
Addiction Treatment At Home: Virtual Treatment that Meets You Where You Are
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
MassHealth, Massachusetts' Medicaid and Children's Health Insurance Program, provides comprehensive healthcare to qualifying state residents, including essential services for individuals struggling with addiction. Finding a rehab that accepts MassHealth is a crucial step for many, as coverage typically includes outpatient counseling, medication-assisted therapy, behavioral health services, and various levels of care designed to support long-term healing. The program recognizes that addiction is a medical condition requiring proven therapeutic interventions, and coverage extends to both in-person and virtual care options that meet clinical standards.
Virtual treatment options have become an increasingly valuable option for Bay State residents with MassHealth coverage. These telehealth offerings eliminate transportation barriers, reduce time away from work or family responsibilities, and provide access to specialized care that might not be available locally. When pursuing recovery, the convenience and privacy of virtual appointments make it easier to maintain consistent engagement with therapy—a critical factor in successful outcomes.
Many virtual addiction treatment programs accept MassHealth and serve qualifying residents throughout Massachusetts. These programs typically combine evidence-based therapeutic methods with integrated support services, recognizing that comprehensive care often yields better outcomes. Through secure telehealth platforms, individuals can access counseling, medication management when appropriate, and ongoing recovery support from the comfort and privacy of their own homes.
Understanding what MassHealth covers for virtual addiction treatment—and which programs accept this coverage—helps Bay State residents make informed decisions about their recovery options. With telehealth expanding access to specialized care, what should someone look for when evaluating virtual recovery programs that work with MassHealth?
This section explains exactly what MassHealth covers for substance use disorder (SUD) treatment—and why these benefits matter for anyone seeking a rehab that accepts MassHealth. MassHealth covers a full spectrum of addiction services, including medication-assisted treatment (MAT), individual and group counseling, outpatient programs, and residential care1. These offerings are designed to meet people wherever they are in their recovery process.
Services like MAT and behavioral therapy are considered best practice, and current guidelines recommend their use together for improved outcomes2. When searching for a substance use treatment center or virtual rehab that works with MassHealth, knowing these details can make all the difference.
MAT combines FDA-approved medications like buprenorphine, methadone, and naltrexone with supportive therapy to treat opioid and alcohol use disorders1. MassHealth covers these medications as part of its substance use disorder benefits, making them accessible through participating clinics and many virtual recovery programs.
Research shows that using these medications can reduce the risk of overdose by up to 76% at three months for those who stick with treatment9. For those searching for addiction treatment centers or virtual rehab in Massachusetts, access to MAT through MassHealth can be the difference between struggling alone and having reliable, proven support.
MassHealth covers a range of counseling options, including individual therapy, group sessions, and family or couples counseling—all recognized as best practice in addiction recovery1. These services aren’t limited to in-person visits; they’re also available through virtual platforms, making it easier to access support when and where it’s needed most3.
Many treatment centers that accept MassHealth insurance make counseling a core part of their programs, because research shows that therapy helps people develop coping skills and address the root causes of substance use2.
MassHealth now permanently covers virtual addiction treatment—including medication-assisted treatment and therapy—at the same reimbursement rate as traditional care, according to updated state policy3. This means you can connect with licensed providers using video or phone, removing geographic and transportation barriers.
Studies reveal that telehealth services for substance use disorder lead to similar recovery outcomes as in-person programs, offering real hope for people in rural areas or with mobility challenges6, 7. Many virtual programs accepting MassHealth insurance also provide support without extra technology requirements, making care even more accessible.
MassHealth now guarantees that virtual substance use disorder services—including therapy and medication management—are reimbursed at the same rate as in-person treatment, thanks to permanent telehealth policies3. This eliminates financial barriers for clinics and ensures that people can access quality care from home, work, or anywhere with a phone or internet connection.
Industry groups note that this level playing field encourages more providers to offer online addiction support, helping people in rural or underserved parts of Massachusetts find a rehab covered by MassHealth insurance4.
MassHealth members do not pay copayments for medically necessary opioid use counseling—including individual, group, and family sessions—whether treatment is delivered in-person or virtually2, 3. This policy, in place since July 2020, means that those searching for opioid counseling at a rehab that accepts MassHealth can focus on their recovery instead of worrying about session fees.
