
Why Choose Telehealth for Addiction Recovery?
December 18, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Understanding what is outpatient treatment begins with the concept of flexible recovery. It is a non-residential approach to substance use disorder care that allows individuals to receive professional support while maintaining their daily responsibilities. Unlike residential or inpatient programs that require living at a treatment facility, this care model lets people attend scheduled counseling appointments and therapeutic activities while continuing to live at home, work, or attend school.
This approach is comparable to physical therapy for an injury—you receive expert clinical support during scheduled sessions but return to your own bed at night. Outpatient programs can serve as a primary step in recovery, a transition from more intensive residential care, or a method for maintaining long-term progress. Studies reveal that outpatient care allows individuals to keep community ties, which is a key part of ongoing recovery success1.
The flexible recovery continuum means that outpatient care adapts based on each person's needs. Instead of a one-size-fits-all approach, individuals might start with intensive treatment and gradually step down to fewer appointments.
| Program Type | Intensity & Structure | Best Suited For |
|---|---|---|
| Partial Hospitalization (PHP) | High Intensity: 5–6 hours/day, 5–7 days/week. | Individuals needing close monitoring and complex symptom management but who have a safe home environment. |
| Intensive Outpatient (IOP) | Moderate Intensity: 9–20 hours/week. | Those balancing recovery with work or family duties who need more than weekly therapy. |
| Standard Outpatient | Lower Intensity: <9 hours/week (e.g., weekly counseling). | Maintenance phase recovery or those with mild symptoms and strong support systems. |
Research confirms that matching the intensity of outpatient addiction treatment to a person’s stage of recovery leads to the best results23. These levels allow treatment to fit a person’s needs as they change over time, creating a flexible path to recovery.
The core components of these programs include individual counseling, group therapy, medication management when appropriate, and skill-building workshops focused on relapse prevention. Most programs begin with a comprehensive assessment to evaluate the severity of addiction and identify co-existing psychological conditions.

A typical week might include individual counseling with a licensed therapist, group meetings to build peer connections, and psychoeducation classes. The schedule adapts to real life rather than replacing it. For example:
