
Online Peer Coaching: Ongoing Virtual Support and Accountability in Recovery
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Navigating the various types of outpatient rehab can feel overwhelming, but the core concept is simple: professional addiction treatment that allows you to live at home. Unlike residential programs that require a 24/7 stay, outpatient care integrates recovery into your daily life. This structure enables you to continue working, attending school, or caring for family while receiving evidence-based treatment.
Treatment + Daily Life = Sustainable Recovery
Outpatient care acts as a bridge, connecting clinical therapy with real-world application. You learn coping skills in a session and apply them immediately in your home environment.
The intensity of care is not "one size fits all." It scales based on your medical necessity and recovery stage. Some individuals start with high-intensity schedules and step down over time, while others may only need weekly check-ins. Treatment typically combines individual counseling, group therapy, and education on the underlying factors of dependency. Crucially, effective programs also address co-occurring mental health conditions—such as anxiety or depression—that often accompany substance use disorders.
What you'll learn: How to determine if outpatient care is safe and appropriate for your current situation.

Before choosing a program, review this checklist. If you answer "Yes" to most questions, outpatient rehab is likely a strong fit.
Research indicates that outpatient care is as effective as inpatient programs when the individual is matched to the correct intensity level1.
The American Society of Addiction Medicine (ASAM) provides the industry standard for matching patients to the right level of care. Think of these levels as "dials" that adjust the volume of support you receive.
The Three Main Outpatient Levels:
Practice This: Look at your calendar. Can you dedicate 3 hours a day, 3 days a week (IOP)? Or do you need full-day support (PHP)? Being realistic about your time availability is the first step in choosing a sustainable program.
Once you understand the foundation, it is time to look at the specific program structures. The following table breaks down the differences between the three primary types of outpatient rehab to help you compare them side-by-side.
| Program Type | Time Commitment | Best Suited For | Key Features |
|---|---|---|---|
| Standard Outpatient | 1–3 sessions/week (< 9 hours) | Individuals with long-term stability or stepping down from IOP. | Focus on maintenance, coping skills, and reintegration. |
| Intensive Outpatient (IOP) | 3–5 days/week (9–19 hours) | Those needing structure but working/schooling full-time. | Group therapy, family sessions, and regular drug testing. |
