
Depression And Brain Fog: Virtual Care That Breaks Barriers and Builds Futures
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
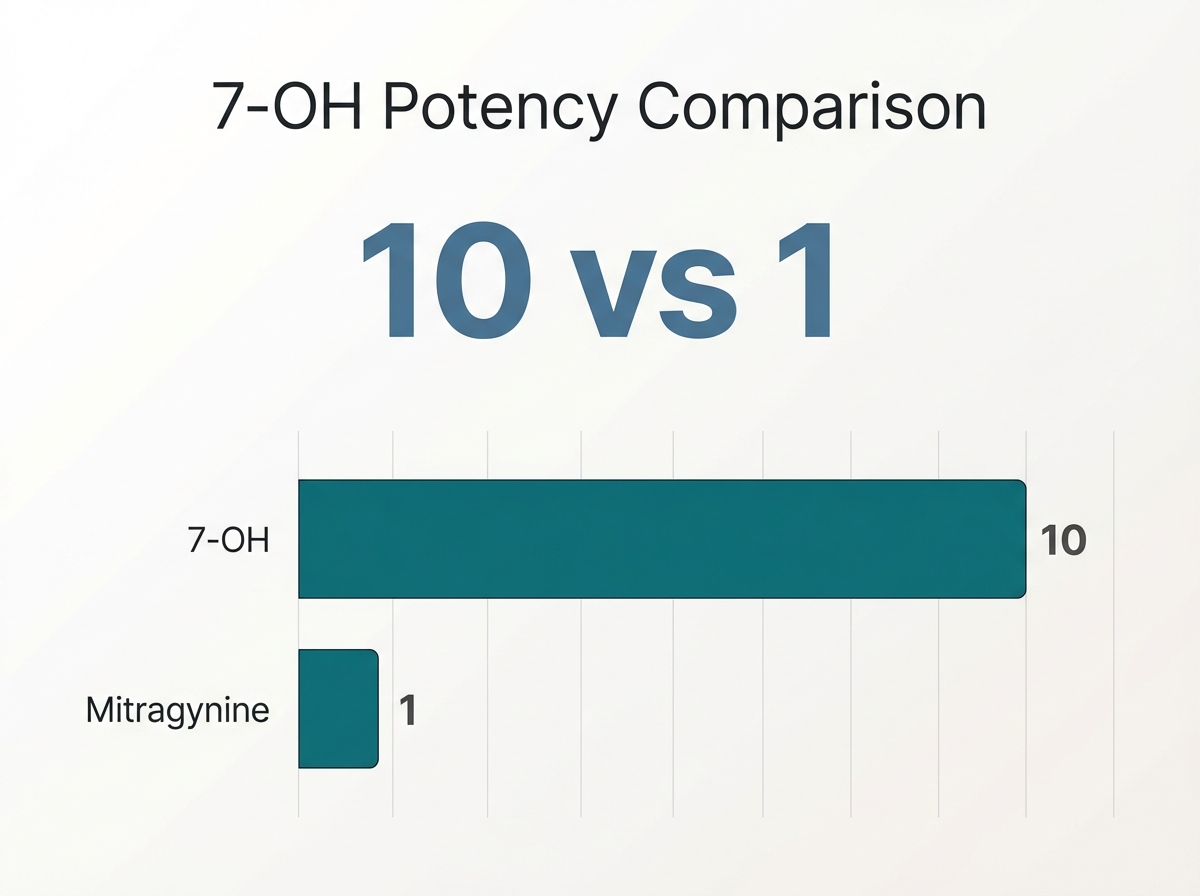
7-hydroxymitragynine listed as an isolated ingredient or in concentrations above 2%, you are dealing with a high-potency product, not traditional kratom. You might have seen products labeled "7-OH" at your local smoke shop or gas station, often marketed as a stronger version of kratom. However, the 7-OH dangers associated with this potent alkaloid are distinct and serious. While the kratom plant naturally contains trace amounts of 7-hydroxymitragynine, manufacturers have developed concentrated forms that are significantly more powerful. These versions can be up to ten times stronger than standard kratom extracts, creating effects that more closely resemble synthetic opioids than the plant's natural form.