IOP session, and return home by early afternoon.Evidence-based therapeutic approaches form the backbone of what is outpatient care. These methods are chosen because research shows they help people make real, lasting changes.
"Studies reveal that up to 60% of patients in CBT-based outpatient addiction treatment programs provided clean toxicology screens at a 52-week follow-up, showing strong long-term results." 14
Key therapies include:
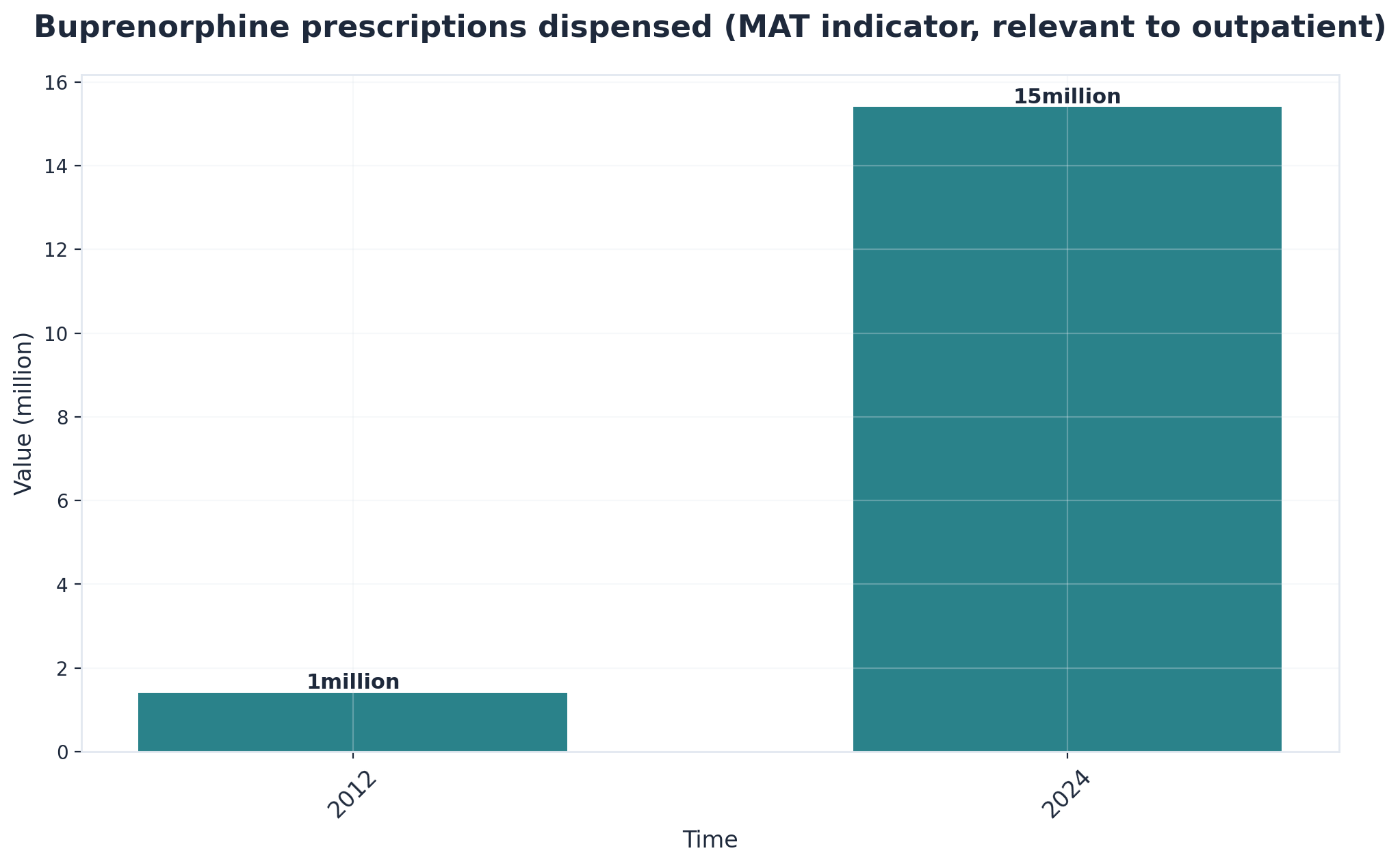
MAT combines FDA-approved medications with counseling and therapy. Medications like buprenorphine, methadone, and naltrexone act like training wheels on a bike: they help stabilize recovery while individuals learn new skills through counseling. Research shows that combining these medications with behavioral support leads to better and longer-lasting recovery outcomes compared to therapy alone5.
With the rise of virtual outpatient care, people can now access prescription management and check-ins online. This setup works a bit like online banking—it lets people manage important health tasks from home while maintaining privacy.
Outpatient treatment has proven highly effective for individuals seeking recovery. A 2020 study published in the Journal of Substance Abuse Treatment found that individuals who completed structured outpatient programs achieved 12-month sobriety rates of 68%, comparable to residential treatment outcomes.
The flexibility of this approach allows individuals to immediately apply recovery skills in real-world situations. Rather than learning coping strategies in isolation, participants face actual triggers and stressors while having professional support readily available. This hands-on practice strengthens recovery skills and builds confidence.
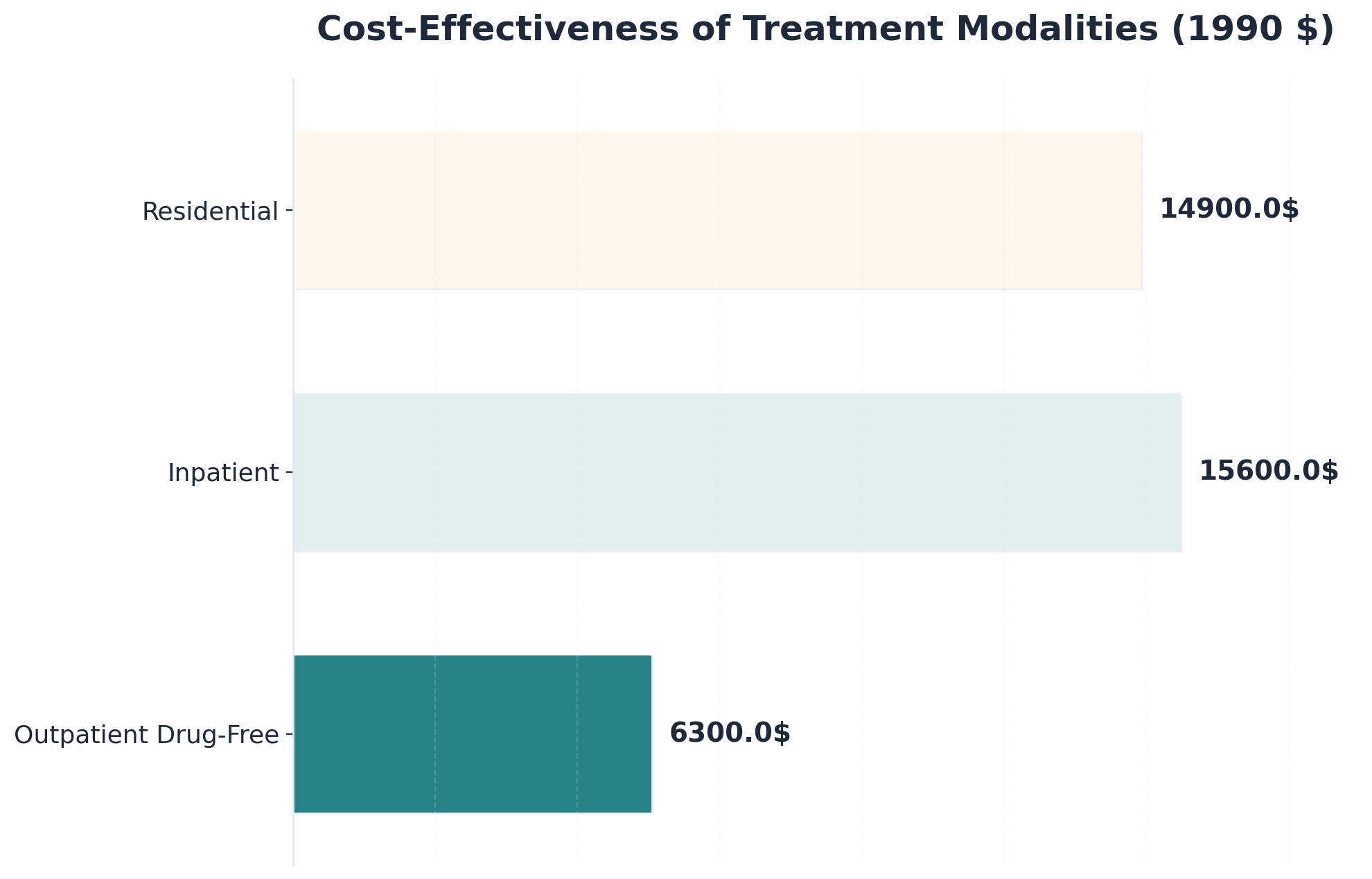
Comparable outcomes at a lower cost are a major reason why what is outpatient care continues to grow in popularity. Research highlights that outpatient drug-free programs cost less than half per successfully treated case compared to inpatient care—approximately $6,300 versus $15,600—while delivering similar results11.
Additionally, maintaining work and family connections is a standout strength. Studies show that being able to remain active in work and family life boosts motivation and treatment retention1, 2.
Outpatient programs are designed to go beyond a generic approach by offering services that address co-occurring mental health conditions, trauma histories, and neurodivergence.
Technology has transformed addiction treatment by removing traditional barriers. Virtual outpatient services now deliver evidence-based treatment directly to individuals in their homes. This is particularly valuable for Pathfinder's service areas in Vermont, Massachusetts, Connecticut, and New Hampshire, where rural geography can otherwise limit access to specialized care.