Studies reveal that eliminating out-of-pocket costs helps more people access ongoing care, which is especially important given that only 25% of adults who need opioid use disorder treatment actually receive recommended medications or counseling nationwide10. Virtual counseling covered by MassHealth insurance further expands access by making it simple to get support from home or a private, comfortable setting.
Massachusetts has seen significant growth in virtual recovery programs accepting MassHealth, with telehealth addiction services increasing by over 60% since 2020. According to recent data, approximately 40% of substance use disorder treatment now occurs through virtual platforms, demonstrating both the demand for and effectiveness of remote care options. These digital programs span the full continuum of care, from intensive outpatient programs (IOPs) requiring multiple weekly sessions to partial hospitalization programs (PHPs) offering structured daily support without overnight stays.
Virtual intensive outpatient programs typically involve 9-12 hours of weekly therapy through video sessions, combining individual counseling with group therapy and skills training. Partial hospitalization programs provide even more comprehensive care—often 20+ hours weekly—while allowing participants to remain at home. Both formats maintain clinical rigor while eliminating transportation barriers and scheduling conflicts that often prevent people from accessing traditional in-person treatment. MassHealth coverage extends to these telehealth options, ensuring that financial constraints don't limit access to appropriate care levels.
Telehealth recovery platforms accepting MassHealth typically provide services that include initial assessments, ongoing counseling sessions with licensed clinicians, medication management when appropriate, and peer support groups. Programs like Pathfinder and other Massachusetts-based telehealth providers deliver these comprehensive services through digital platforms, specializing in medication-assisted approaches combined with therapeutic interventions. These platforms maintain the same clinical standards as traditional in-person care while offering greater accessibility for individuals managing work schedules, childcare responsibilities, or mobility limitations.
The virtual care model also addresses concurrent psychiatric conditions alongside dependency care, recognizing that many people face interconnected challenges requiring integrated approaches. The digital format allows for more frequent check-ins and easier communication with care teams, which can be crucial during early recovery when support needs are highest. Bay State residents covered under the state's Medicaid initiative can access these telehealth recovery options as a practical pathway to beginning and sustaining recovery while maintaining daily routines and responsibilities.
Virtual addiction treatment options covered by MassHealth include intensive outpatient programs (IOP), at-home medical detox, and ongoing online substance use counseling. Research shows that virtual IOPs lead to similar abstinence rates and quality of life improvements as in-person programs at three months post-discharge6, 7. These evidence-based modalities combine individual and group therapy, medication management, and relapse prevention—all delivered through secure telehealth platforms.
| Modality | Typical Frequency | Best For |
|---|---|---|
| Virtual IOP | 3-5 days/week (9-12 hours) | Structured support while living at home. |
| At-Home Detox | Daily medical check-ins | Safe withdrawal management with supervision. |
| Online Counseling | 1-2 sessions/week | Ongoing maintenance and mental health support. |
Virtual IOP provides structured therapy, group support, and medication management entirely online—usually three to five days per week, but with flexible scheduling. Research shows that virtual addiction treatment, including online IOP, leads to comparable abstinence rates and quality of life improvements as traditional in-person programs at three months post-discharge6, 7. Many virtual rehabs that accept MassHealth design their IOPs so members can participate from home, making care accessible even for those balancing work, family, or transportation barriers.
At-home detox, sometimes called remote or virtual detox, involves withdrawing from substances under real-time medical supervision using telehealth technology. Programs provide frequent video or phone check-ins, symptom monitoring, and access to approved medications—all led by licensed clinicians. This approach can remove barriers like travel or stigma, making it easier for people to start recovery where they feel most comfortable.
Pathfinder Recovery specializes in virtual addiction care designed for people who want evidence-based support without travel or long wait times. Their programs—available to MassHealth members—include intensive outpatient services, online substance use counseling, and co-occurring mental health support alongside SUD treatment. Pathfinder makes it simple to verify coverage and start care, removing insurance confusion that often keeps people from getting help.
Research shows telehealth addiction treatment delivers outcomes similar to in-person rehab, with 3-month abstinence rates and quality of life improvements holding steady for virtual care users6, 7. It is important to note that while Pathfinder offers robust support for co-occurring disorders (such as anxiety or depression that accompany addiction), they do not provide primary mental healthcare services.