What makes 7-OH particularly concerning is its mechanism of action in your brain. It binds to the same opioid receptors targeted by prescription painkillers and illicit opioids. This produces similar euphoric effects but carries comparable risks for dependence. Unlike whole-leaf kratom, which contains a balance of multiple alkaloids, concentrated products deliver an intense, isolated effect that significantly increases the potential for misuse.
The alkaloid's popularity has surged dramatically, particularly among people seeking alternatives to regulated substances or those attempting to manage chronic pain without medical supervision. Because federal regulation is currently limited, manufacturers can produce 7-OH in varying concentrations without standardized testing. This leads to unpredictable potency and increased health risks for you as the consumer.
Emergency departments across the country have documented cases involving people experiencing severe withdrawal symptoms, overdose-like reactions, and complications from combining the alkaloid with other drugs. For those struggling with dependence, professional treatment programs that address both substance use and concurrent mental health concerns can provide comprehensive support for recovery.
It is vital to understand how a natural leaf is transformed into a synthetic concentrate to grasp the risks involved. Kratom leaves naturally contain a wide mix of plant compounds, but only tiny amounts of 7-hydroxymitragynine—typically less than 0.04% by weight. In commercial labs, manufacturers extract and boost this single component.
Imagine squeezing a single orange for juice versus pouring a bottle of pure chemical orange flavoring—one is subtle, the other is overwhelming. This chemical concentration is what puts 7-OH dangers at the center of public health warnings, since the resulting products behave more like synthetic opioids than herbal teas.3, 7
To help you visualize the difference, here is a comparison of natural kratom versus the lab-concentrated 7-OH products found on shelves today:
| Feature | Natural Kratom Leaf | Concentrated 7-OH |
|---|---|---|
| 7-OH Content | Trace amounts (< 0.04%) | Highly concentrated (up to 100x higher) |
| Onset of Effects | Gradual, milder | Rapid, intense rush |
| Risk Profile | Lower risk of acute overdose | High risk of respiratory depression & seizure |
This stark contrast is why public health officials are concerned. Products made with concentrated 7-OH can trigger rapid dependence, accidental overdose, and a much higher risk of severe side effects compared to traditional kratom use.3, 7
Manufacturers use lab techniques to isolate and boost 7-hydroxymitragynine, creating a dose that can be dozens of times more powerful than the plant itself. Industry reports show that these concentrated formulas can make 7-OH act more like a prescription opioid than a herbal supplement. Studies reveal that such products have caused a surge in poison control calls and documented fatal overdoses, especially among young adults.2, 3
Think of your brain’s opioid receptors as locks, and 7-OH as a highly specialized key. While natural kratom is a key that turns the lock slowly, 7-OH is a master key that throws the door wide open instantly. Studies show that 7-OH’s binding affinity at the mu-opioid receptor is 14 to 22 times greater than morphine.3, 7
7-OH acts as a full agonist, meaning it maximizes the opioid response at very low doses. This extreme potency explains why 7-OH dangers, such as overdose and rapid physical dependence, are so much higher than with typical kratom use. It is not just a "stronger tea"; it is a chemically distinct interaction with your biology.