Evidence from healthcare systems implementing telehealth addiction treatment indicates that virtual services can achieve outcomes comparable to in-person sessions. The key difference lies in accessibility—virtual platforms can reach individuals who might otherwise go without treatment due to geographic or logistical constraints.
With secure video calls and online platforms, individuals can now meet with therapists, doctors, or support groups right from home. This shift makes outpatient addiction treatment as easy to access as online shopping or virtual school.
Research-backed evidence shows that virtual outpatient care stands toe-to-toe with traditional, in-person treatment. Patients report similar satisfaction, engagement, and recovery rates17. Furthermore, virtual care helps overcome privacy barriers; with secure video sessions, individuals can seek support without worrying about being seen entering a clinic.
Outpatient addiction treatment doesn’t simply end after the last therapy session. Ongoing support like aftercare planning, alumni programs, and peer recovery groups play a key role. Studies show that relapse rates after formal treatment are between 40% and 60%, similar to other chronic health conditions like diabetes31.
Virtual outpatient programs make it easier to stay connected with counselors and peer mentors for ongoing encouragement and accountability, bridging the gap between formal care and community life.
While virtual care expands access to treatment, selecting the right program requires a systematic evaluation process. Consider these key factors:
IOP, PHP, or standard care.Choosing a recovery program raises many questions. Understanding what to expect can help individuals and families make more informed decisions about their care journey.
Yes, many people continue working full-time while participating in what is outpatient treatment for substance use disorder. Outpatient addiction treatment is specifically designed to fit around daily responsibilities, including employment. Scheduling is often flexible, with sessions offered in the evenings, early mornings, or even virtually. Studies show that maintaining work and family connections is a key strength of outpatient care—being able to stay active in your job can boost motivation and help you stick with treatment1, 2.
Virtual outpatient treatment is shown to be just as effective as traditional in-person care for substance use disorder. Research comparing online and face-to-face outpatient programs found no difference in patient satisfaction, substance use outcomes, or how well people stayed engaged with therapy17. This means that people choosing virtual outpatient addiction treatment can expect results similar to those attending in-person sessions.
