicts, and establish healthy routines in the same settings where they'll continue applying these skills after treatment ends. They practice recovery while maintaining their roles as parents, employees, and community members rather than temporarily stepping away from these identities.
This real-world practice environment offers distinct psychological advantages. Participants build confidence in their ability to maintain recovery amid daily responsibilities and challenges. They strengthen existing support networks rather than relying exclusively on treatment-based relationships that may not continue post-program. The integration of clinical support with ongoing life demands creates a recovery foundation built on realistic circumstances rather than the artificial structure of residential care—an approach that for many individuals produces more durable, transferable recovery skills.
Confidentiality is a top priority for many considering rehab in Vermont, especially given how stigma can impact people’s willingness to seek help. Virtual addiction recovery programs offer a way to participate in treatment privately, from home, without the concern of being recognized at a clinic or facility.
"Studies reveal that this added layer of privacy can help reduce barriers created by stigma and encourage more individuals to access care."8
In smaller towns or rural areas, where community ties are strong and anonymity is harder to maintain, the ability to connect with addiction treatment programs remotely can make all the difference. Both in-person and virtual care models are required to protect patient confidentiality, but telehealth’s home-based approach provides a unique sense of comfort and control.
Virtual care offers distinct privacy advantages. By participating in addiction treatment programs from home, individuals can avoid the anxiety that may come with being seen at a local clinic—something that can be especially important in close-knit or rural communities. Research shows that this level of discretion encourages more people to seek help, as private, home-based sessions reduce worries about community stigma and make the process feel safer and more comfortable8.
Many virtual addiction recovery programs use secure platforms and encrypted communications, so conversations and records remain confidential. For people who value anonymity or feel nervous about in-person visits, this added privacy can be a deciding factor in sticking with an addiction recovery program.
HIPAA compliance is a cornerstone of both in-person and virtual rehab in Vermont, ensuring that sensitive health information stays protected, even as care moves online. Virtual addiction treatment programs use secure, encrypted platforms that meet strict federal privacy standards set by the Health Insurance Portability and Accountability Act (HIPAA). This means every video call, message, and digital health record is safeguarded against unauthorized access.
Research shows that telehealth providers must follow the same confidentiality rules as traditional clinics, offering peace of mind for those concerned about privacy during their recovery journey8. Addiction recovery programs regularly update their systems and train staff to stay current with HIPAA requirements, so individuals can trust that their information is handled with the highest level of security.
Integration with daily life is a major factor for anyone considering rehab in Vermont. Virtual addiction recovery programs offer the flexibility to attend therapy sessions from home, making it easier for people to manage work shifts, family duties, or unpredictable schedules. Research shows that matching treatment to a person’s routines and real-world demands increases engagement and recovery success10.
In contrast, in-person addiction treatment centers provide structure and a break from daily distractions, which may benefit those who need routine or a more immersive setting. Both virtual and in-person options aim to help individuals build healthy habits that fit their everyday lives, but the right fit depends on whether you need flexibility or thrive with hands-on support.
Balancing work and family responsibilities is a major concern for many people seeking rehab in Vermont. Virtual addiction recovery programs make it possible to fit therapy and support sessions around job shifts, childcare, and other daily obligations. Research shows that this kind of scheduling flexibility increases engagement and helps people stick with their treatment plan10.
For parents or caregivers, online addiction treatment means less time away from home and fewer logistical hurdles, such as arranging transportation or finding coverage for dependents. In contrast, in-person addiction treatment centers offer a structured break from daily stressors, which can help some individuals focus solely on recovery without outside distractions.
Building real-world coping skills is a cornerstone of successful rehab in Vermont, whether someone chooses in-person or virtual addiction recovery programs. In traditional addiction treatment centers, individuals practice skills like stress management, healthy communication, and relapse prevention in a structured setting with immediate support from peers and counselors. This hands-on approach can help people translate lessons from therapy into daily routines.
For those using virtual addiction treatment programs, coping strategies are woven into real-time life challenges—such as handling cravings at home or managing triggers in familiar environments. Studies reveal that when treatment fits daily life and allows for practice in real-world settings, people are more likely to stay engaged and maintain progress after formal care ends10.
Recovery is deeply personal, and choosing the right treatment approach requires careful consideration of individual circumstances, needs, and recovery goals. Understanding when each option serves best helps ensure appropriate matching to the level of care that will support lasting change.