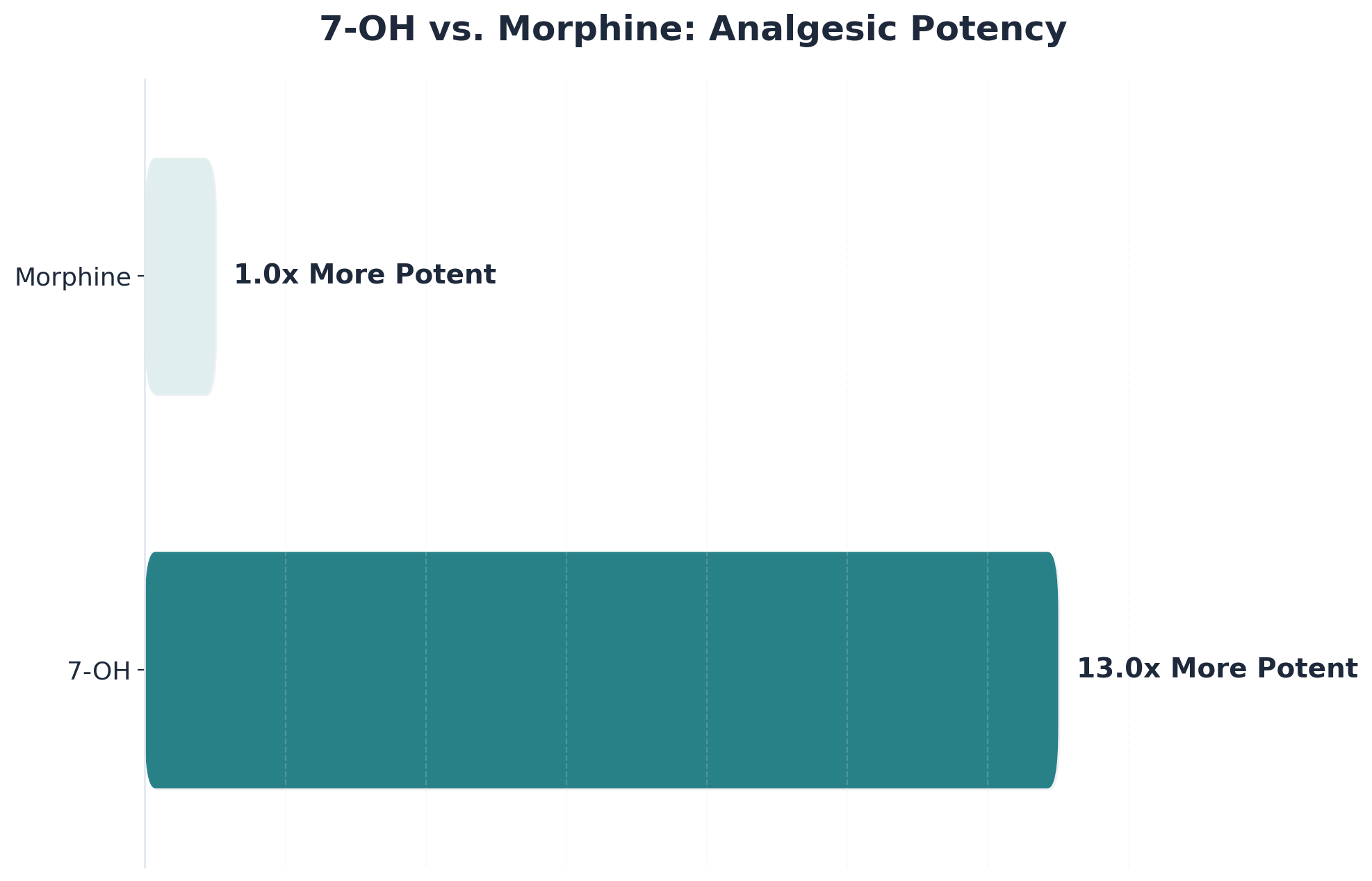
Unlike traditional kratom, which contains a blend of alkaloids that can buffer effects, 7-OH is a purified compound. Research shows that 7-OH is about 13 times more potent than morphine in pain relief and 10 times more potent than mitragynine. These opioid-mimicking properties are what put 7-OH risks at the forefront of health alerts.
The emergence of 7-hydroxymitragynine in concentrated form has raised significant alarm among toxicologists. While traditional kratom products contain approximately 0.01-0.04% of this alkaloid by weight, synthetic versions can contain concentrations 10 to 100 times higher. This dramatic increase in potency translates directly to heightened risks for you.
Research published in clinical toxicology journals has documented severe adverse effects. Respiratory depression—a potentially fatal slowing in breathing patterns—occurs at rates comparable to traditional opioids. Emergency departments across the Northeast have reported a 340% increase in cases between 2019 and 2022 where patients presented with seizures, loss of consciousness, and cardiac arrhythmias after consuming high-potency products.
"Its interaction with mu-opioid receptors in brain tissue creates dependency patterns that mirror prescription opioid addiction, with users developing tolerance within 2-4 weeks."
Physical consequences extend beyond acute intoxication. Prolonged consumption has been linked to liver damage, with elevated enzyme levels indicating hepatotoxicity in approximately 18% of regular users. Gastrointestinal complications, including severe constipation and nausea, occur in an estimated 60-70% of chronic users.