Virtual outpatient treatment is designed to protect your privacy, so your employer or colleagues will not be notified that you are attending unless you choose to share that information. Sessions are held on secure telehealth platforms, and all communication is confidential. Research shows that concerns about privacy are common, but telehealth makes it easier for individuals to access what is outpatient care without being seen entering a clinic17.
If a relapse happens during or after what is outpatient treatment, it's important to remember that this is a common part of the recovery process. Studies show that between 40% and 60% of individuals experience a relapse after formal treatment31. Outpatient addiction treatment programs are designed to help people get back on track—providers can adjust the treatment plan, offer additional support, or recommend a different level of care if needed.
Yes, outpatient treatment can work well for people with co-occurring mental health conditions, as long as the program is designed to support both substance use disorder and mental health challenges together. Research shows that about 6.7% of adults have both a substance use disorder and a co-occurring mental illness, and individuals do best when these issues are treated at the same time33.
Outpatient treatment is typically much more affordable than inpatient rehab. Studies reveal that the cost per successfully treated case in an outpatient addiction treatment program is about $6,300, while inpatient programs can cost around $15,600 for the same outcome—less than half the price11. Research also shows that outpatient care can offer overall savings of 17% to 60% compared to inpatient services10.
Yes, you can receive medication-assisted treatment (MAT) through a virtual outpatient program. Modern outpatient addiction treatment often includes virtual options for medication management via secure video calls. Studies reveal that telehealth-based prescription management is just as safe and effective as in-person visits, offering high satisfaction and expanding access to care7.
Yes, outpatient treatment can be a strong option for someone who has been through rehab before and experienced a relapse. What is outpatient care allows individuals to re-engage with therapy, peer support, and medication-assisted treatment while staying involved in daily life. Many programs include relapse prevention strategies and aftercare planning to help rebuild progress.
Deciding between Partial Hospitalization Programs (PHP), Intensive Outpatient Programs (IOP), or standard outpatient care depends on your personal needs. PHP offers the most structured support (5+ hours/day), IOP is less intensive (9-20 hours/week), and standard outpatient care typically involves fewer than nine hours per week. Studies reveal that matching the intensity of outpatient addiction treatment to your recovery stage leads to the best results23.
Yes, many outpatient programs are thoughtfully adapted for neurodivergent individuals. What is outpatient care often involves flexible therapy options, sensory-friendly environments, and communication styles that meet a wide range of needs. Studies reveal that tailoring care to support neurodiversity leads to better engagement and improved outcomes in recovery33.
Yes, family members can often participate in your outpatient treatment. Outpatient addiction treatment frequently includes family therapy sessions or educational groups. Studies reveal that including family in what is outpatient care strengthens relationships and provides a stronger support system, which can improve recovery outcomes1, 2.
Pathfinder serves individuals in Vermont, Massachusetts, Connecticut, and New Hampshire with virtual outpatient treatment for substance use disorder and co-occurring mental health needs. Virtual care makes what is outpatient treatment more accessible by allowing people to attend therapy from home, which research shows helps break down barriers to care7, 17.
For most people, detoxing from drugs or alcohol at home is not considered safe unless a medical provider has specifically approved it. Research shows that outpatient detoxification can be safe only for individuals with mild to moderate withdrawal symptoms who have a stable home environment2, 23. If someone is at risk for severe withdrawal, inpatient detox is usually needed.
Most insurance plans, including many private and public options, do cover virtual outpatient treatment for substance use disorder. Coverage usually includes services delivered through secure video calls. Studies reveal that cost and insurance coverage remain important factors in accessing what is outpatient care16, 1.
Navigating the journey of recovery requires dedication, support, and access to the right resources. Throughout this guide, we've explored the essential components of effective addiction treatment, from understanding evidence-based approaches to recognizing the importance of integrated care for concurrent psychiatric conditions. Recovery is not a one-size-fits-all process, and finding treatment that addresses individual needs makes all the difference in achieving lasting wellness.
The landscape of addiction treatment continues to evolve, with virtual care options expanding access to quality support for individuals who might otherwise face barriers to treatment. Telehealth services have opened new pathways to recovery, allowing people to receive comprehensive care while maintaining their daily responsibilities and staying connected to their support networks.
The first step is to reach out for a confidential consultation with a licensed treatment provider who can assess your unique situation and recommend appropriate care options. Whether you're exploring outpatient therapy, medication-assisted treatment, or comprehensive psychiatric support, professional guidance will help you identify the approach that best fits your needs and circumstances.

December 18, 2025

November 6, 2025

November 6, 2025