Consider in-person treatment when: Medical detoxification is needed, co-occurring mental health conditions require intensive stabilization, the home environment presents active triggers or unsafe situations, previous outpatient attempts haven't succeeded, or immediate 24/7 clinical support would significantly reduce relapse risk. The structured setting and physical separation from familiar patterns can create the foundation needed for early recovery.
Consider telehealth treatment when: Medical withdrawal risks are low to moderate, stable housing and a supportive home environment exist, work or family responsibilities make residential treatment impractical, geographic isolation limits access to quality local programs, or maintaining daily routines would strengthen rather than undermine recovery efforts. Digital formats work particularly well when motivation is strong and external accountability structures are in place.
Questions to guide your decision:
What does medical assessment indicate about withdrawal risks?Do I have safe, stable housing during treatment?Would maintaining my current routine support or hinder my recovery?What co-occurring conditions need attention?Appropriate matching matters significantly. Research demonstrates that telehealth produces comparable outcomes to conventional treatment—but only when clinical factors, readiness for change, environmental stability, and support systems align with this level of care. A thorough assessment by qualified professionals helps determine fit. Many people also benefit from hybrid or stepped-care approaches: starting with intensive in-person treatment, then transitioning to digital continuing care, or beginning with telehealth and stepping up if needs change.
Matching treatment to individual needs is the key to finding the most effective rehab in Vermont. Research shows that both in-person and virtual addiction recovery programs deliver strong outcomes, but choosing the right setting depends on the severity of symptoms, co-occurring mental health needs, and personal circumstances1, 6.
For some, the structure and daily accountability of in-person addiction treatment centers make a real difference, especially when managing complex challenges or recent relapses. Others may benefit more from the accessibility and privacy that virtual addiction recovery programs provide—particularly if travel, schedule, or stigma are major barriers8. Studies reveal that aligning care with a person’s preferences and life demands increases engagement and long-term recovery success10.
High-acuity and complex cases require the most structured and hands-on support that rehab in Vermont can offer. Individuals with recent suicidal thoughts, repeated relapses, or severe co-occurring mental health conditions often benefit most from in-person addiction treatment centers, where around-the-clock supervision and immediate crisis intervention are available.
Research highlights that these residential or intensive outpatient programs deliver better outcomes for those with complex needs, as the immersive environment strengthens accountability and ensures rapid access to multidisciplinary teams6. Many addiction recovery programs use face-to-face approaches for people who need close monitoring or are transitioning from inpatient care.
Ideal candidates for virtual rehab in Vermont are individuals who need flexibility, value privacy, or face barriers like long travel distances and scheduling conflicts. Virtual addiction recovery programs are especially helpful for people balancing work, family, or living in rural areas without easy access to treatment centers.
Research shows that virtual care is just as effective as in-person settings for intensive outpatient and medication-assisted treatment, making it a reliable option for those with mild to moderate substance use challenges and stable home environments1, 9. This model is also beneficial for those who feel stigma about seeking help or who want to keep their recovery journey private.
Virtual rehab in Vermont with Pathfinder brings flexible, evidence-based recovery support straight to individuals’ homes, using secure telehealth tools to connect people with licensed professionals. Pathfinder specializes in helping those managing substance use and co-occurring mental health concerns, focusing on intensive outpatient and medication-assisted treatment—both proven to be highly effective in virtual formats1, 9.
Those participating in online addiction recovery programs benefit from personalized therapy, group sessions, and medication management, all designed to fit around work, family, and other daily responsibilities. Studies reveal that this approach not only matches the clinical outcomes of traditional rehab in Vermont but also removes barriers like transportation and stigma, making it easier for more people to access help8. Pathfinder’s fully virtual model is available to residents across Vermont, Massachusetts, Connecticut, and New Hampshire.
Pathfinder’s comprehensive remote care services are designed to meet people where they are—literally and figuratively. Individuals can access intensive outpatient support, medication-assisted treatment for substance use, and co-occurring mental health therapy, all from the comfort and privacy of home. These virtual addiction recovery programs combine regular video sessions with licensed professionals, online group therapy, and secure digital tools for medication management.
Research shows that this approach achieves outcomes on par with in-person care, particularly for intensive outpatient and MAT needs1, 9. Many people appreciate the flexibility to schedule appointments around work or family, while still receiving evidence-based treatment and ongoing support.