Unlike the slower effects of natural kratom, concentrated 7-OH products can cause seizures, confusion, and loss of consciousness by overstimulating the central nervous system. On the respiratory side, research shows that 7-OH acts as a powerful opioid, depressing breathing even at low doses.3, 7
Lab-concentrated 7-OH can overwhelm the brain’s electrical activity. This overstimulation may result in seizures—sudden bursts of abnormal brain signals that can cause convulsions. Researchers have documented cases where people using synthetic kratom derivatives experienced severe neurological symptoms, including tonic-clonic seizures and episodes of prolonged disorientation.3, 6
When 7-OH binds powerfully to mu-opioid receptors in the brainstem, it slows and can even stop the body’s automatic drive to breathe. Studies show that 7-OH produces respiratory depression with more than three times the potency of morphine. Public health records confirm multiple fatal overdoses in young, otherwise healthy adults, making this one of the most critical 7-OH dangers.2, 3, 7
Research shows that concentrated 7-OH products are linked to liver toxicity—including jaundice, acute hepatitis, and even liver failure in rare cases. These organ-specific risks set 7-OH apart from traditional kratom, which is far less likely to cause such severe metabolic side effects.3, 10
The liver is responsible for breaking down toxins, but the high potency of synthetic 7-OH can overwhelm these defense systems. Studies and case reports have documented severe liver toxicity in people using these products, with symptoms such as yellowing of the skin, dark urine, and abdominal pain.3, 10
Because 7-hydroxymitragynine acts as a full agonist at mu-opioid receptors, it can rewire the brain’s reward system after just a short period of use. Research shows that individuals exposed to concentrated 7-OH products report strong urges to keep using and experience withdrawal symptoms such as anxiety, muscle aches, and insomnia when they stop.3, 7
The market for this concentrated alkaloid has expanded dramatically since early 2022. What began as a niche product has evolved into an industry generating an estimated $150-200 million annually. The surge in popularity stems partly from the compound's legal status in most states, creating a perception of safety that doesn't align with emerging evidence.
Social media influencers and online communities have amplified the reach of these concentrated kratom products. Google Trends data indicates a 340% increase in searches for the alkaloid between January 2022 and December 2023. This digital marketing ecosystem has proven especially effective at reaching younger demographics who may be unaware of the compound's addictive potential.
7-hydroxymitragynine gummies, shots, and vapes are now common in gas stations, smoke shops, and widely available online. Studies show that this widespread accessibility has led to a spike in documented poisonings and overdoses, particularly as these products often mimic harmless supplements but act far more like potent opioids.2, 3
The sheer spread of synthetic kratom availability means 7-OH products no longer require a specialty shop. Gas stations and smoke shops now routinely stock these concentrated substances right next to snacks, making them easy for anyone to buy without much scrutiny. Online, the situation is even more concerning: a simple search opens up dozens of vendors shipping directly to homes, often with minimal age verification.
Companies selling synthetic kratom derivatives often use colorful packaging, candy-like flavors, and influencer partnerships to appeal to teens and young adults. These products are frequently advertised as "natural" or "wellness boosters," masking their true opioid-like risks. Research shows that this targeted advertising is directly linked to increased calls to poison control centers.2, 3
As 7-hydroxymitragynine products rapidly spread, the FDA issued warning letters to companies selling these potent derivatives and formally recommended that 7-OH be classified as a Schedule I controlled substance. This move reflects deep concern over documented poisonings and fatal overdoses.1, 2, 3
In June 2025, the FDA sent warning letters to several companies selling 7-hydroxymitragynine gummies, shots, and vapes, citing their opioid-like potency. Soon after, the agency formally recommended that 7-OH be classified as a Schedule I controlled substance—the strictest federal category, typically reserved for drugs with no accepted medical use and high abuse potential.1, 3
Health departments in places like Texas and Los Angeles County have released formal advisories after seeing spikes in poison control calls and severe illness. These warnings often outline the symptoms of opioid-like toxicity and call for stricter monitoring of market proliferation at local retailers.2, 4
As 7-hydroxymitragynine use continues to rise, the good news is that effective treatment options already exist. The pharmacological profile of 7-OH—with its strong opioid receptor activity—means that people experiencing problematic consumption can benefit from comprehensive addiction treatment that addresses both physical dependence and psychological factors.