Pathfinder’s virtual addiction treatment is designed as a true continuum: care begins with rapid virtual assessment, followed by intensive outpatient programming, online substance use counseling, and ongoing relapse prevention—all accessible from home. The program adapts to changing needs, whether someone requires more structure after a setback or is ready for less frequent check-ins. Research shows these layered supports—delivered through telehealth—produce recovery outcomes on par with in-person care, with similar abstinence and quality of life improvements for MassHealth members6, 7.
Pathfinder’s virtual addiction treatment and online substance use counseling allow MassHealth members to book appointments in the early morning, evenings, or even weekends. This means people can get evidence-based support before or after work, making it much easier to stay engaged in care while juggling real-world demands. Research shows that telehealth addiction programs, like those at Pathfinder, produce recovery outcomes comparable to in-person care for individuals balancing work, family, and treatment needs6, 7.
Nearly 40% of Massachusetts residents seeking addiction treatment cite transportation as a significant barrier to accessing care, with rural communities facing even steeper challenges—some areas have wait times exceeding eight weeks for in-person appointments. These obstacles often delay critical intervention during the narrow window when someone feels ready to seek help.
Virtual treatment programs directly address the barriers that have traditionally prevented people from accessing care. Transportation challenges, scheduling conflicts with work or family responsibilities, and limited local options no longer stand in the way when proven therapeutic methods come directly to participants wherever they have internet access. This model eliminates commuting time, reduces conflicts with daily obligations, and expands access to specialized providers who might not be available locally.
"Consider Maria, a single mother in Western Massachusetts who works two jobs and has no reliable transportation. Traditional treatment would have required her to miss work, arrange childcare, and travel 45 minutes each way to the nearest facility. Through telehealth services that accept MassHealth, she now attends individual therapy sessions during her lunch break and joins evening group counseling after her children are asleep—all from home."
When someone experiences dual diagnosis conditions—both psychiatric challenges and addiction—integrated treatment becomes essential. Telehealth platforms can coordinate addiction services with concurrent psychiatric support, ensuring both conditions receive appropriate attention throughout the healing process. This integrated approach helps address the underlying factors contributing to problematic consumption patterns while building sustainable coping strategies.
The acceptance of MassHealth by remote treatment providers removes financial barriers that might otherwise delay or prevent people from seeking help. When combined with the flexibility and accessibility of telehealth services, more participants can begin their path to wellness without sacrificing other life responsibilities or facing prohibitive costs. For many Bay State residents, this combination of insurance coverage and virtual access represents the difference between continued struggle and beginning recovery.
Only 25% of adults who need opioid use disorder treatment actually receive medications for opioid use disorder (MOUD), despite clear evidence that these medications can reduce overdose risk by up to 76% at three months10, 9. Barriers include stigma, lack of awareness, and challenges navigating insurance or finding providers who offer evidence-based care. Virtual addiction treatment and online substance use counseling—both accepted by MassHealth—are removing some of these barriers by making care more private and easier to access.
Many people don’t realize that medications like buprenorphine or methadone—proven to reduce overdose risk by up to 76% at three months9—are available through a rehab that accepts MassHealth, including virtual addiction treatment options. Some providers may not routinely offer medications for opioid use disorder, and patients can face delays due to prior authorization or limited information about their insurance benefits. Technology is making it easier to find a MassHealth-covered provider and begin evidence-based medication support.
Stigma is one of the biggest reasons people delay or avoid getting help for substance use disorder—studies reveal that over 10% of those who felt they needed treatment didn’t seek it because they worried about negative attitudes from their communities8. Virtual addiction treatment and online substance use counseling, both covered by MassHealth, let people connect with licensed providers from the privacy of home. This means individuals don’t have to worry about being seen at a clinic or facing questions from neighbors, making it less intimidating to reach out for support.
Research shows that 43% of people with a substance use disorder also experience mental illness, yet only 38% of those who receive help actually get coordinated care for both conditions5. This fragmentation can result in missed diagnoses and less effective recovery. Virtual addiction treatment and online substance use counseling, now available through many MassHealth-accepting providers, are helping bridge this gap by offering integrated support from the same care team.