Addressing the digital divide is a priority for Pathfinder’s virtual rehab in Vermont, as gaps in broadband and device access can prevent some individuals from getting the care they need. Research shows that about 22% of rural areas lack high-speed internet, which remains a significant barrier for many seeking addiction treatment programs8.
To help bridge this gap, Pathfinder offers technical support to guide individuals through setup, recommends low-cost device options, and partners with local resources to connect clients to internet assistance programs. Many virtual addiction recovery programs are designed with user-friendly platforms, making it easier for those new to technology to participate.
Yes, switching from in-person to virtual rehab in Vermont is often possible if your circumstances change—such as a new work schedule, transportation issues, or moving to a rural area. Many addiction recovery programs in Vermont now offer flexible options that let individuals continue their care with the same treatment team, either fully online or as a hybrid model. Research shows that virtual rehab provides clinical outcomes similar to in-person programs, especially for intensive outpatient and medication-assisted treatment, so you won’t lose quality of care if you make the transition1, 9. If you’re considering a switch, talk with your treatment provider about your needs to ensure a smooth handoff and maintain your progress.
Virtual rehab in Vermont usually lets you get started much faster than most in-person programs. Research highlights that over half of people seeking treatment say long wait times are a major barrier—sometimes waiting days or weeks for an in-person opening5. By contrast, virtual addiction recovery programs in Vermont often offer rapid intake, flexible scheduling, and even same-day appointments, so you can begin your recovery journey as soon as you’re ready. This quick access is especially helpful for those eager to start therapy and medication-assisted treatment without delay.
Yes, most insurance plans—including Medicaid, Medicare, and many private insurers—cover virtual rehab in Vermont much like they do for in-person addiction treatment. Recent trends show that reimbursement rates for telehealth services are reaching near parity with traditional care, especially for intensive outpatient and medication-assisted treatment programs9. This means if your insurance covers in-person rehab, it likely also covers virtual addiction recovery programs in Vermont, though your exact benefits may depend on your specific plan.
Yes, you can receive virtual rehab in Vermont even if you live in a rural area with limited healthcare options. Virtual addiction recovery programs are specifically designed to overcome distance and transportation barriers by connecting you with licensed professionals for therapy, counseling, and medication-assisted treatment online. While about 22% of rural areas lack high-speed internet, many rehab programs in Vermont offer technical support, device recommendations, and can help you find community resources like libraries or clinics with secure Wi-Fi to make remote care possible8.
To participate in virtual rehab sessions for rehab in Vermont, you’ll need one of the following: a smartphone, tablet, laptop, or desktop computer with a camera, microphone, and internet access. Most addiction recovery programs in Vermont recommend using broadband or a stable Wi-Fi connection to ensure clear video and audio. Industry experts find that user-friendly telehealth platforms work well with common devices, so you don’t need special equipment or advanced tech skills8.
Pathfinder Recovery provides virtual care for co-occurring mental health conditions like depression and anxiety as part of their substance use disorder (SUD) treatment approach. While Pathfinder does not offer primary mental healthcare alone, their team is equipped to support individuals in rehab in Vermont who are managing both substance use and mental health symptoms at the same time. This integrated model is backed by research showing that virtual addiction treatment programs in Vermont can effectively address depression and anxiety alongside SUD, especially within intensive outpatient and medication-assisted treatment formats1.
If you want to participate in virtual rehab in Vermont but don’t have reliable internet at home, you’re not alone—about 22% of rural areas face similar challenges accessing high-speed broadband8. Many addiction recovery programs in Vermont are aware of this digital divide and work to help individuals find solutions. Options might include using a local library, community center, or clinic with secure Wi-Fi for your sessions. Some virtual addiction treatment programs in Vermont also offer technical support, recommend affordable devices, or connect you with local resources for discounted or free internet access.
No, your employer will not be notified if you attend virtual rehab in Vermont during work hours unless you choose to share that information. Virtual addiction recovery programs in Vermont are designed to protect your privacy—sessions are confidential and happen through secure, HIPAA-compliant platforms that do not involve your workplace or supervisor8. As long as you arrange your therapy or support meetings around your own schedule and use a private device or secure connection, your participation remains between you and your provider.
Yes, virtual medication-assisted treatment (MAT) is considered just as safe as receiving prescriptions in person for most people seeking rehab in Vermont. Research shows that telehealth-based MAT—where medications like buprenorphine are prescribed and managed through secure video or phone visits—results in retention and abstinence rates comparable to, and sometimes even better than, traditional office-based care4, 9. Licensed providers follow strict safety protocols, monitor progress closely, and use secure, HIPAA-compliant platforms to protect your privacy.