Medication-assisted treatment (MAT) represents the gold standard for opioid-related dependencies. Medications like buprenorphine and naltrexone can help manage withdrawal symptoms and cravings while people work on underlying recovery issues. Studies show that MAT reduces opioid use by approximately 50% and significantly decreases overdose risk.
Pathfinder Recovery provides virtual outpatient treatment for people throughout the Northeast who are navigating addiction challenges. We serve individuals in Vermont, Massachusetts, Connecticut, and New Hampshire, offering evidence-based interventions tailored to your specific needs.
MAT uses opioid-blocking or stabilizing medications to target the same brain receptors hijacked by high-potency 7-OH. This approach is a proven response to opioid use disorder treatment, reducing the risk of fatal overdose and supporting safer withdrawal. Research shows MAT can decrease overdose deaths by up to 76% within three months.1
Buprenorphine acts as a partial opioid agonist—binding to the same receptors hijacked by 7-hydroxymitragynine but with a ceiling effect that lowers overdose risk. Methadone, a full agonist, is used in carefully monitored doses to stabilize cravings. For people exposed to synthetic kratom derivatives, these MAT approaches help block the intense cravings and withdrawal symptoms that come with 7-OH’s opioid-like potency.1
Research confirms that individuals who receive MAT experience a 76% reduction in overdose mortality at three months compared to those who go without treatment. This powerful outcome highlights why opioid use disorder treatment protocols are so critical for those exposed to potent synthetic kratom products.1
Evidence shows that opioid use disorder treatment is most effective when behavioral support is included alongside medication. Virtual recovery support—delivered through secure video or phone—removes barriers like travel time or stigma, making it easier for people in Vermont, Massachusetts, Connecticut, and New Hampshire to get help from home.1
Many people impacted by synthetic kratom products have histories of trauma or identify as neurodivergent. Trauma-informed care starts by acknowledging that past experiences can shape reactions to withdrawal. Likewise, neurodivergent support means adapting care for people with ADHD, autism, or sensory differences—such as offering flexible session formats and clear communication.1
Pathfinder’s approach starts with a thorough intake and assessment by licensed clinicians. We develop a care plan that may include buprenorphine or methadone for opioid withdrawal, plus ongoing behavioral therapy. Unlike many programs, Pathfinder offers flexible telehealth sessions and peer support groups, so you can access help from your own home in New England.1
The emergence of 7-hydroxymitragynine as a concentrated kratom extract has introduced significant new risks to those seeking pain relief or managing addiction. While traditional kratom products contain relatively low concentrations of this potent opioid agonist, modern extraction techniques have created products where this alkaloid's levels can be 10 to 1,000 times higher than naturally occurring amounts. This dramatic increase in potency has led to a corresponding rise in adverse events, including respiratory depression, seizures, and fatal overdoses.
The convergence of these factors—unregulated production, aggressive marketing, and consumers seeking natural alternatives—has created a perfect storm of public health risk. Products with opioid-like effects strong enough to create physical dependence are being sold alongside dietary supplements, often without adequate safety warnings or dosage guidance. The lack of standardization means that even experienced users cannot reliably predict the strength of what they purchase, transforming what some perceive as a benign botanical into a substance with genuine addiction potential.
For those struggling with kratom dependence or use of potent extracts, specialized treatment can address both the physical aspects of withdrawal and the underlying factors that contribute to substance use. Pathfinder Recovery provides virtual outpatient services that recognize recovery as a comprehensive process—one that involves developing healthy coping strategies, addressing concurrent psychiatric challenges, and building sustainable support systems tailored to individual needs.
As concentrated kratom extracts become more prevalent, informed decision-making becomes increasingly critical. The gap between public perception of kratom as a harmless botanical and the clinical reality of 7-hydroxymitragynine's opioid effects represents a significant public health challenge. Moving forward, greater awareness, clearer regulation, and accessible treatment options will be essential to protecting individuals from the risks these potent extracts present—and empowering those affected to seek the support they need for lasting recovery.
As this potent kratom alkaloid continues to gain popularity, many individuals and families have questions about its risks. Understanding the facts about this concentrated compound can help people make informed decisions about their health.