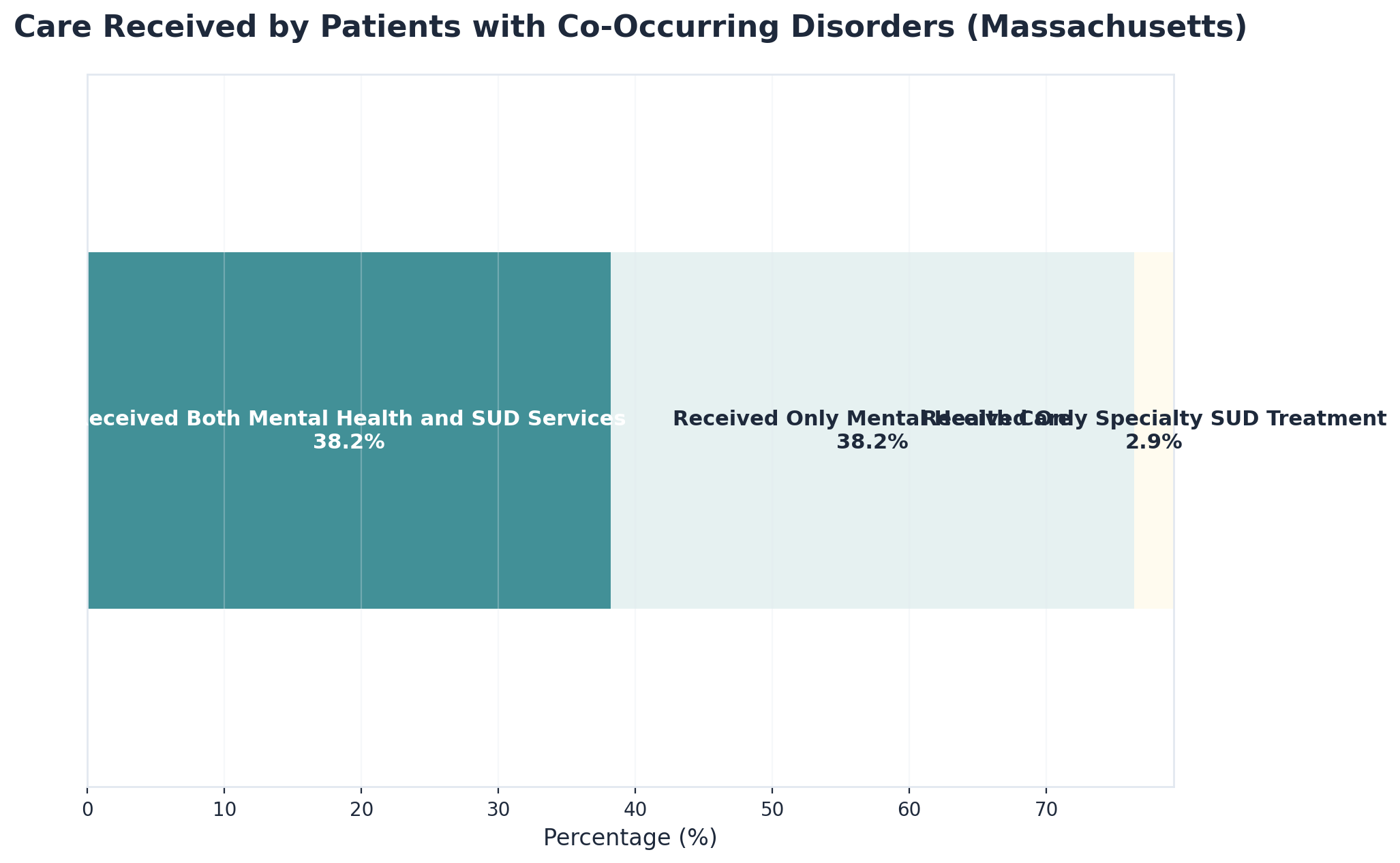
Many individuals seeking recovery experience both substance use challenges and symptoms like anxiety, depression, or PTSD. Virtual addiction treatment and online substance use counseling—now widely available through MassHealth-accepting providers—make it easier to receive care for both conditions from the same team. These integrated models let you meet with therapists and recovery specialists who understand the intersection of mental health and substance use, creating a more seamless and effective recovery path.
Many individuals living with substance use disorder have experienced trauma—whether in childhood, relationships, or other life events. Trauma-informed therapy recognizes how past experiences can impact recovery and works to create a sense of safety and trust in every session. Providers offering virtual addiction treatment and online substance use counseling through MassHealth often use approaches that prioritize empowerment, compassion, and collaboration, helping people feel respected and understood. Research in Massachusetts highlights that integrated care—including trauma-informed therapy—leads to better outcomes for those with co-occurring mental health and substance use challenges5.