If you experience a relapse while participating in virtual rehab in Vermont, your care team will work with you quickly to adjust your recovery plan and provide extra support. Virtual addiction recovery programs in Vermont are designed to respond to setbacks with compassion—not judgment—so you can get back on track without losing momentum. Many programs offer flexible scheduling for urgent check-ins, access to crisis resources, and increased therapy sessions if needed. Studies reveal that matching treatment intensity to a person’s changing needs is key to long-term recovery success10.
Yes, family members can participate in your virtual treatment sessions for rehab in Vermont, as long as you and your clinical team agree it would support your recovery. Many virtual addiction recovery programs in Vermont actively encourage involving loved ones through secure video meetings, since family engagement can improve motivation and help with long-term success. These sessions are set up to protect your privacy and follow strict confidentiality rules, just like in-person care8.
Virtual programs for rehab in Vermont are increasingly designed to support neurodivergent individuals, including those with ADHD or autism. Many addiction recovery programs in Vermont now offer flexible session formats, such as shorter meetings, visual schedules, and clear routines, which can help reduce overwhelm and improve focus for people with attention or sensory differences. Providers are trained to adapt communication styles—using straightforward language, visual aids, and step-by-step instructions—to meet the unique needs of each participant.
If traditional rehab in Vermont didn’t bring the results you hoped for, trying a virtual addiction recovery program could offer a different experience and new opportunities for progress. Research shows that virtual rehab—especially for intensive outpatient and medication-assisted treatment—delivers clinical outcomes that are just as effective as in-person care, largely because it removes barriers like travel, wait times, and stigma that can stand in the way of staying engaged1, 9.
Pathfinder Recovery offers virtual rehab in Vermont for individuals with substance use and co-occurring mental health needs, but trauma-focused therapies like EMDR are not currently available through their telehealth platform. Instead, Pathfinder’s virtual addiction recovery programs focus on evidence-based approaches proven effective for intensive outpatient and medication-assisted treatment via secure video sessions1, 9. If trauma-specific therapies like EMDR are a priority, Pathfinder’s team can provide referrals to local providers specializing in these services.
The decision between facility-based and remote treatment ultimately depends on individual circumstances, preferences, and recovery needs. Traditional programs offer structured environments with face-to-face interactions and immediate medical support, which can be invaluable when requiring intensive care or when benefiting from physical separation from triggering environments. However, these programs often require significant time commitments, travel arrangements, and extended absences from work or home life.
Telehealth services have emerged as a powerful alternative that addresses many of these barriers while maintaining clinical effectiveness. Remote treatment provides the flexibility to attend therapy sessions from home, eliminating commute times and allowing individuals to integrate recovery into their daily lives. This approach works particularly well when balancing work obligations, childcare duties, or when residing in rural areas with limited specialized treatment facilities nearby. The convenience factor often leads to better attendance rates and sustained engagement throughout the recovery journey.
Throughout the New England region—including VT, MA, CT, and NH—Pathfinder Recovery offers comprehensive telehealth services that combine the clinical rigor of traditional programs with the accessibility of digital platforms. The program includes one-on-one therapy, group support sessions, and integrated treatment when managing both addiction challenges and psychiatric conditions simultaneously.
Remote rehabilitation through Pathfinder's services enables clients to build recovery skills while remaining connected to their support systems and maintaining their daily routines. This real-world application of coping strategies can strengthen long-term recovery outcomes, as participants practice new behaviors in the environments where they'll actually apply them. Whether someone needs the flexibility to work during treatment, prefers the privacy of receiving care at home, or simply lives far from traditional treatment centers, online therapy provides a viable path toward lasting recovery, allowing individuals to access professional support without the logistical barriers that might otherwise delay or prevent treatment.
Both facility-based and telehealth approaches have demonstrated effectiveness when properly matched to individual needs and circumstances—what matters most is taking that first step toward help rather than remaining paralyzed by indecision. The most important choice isn't necessarily which modality to select, but rather the decision to seek support in the first place. Consider your unique situation, the practical realities of your daily life, and what format would make it easiest for you to commit fully to the recovery process, then take action on that insight.

November 6, 2025

November 6, 2025

November 6, 2025