Yes, someone can overdose on 7-OH even if they have previously used traditional kratom with no problems. The main reason is that 7-hydroxymitragynine (7-OH) is dramatically more potent—studies show it can be up to 13 times more powerful than morphine and about 10 times more than natural kratom’s main alkaloid, mitragynine.3, 7 This means a dose that felt safe with plant-based kratom could cause severe opioid-like toxicity, including respiratory depression or fatal overdose, with concentrated 7-OH products.
Physical dependence on 7-OH products can develop much faster than with traditional kratom or many other opioids. Research shows that because 7-hydroxymitragynine is a full agonist at the mu-opioid receptor, the brain’s reward system can adapt in just a few days of repeated use.3, 7 People may notice opioid use disorder symptoms—like cravings, increased tolerance, and withdrawal symptoms—within a week or even sooner.
Yes, naloxone (Narcan) can usually reverse a 7-OH overdose, but there are important caveats. Since 7-hydroxymitragynine binds mu-opioid receptors very powerfully, higher or repeated doses of naloxone may be needed to fully reverse life-threatening breathing suppression.3, 7 It is crucial to call 911 for any suspected overdose, even if Narcan is available.
Yes, you can receive treatment for 7-OH use without having to take time off work, thanks to the flexibility of virtual recovery support. Pathfinder Recovery offers telehealth-based care for substance use disorder and co-occurring mental health needs, allowing individuals to schedule appointments outside of traditional business hours and access sessions from home.1
Yes, Pathfinder Recovery accepts most major insurance plans for treatment of substance use disorder—including care for those affected by 7-OH dangers. This means that individuals seeking help for synthetic kratom risks can often use their health insurance to cover medication-assisted treatment, behavioral therapy, and virtual recovery support.1
Pathfinder Recovery currently provides virtual treatment for substance use disorder and co-occurring mental health needs to individuals living in Vermont, Massachusetts, Connecticut, and New Hampshire. This telehealth approach means that people in these states can access evidence-based care from the comfort and privacy of their own home.1
Withdrawal from 7-OH is often more rapid, intense, and unpredictable compared to withdrawal from prescription opioids. This is because 7-OH acts as a full agonist at mu-opioid receptors with much higher potency—up to 13 times that of morphine—leading to quicker physical dependence.3, 7 People may experience classic opioid withdrawal effects alongside rebound neurological symptoms, such as confusion or agitation.
Detoxing from 7-OH at home with medical supervision is sometimes possible, but it comes with significant risks due to the compound’s high potency. Medical professionals often recommend that individuals attempting to stop synthetic kratom use do so with close oversight, ideally through a formal virtual or outpatient detox program to manage severe withdrawal and respiratory risks.1, 3
Legal status doesn’t mean a product is safe. Research confirms that 7-OH is up to 13 times more potent than morphine and has caused fatal overdoses and rapid physical dependence.2, 3, 7 Gently sharing facts—like FDA warnings and the difference between plant-based kratom and these concentrated products—can help your loved one understand why caution is needed.
Yes, Pathfinder Recovery offers support for families and loved ones. While the primary focus is on treating the individual's substance use disorder, families are included through education, communication strategies, and optional participation in therapy sessions (with consent).1
Virtual treatment platforms like Pathfinder Recovery use secure, encrypted video and messaging systems that meet strict healthcare privacy laws (such as HIPAA). Records are stored securely and only accessible to authorized clinical staff.1
Yes, medication-assisted treatment (MAT) is considered highly effective for dependence on 7-OH. Medications like buprenorphine and methadone directly target the same opioid receptors that 7-hydroxymitragynine activates, helping to manage cravings and prevent severe withdrawal symptoms.1
Pathfinder Recovery offers a flexible virtual-first care model. Accommodations can include extra time for processing information, clear written summaries after sessions, or video calls with reduced visual distractions. Providers are trained in trauma-informed and neurodivergent accommodations.1
Yes, Pathfinder Recovery specializes in supporting people navigating both substance use disorder and co-occurring mental health challenges. Licensed clinicians develop integrated care plans that combine medication-assisted treatment, behavioral therapy, and support for mental health needs.1

November 6, 2025

November 7, 2025

February 5, 2026