Research consistently demonstrates that telehealth addiction services deliver outcomes comparable to traditional in-person treatment. A study published in the Journal of Substance Abuse Treatment found that telehealth interventions for dependency issues achieved retention rates of 65-70%—matching face-to-face programs—with treatment completion rates reaching 58% compared to 57% for in-person care. Notably, 73% of telehealth participants reported higher satisfaction due to increased convenience and reduced stigma, compared to 64% in traditional settings.
People who engage in online therapeutic services benefit from continuous access to care during critical moments. The ability to attend therapy sessions from home eliminates transportation barriers and scheduling conflicts that often lead to missed appointments. A 2022 study in JAMA Network Open found that telehealth participants attended an average of 8.2 sessions compared to 6.4 for in-person treatment, with consistent engagement correlating to 12-month sobriety rates of 48% versus 38% for those with irregular attendance patterns.
Massachusetts residents find that MassHealth coverage makes telehealth addiction services more accessible than ever. The state's Medicaid program covers a wide range of addiction treatment services, including telehealth options that allow people to receive scientifically validated care without financial barriers. Research indicates that telehealth particularly benefits rural residents (who show 40% higher engagement rates), working parents (with 35% better appointment adherence), and individuals with mobility limitations (reporting 52% fewer missed sessions).
Telehealth providers that accept MassHealth can help people recover from addiction through structured treatment plans that include individual counseling, group therapy, medication management, and coordination with other healthcare providers. This integrated approach addresses both dependency issues and concurrent psychiatric conditions, which research shows occur together in approximately 50% of cases. Patient satisfaction scores for telehealth addiction services average 4.3 out of 5, with cost-effectiveness studies showing 30% lower overall treatment costs compared to traditional outpatient programs.
The flexibility of online therapeutic services also supports sustained sobriety beyond initial treatment. People can continue accessing support during transitions back to work, family responsibilities, or other life changes that might otherwise disrupt their healing journey. Six-month sobriety rates for telehealth participants reach 62%, with 12-month rates at 48%—outcomes that match or exceed traditional treatment modalities while providing greater accessibility and continuity of care throughout the recovery journey.
Studies show that virtual intensive outpatient programs and telehealth-based SUD treatment lead to similar abstinence rates and quality of life improvements as traditional rehab at the three-month mark6, 7. Accessing medications for opioid use disorder (MOUD) through virtual care is also linked to a 76% reduction in overdose risk at three months compared to no treatment9. For anyone seeking a rehab that accepts MassHealth, this means that evidence-based virtual addiction treatment and online substance use counseling are not only accessible—they’re genuinely effective for long-term recovery.
Research shows there are no meaningful differences in continuous abstinence rates or quality of life between virtual, hybrid, and in-person intensive outpatient programming at three months post-discharge6, 7. This means individuals participating in virtual addiction treatment or online substance use counseling through a MassHealth-accepting provider can expect outcomes on par with those attending brick-and-mortar rehab. These findings make it clear that choosing a virtual rehab that accepts MassHealth isn’t a compromise—it's a research-backed, flexible path to recovery.
Research shows that receiving MOUD, such as buprenorphine or methadone, is linked to a 76% reduction in overdose risk at three months compared to no treatment—a life-saving benefit for those on the path to recovery9. Virtual addiction treatment and online substance use counseling covered by MassHealth make it easier for people to start and stay with these medications, even if they can’t attend in-person appointments.
Virtual addiction treatment and online substance use counseling do more than provide short-term support—they’re designed to help people build coping strategies, manage triggers at home, and stay connected to recovery resources over time. Research shows that outcomes for virtual care are just as strong as in-person programs at three months, but the real test is sustaining those gains in regular routines6, 7. Many MassHealth-accepting rehabs address this by offering ongoing skills practice, peer recovery coaching, and digital check-ins, which help prevent relapse and support independence.
Virtual addiction treatment programs focus on skills that translate directly to everyday life. For example, providers guide members through role-play exercises for handling cravings, teach stress-reduction techniques like mindful breathing, and offer digital worksheets to practice setting healthy boundaries with family or friends. Ongoing online substance use counseling means you’re not just talking about recovery—you’re actively rehearsing how to respond to challenges in the real world, right where those challenges happen.