| Partial Hospitalization (PHP) | 5 days/week (20–30 hours) | Individuals transitioning from detox or inpatient care. | Daily medical monitoring, intensive therapy, skill-building. |
Intensive Outpatient Programs (IOPs) are the "middle ground" of recovery. They typically run for 9-12 hours a week. This format is ideal if you are stepping down from residential treatment but still need accountability. It allows you to maintain your job or education while receiving significant clinical support3.
Partial Hospitalization Programs (PHPs) are the most intensive option. Often called "day treatment," PHP treats addiction with the same clinical rigor as inpatient care but allows you to sleep at home. This is often the recommended starting point for someone with a moderate-to-severe substance use disorder who has a stable home environment but needs daily medical and therapeutic intervention.
Virtual outpatient care removes barriers like transportation and geography. Using secure telehealth platforms, you can access therapy, group support, and medical appointments from home. This is particularly valuable for residents in Vermont, Massachusetts, Connecticut, and New Hampshire, where winter weather or rural distances can make travel difficult.
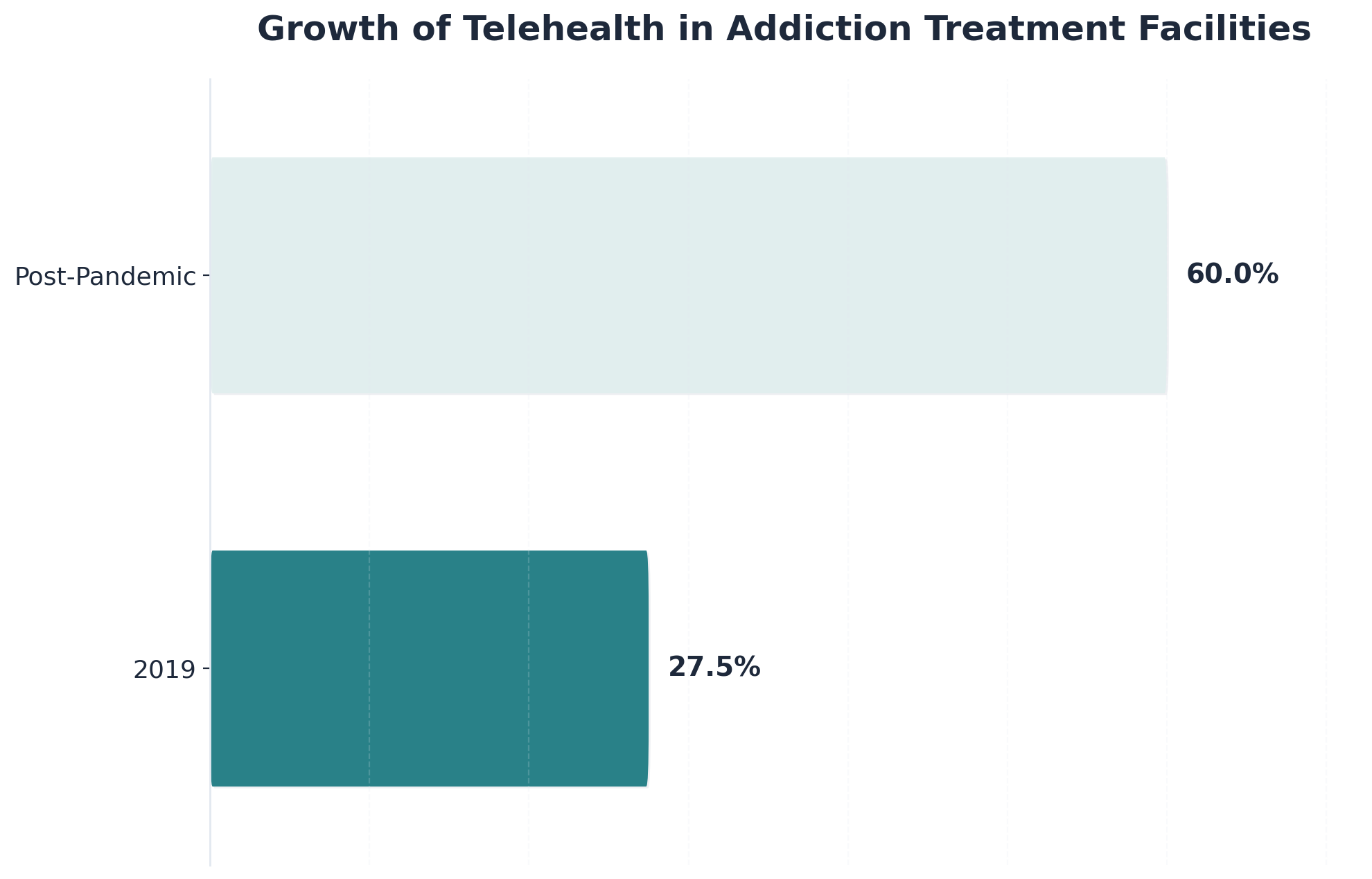
"Over 60% of treatment facilities now offer telehealth services, and industry standards require strict data protection and privacy safeguards." 6
Practice This: Test your tech. Ensure you have a private room, a stable internet connection, and headphones. If you can stream a video, you have the bandwidth for virtual recovery.
Standardized approaches often miss critical factors that influence recovery. Specialized care pathways address unique clinical situations, ensuring that treatment is relevant to your specific life experience and medical needs.
Dual Diagnosis treatment integrates support for addiction with care for co-occurring psychiatric conditions like depression, anxiety, or PTSD. It is critical to treat both simultaneously; treating one without the other often leads to relapse.
Studies indicate that integrated dual diagnosis programs reduce hospitalization rates by 40% compared to treating conditions separately10.
Trauma-Informed Care recognizes that past trauma often drives substance use. These programs create a safe environment where you can process experiences without being re-traumatized. For those in New England, finding a provider who offers co-occurring support alongside SUD treatment is essential for holistic healing.
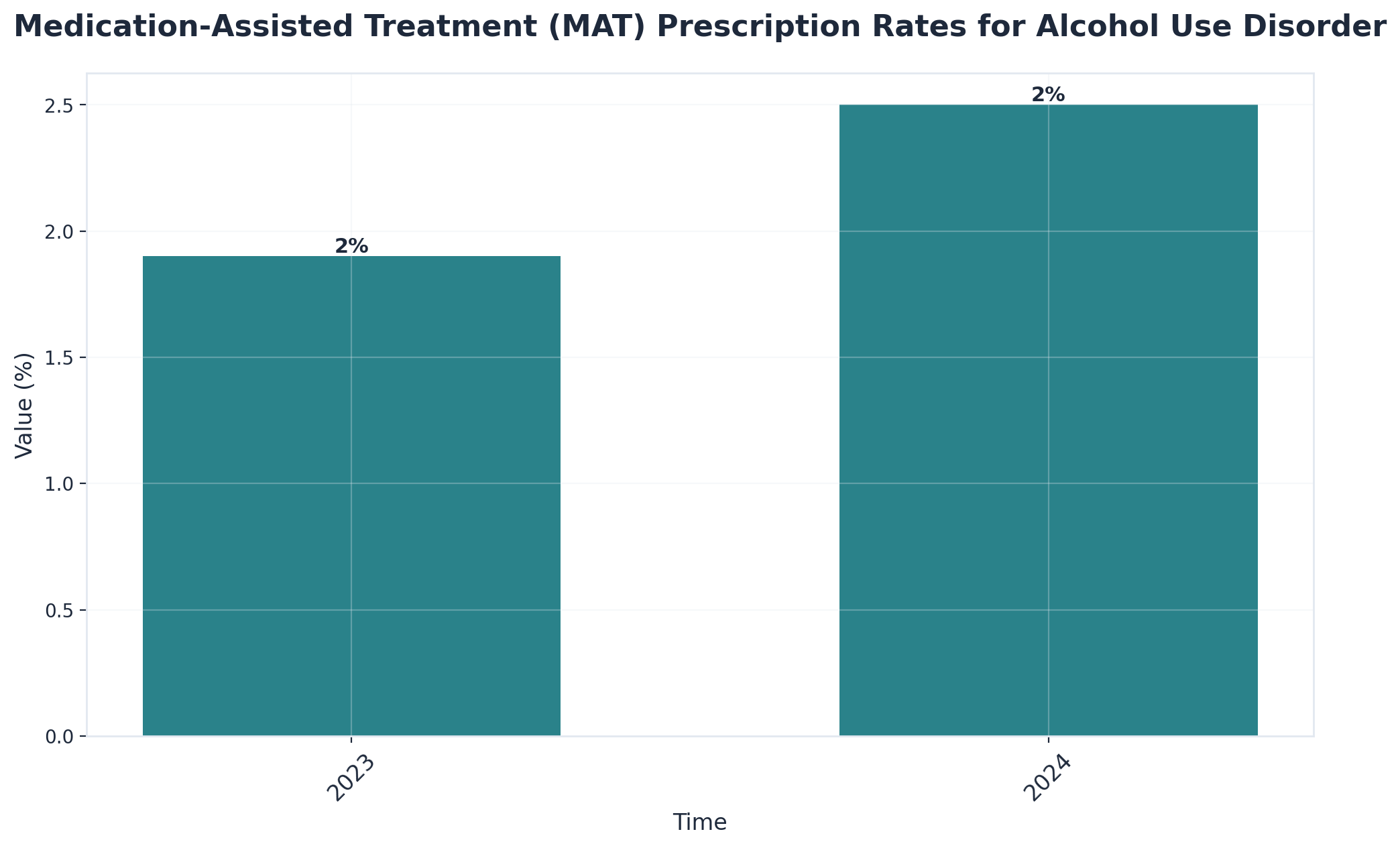
MAT combines FDA-approved medications (like buprenorphine or naltrexone) with counseling. It is the gold standard for treating opioid and alcohol use disorders.
Sample MAT Protocol:
Phase 1: Induction (Days 1-3) - Medical assessment via telehealth - Initial medication dosage - Monitoring for withdrawal symptoms Phase 2: Stabilization (Weeks 1-4) - Weekly medical check-ins - Dosage adjustments - Integration with IOP/PHP therapy sessions Phase 3: Maintenance (Ongoing) - Monthly medical visits - Continued behavioral therapy
Practice This: If you are struggling with opioid or alcohol dependence, ask a provider specifically about their MAT capabilities. It is a medical tool that stabilizes brain chemistry, allowing therapy to take root5.
Choosing the right outpatient addiction treatment program is a strategic decision for your health. Whether you need the high structure of a Partial Hospitalization Program or the flexibility of an Intensive Outpatient Program, the goal remains the same: sustainable recovery in the real world.
For residents of Vermont, Massachusetts, Connecticut, and New Hampshire, virtual options have made these critical services more accessible than ever. By matching the program intensity to your specific needs—and ensuring support for co-occurring mental health conditions—you build a foundation for long-term success.
Yes, many individuals continue working full-time. This flexibility is a core strength of outpatient rehab. Programs, including standard and intensive tracks, are structured around work obligations, often offering sessions in the early morning, evening, or virtually6. Employers can also support this by providing flexible scheduling for telehealth sessions.
Virtual outpatient care uses secure, HIPAA-compliant platforms where health information is encrypted. No sessions are recorded without written consent. You can further protect your privacy by using headphones and choosing a quiet, private room for your sessions.
Relapse is viewed as a clinical setback, not a failure. If it occurs, contact your provider immediately. They will adjust your treatment plan—perhaps increasing session frequency or moving you to a higher level of care like PHP—to help you regain stability without judgment1.
Most major insurance plans, including Medicaid and Medicare, cover telehealth rehab services. This is standard across Vermont, Massachusetts, Connecticut, and New Hampshire. Always verify your specific benefits and copays with your provider before starting.
Transitioning is a planned process called a "step-down." Your care team will help you move from inpatient or PHP to a less intensive IOP or standard outpatient program. This gradual reduction in intensity helps maintain recovery momentum while increasing independence7.
Yes, family participation is highly encouraged. Most programs offer virtual family therapy or education sessions. This allows loved ones to learn how to support your recovery, regardless of where they live4.
You generally need a smartphone, tablet, or computer with a camera and microphone, plus a stable internet connection. Most providers use browser-based platforms that do not require complex software installation.

November 6, 2025

November 6, 2025

November 6, 2025