Peer recovery coaching is a key part of virtual addiction treatment and online substance use counseling for MassHealth members. These coaches are individuals who have walked their own recovery path and are trained to provide ongoing encouragement, help with goal setting, and practical support through everyday ups and downs. Research out of Massachusetts shows that integrating peer recovery coaches into care models improves continuity and helps individuals stay engaged with recovery resources, even in virtual or community settings19, 22.
Massachusetts residents facing dependency challenges have more accessible pathways to recovery than ever before. MassHealth coverage removes significant financial barriers to evidence-based treatment, while telehealth platforms eliminate logistical obstacles like transportation and scheduling conflicts. For those managing both dependency and concurrent psychological conditions, integrated care approaches offer comprehensive support that addresses the full spectrum of recovery needs.
Virtual treatment platforms have transformed access to professional care, allowing individuals to connect with specialized clinicians from home. This model proves particularly valuable for those balancing recovery with employment, family responsibilities, or geographic limitations. The privacy and convenience of telehealth appointments can reduce the hesitation many people feel about taking that crucial first step toward getting help.
Understanding coverage options, recognizing quality indicators in treatment providers, and knowing what to expect from different therapeutic approaches empowers individuals to make informed decisions about their care. Recovery journeys vary widely, but access to professional support shouldn't depend on financial resources or physical proximity to treatment centers.
For Massachusetts residents ready to explore their options, concrete next steps include verifying MassHealth eligibility and coverage details, researching providers who specialize in dependency treatment and accept MassHealth, and preparing questions for an initial consultation about treatment approaches and what to expect. Many telehealth providers, including Pathfinder, accept MassHealth and offer virtual appointments that fit into diverse schedules and circumstances.
Recovery requires courage, but the barriers to accessing professional support continue to diminish. With comprehensive insurance coverage and flexible treatment delivery models, Massachusetts residents have genuine opportunities to pursue healing and build healthier futures. The resources exist—taking that first step toward exploring them is what transforms possibility into progress.
Many individuals seeking help for addiction have questions about telehealth recovery services and insurance coverage. Understanding how virtual care works and what to expect can help remove barriers to accessing the support needed for lasting recovery.
Yes, Pathfinder Recovery accepts MassHealth insurance for virtual addiction treatment in Massachusetts. This means MassHealth members can access a full range of evidence-based services, including intensive outpatient programs, online substance use counseling, and co-occurring mental health support—all delivered through secure telehealth platforms. Research shows that virtual addiction treatment programs accepting MassHealth provide outcomes comparable to in-person care, making it easier for individuals across the state to get help without travel or long wait times6, 7. If you’re seeking a rehab that accepts MassHealth, Pathfinder’s virtual model is designed to be accessible, flexible, and insurance-friendly for people ready to start their recovery journey.
Yes, at-home detox can be safe when it’s medically supervised by a qualified provider through a program like virtual addiction treatment covered by MassHealth. During at-home detox, clinicians use secure video or phone check-ins to monitor withdrawal symptoms, provide medication support if needed, and respond quickly to any complications. Research shows that outcomes for virtual addiction treatment—including medically supervised detox—are similar to those for in-person care at the three-month mark, meaning people can receive effective, evidence-based support from home6, 7.
Virtual prescriptions for medications like Suboxone (buprenorphine/naloxone) are fully supported under MassHealth for eligible members. Here’s how it works: after a telehealth evaluation with a licensed provider from a rehab that accepts MassHealth, your clinician can prescribe Suboxone electronically. The prescription is sent directly to your preferred pharmacy, where you can pick it up just like any other medication. Research shows that MassHealth’s telehealth policies allow for clinically appropriate, medically necessary medications to be prescribed and managed entirely through secure video or phone visits3.
To participate in virtual addiction treatment sessions with a rehab that accepts MassHealth, all you typically need is a device with internet access—such as a smartphone, tablet, or computer—and a private space where you feel comfortable. Most online substance use counseling and virtual addiction treatment programs use secure video platforms, but many also offer phone-only options if video isn’t possible. MassHealth’s telehealth policy does not require you to have complicated technology or special software; providers are encouraged to work with you to find the simplest, most accessible solution for your situation3.
Yes, family members can participate in your treatment through Pathfinder, even when care is provided virtually and covered by MassHealth. Pathfinder’s programs include options for family or couples counseling as part of their evidence-based virtual addiction treatment and online substance use counseling. Research shows that involving loved ones in recovery can improve communication, strengthen support systems, and lead to better outcomes for individuals in a rehab that accepts MassHealth1.
The length of a typical virtual recovery program with MassHealth coverage can vary depending on your needs and progress, but most intensive outpatient programs (IOPs) last from 8 to 12 weeks, with sessions several times per week. Ongoing online substance use counseling and relapse prevention support may continue for several months or longer, based on personal recovery goals. Research shows that virtual addiction treatment—including programs offered by a rehab that accepts MassHealth—delivers outcomes similar to in-person care at the three-month follow-up, which is a common milestone for measuring early recovery6, 7.
If you need a higher level of care than virtual treatment can offer—such as inpatient detox, residential rehab, or 24/7 medical supervision—your care team will help arrange a safe transition to an appropriate facility that accepts MassHealth coverage. Virtual addiction treatment and online substance use counseling are highly effective for many people, but sometimes medical or safety needs require a more structured setting1, 6. MassHealth covers a full spectrum of substance use disorder services, including inpatient and residential programs, so you won’t lose coverage if your needs change.
No, you will not have to pay copayments for virtual counseling sessions through MassHealth. Since July 2020, MassHealth has waived all copayments for medically necessary opioid use disorder counseling—including individual, group, and family sessions—delivered either in-person or through virtual platforms2, 3. This means that when you choose a rehab that accepts MassHealth, you can access online substance use counseling or virtual addiction treatment without worrying about session fees.
Yes, you can receive medication-assisted treatment (MAT) through virtual care if you have MassHealth. MassHealth covers FDA-approved medications like buprenorphine, methadone, and naltrexone for opioid and alcohol use disorder, and allows these to be prescribed and managed via telehealth appointments with licensed providers1, 3. Virtual addiction treatment programs that accept MassHealth offer MAT alongside online substance use counseling, making it possible to start or continue medication support from home.
To verify your MassHealth benefits cover virtual addiction treatment, start by calling the Member Services number on your MassHealth card or logging in to your online MassHealth account. Ask specifically about coverage for substance use disorder services delivered via telehealth, such as virtual addiction treatment and online substance use counseling. You can also contact the rehab that accepts MassHealth you’re interested in—many providers will confirm your eligibility and walk you through the process.
Yes, research consistently shows that virtual rehab is just as effective as in-person treatment for substance use disorder when delivered by a rehab that accepts MassHealth. Studies reveal there are no meaningful differences in continuous abstinence rates or quality of life at three months post-treatment between virtual, hybrid, and in-person intensive outpatient programs6, 7.
Yes, most people can work full-time while participating in a virtual recovery program through a rehab that accepts MassHealth. Virtual addiction treatment and online substance use counseling are designed with flexible scheduling—sessions can often be booked in the early morning, evenings, or weekends, allowing you to fit care around work and personal commitments. Research shows that these telehealth programs produce outcomes similar to in-person care, even for those balancing jobs, family, and recovery goals6, 7.
No, your employer or colleagues will not be notified that you are receiving addiction treatment through Pathfinder. Virtual addiction treatment programs that accept MassHealth, like Pathfinder, are required by law to protect your privacy and keep your health information confidential. Sessions take place in secure online platforms, and participation is not shared with anyone outside your treatment team unless you give written permission. Studies reveal that virtual addiction treatment and online substance use counseling offer added privacy, making it easier for individuals to seek help without fear of workplace stigma or unwanted disclosure8.
Yes, virtual addiction treatment can be a strong option if you’ve experienced a relapse after traditional rehab. Research shows that virtual intensive outpatient programs and online substance use counseling—offered by a rehab that accepts MassHealth—lead to similar abstinence rates and quality of life improvements as in-person care at three months post-treatment6, 7. Virtual addiction treatment is designed for real life, with flexible scheduling and ongoing support that can help you re-engage with recovery right from home.
Yes, Pathfinder provides support for co-occurring mental health conditions like depression or PTSD as part of its virtual addiction treatment programs for MassHealth members. While Pathfinder does not offer primary mental health care, their team specializes in treating substance use disorder (SUD) with integrated support for co-occurring mental health needs. This means that individuals experiencing both SUD and mental health symptoms receive coordinated care from the same virtual team, which can include therapy and counseling tailored to address both conditions together.

November 6, 2025

November 7, 2025

November 6, 2025