
Navigating Depression in Recovery
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Virtual treatment for addiction represents a fundamental shift in how individuals access recovery support. Rather than requiring daily commutes to physical facilities, these programs deliver evidence-based care through secure video platforms, mobile apps, and digital communication tools. For those asking does online rehab work, the answer lies in the data: participants can attend therapy sessions, group meetings, and educational workshops from their homes, workplaces, or any private location with internet access, often with retention rates matching or exceeding traditional care.
The core components mirror traditional treatment approaches but are adapted for digital delivery:
Technology enables features that enhance accountability and support between sessions. Some platforms include daily check-ins, medication tracking, and crisis resources available 24/7. Digital tools can monitor progress through self-assessments and provide immediate access to coping techniques during challenging moments. This continuous connection helps fill gaps that traditionally existed between weekly appointments.
Remote recovery platforms typically offer varying levels of care intensity. Intensive outpatient programs might require 9-12 hours of weekly participation, while standard outpatient care involves fewer hours. This flexibility allows treatment to adapt as recovery progresses, scaling up during difficult periods or stepping down as stability increases.
Online addiction treatment is defined by its delivery of substance use disorder support through digital platforms—think secure video sessions, phone calls, and interactive apps. What makes this approach distinct is its flexibility: participants can access therapy, group sessions, and medication management from the comfort of their own home or any private space with an internet connection.
"Studies reveal that people often feel more comfortable and empowered when treatment fits their lifestyle and privacy preferences."7
LSI keywords such as "virtual recovery programs" and "telehealth addiction services" describe these models well. Unlike traditional settings, online treatment often provides 24/7 access to resources and support, personalized digital tools, and the ability to reach licensed clinicians across state lines.
Core components of virtual care models include secure video therapy sessions, digital medication-assisted treatment, online group counseling, and interactive self-help resources. These pieces are woven together in telehealth addiction services to offer real-time and on-demand support. Secure video calls allow individuals to connect with licensed clinicians, while apps and web portals deliver reminders, educational content, and progress tracking.
Practice This:
Tool Checklist: [ ] Appointment Reminders [ ] Mood/Craving Trackers [ ] Secure Messaging with Clinicians
Skill Checkpoint: You’re ready for the next level when you can describe how these elements combine to answer the question, does online rehab work, and explain at least two features that promote engagement or abstinence in telehealth addiction services.34
Telehealth stands apart from in-person rehab in several meaningful ways. First, virtual care brings flexibility—sessions can fit around work schedules or family obligations, and location is no longer a barrier. Many people in rural New England or those without transportation find this especially valuable. Second, telehealth addiction services often offer increased privacy and discretion.
However, there are trade-offs. Some individuals miss the structure and social connection of a physical rehab environment, and technological issues—like unstable internet or lack of a private space—can limit participation for others.
Multiple large-scale studies show that telehealth addiction services are not just convenient—they deliver results equal to or better than traditional models. For example, one major review found that virtual care achieves abstinence rates and substance use reductions comparable to in-person treatment.3
| Metric | Virtual Outcome | In-Person Outcome | Key Insight |
|---|---|---|---|
| Retention (30 Days) | 80% Engagement | 50-68% Engagement | Virtual care often retains patients longer due to reduced barriers.4 |
| Opioid Overdose Reduction | 36% Reduction | Baseline | Starting buprenorphine online significantly reduces overdose risk.5 |
| Dropout Rates (CBT) | 25% Dropout | 50% Dropout | Web-based CBT keeps neurodivergent and general populations engaged.6 |
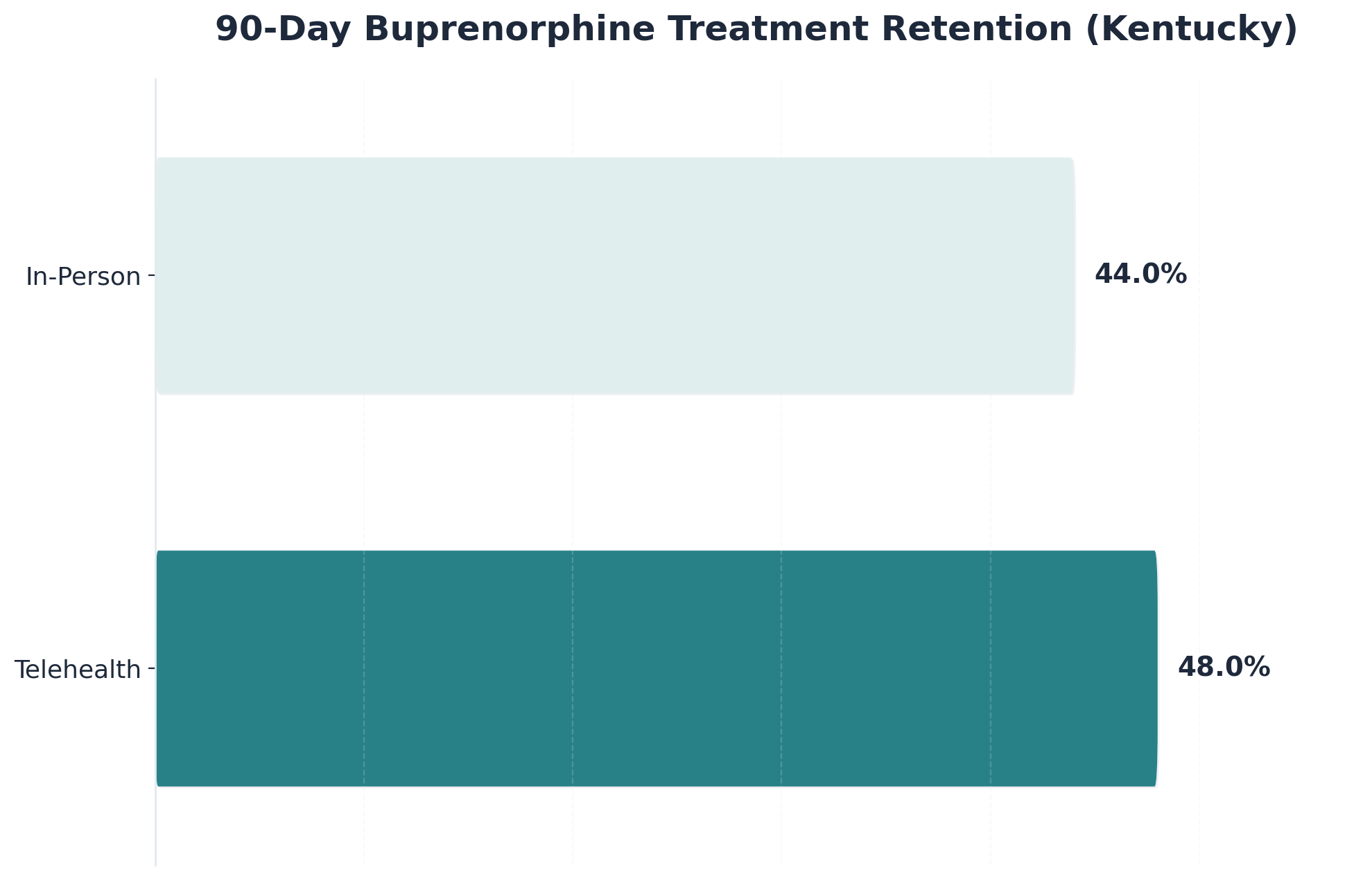
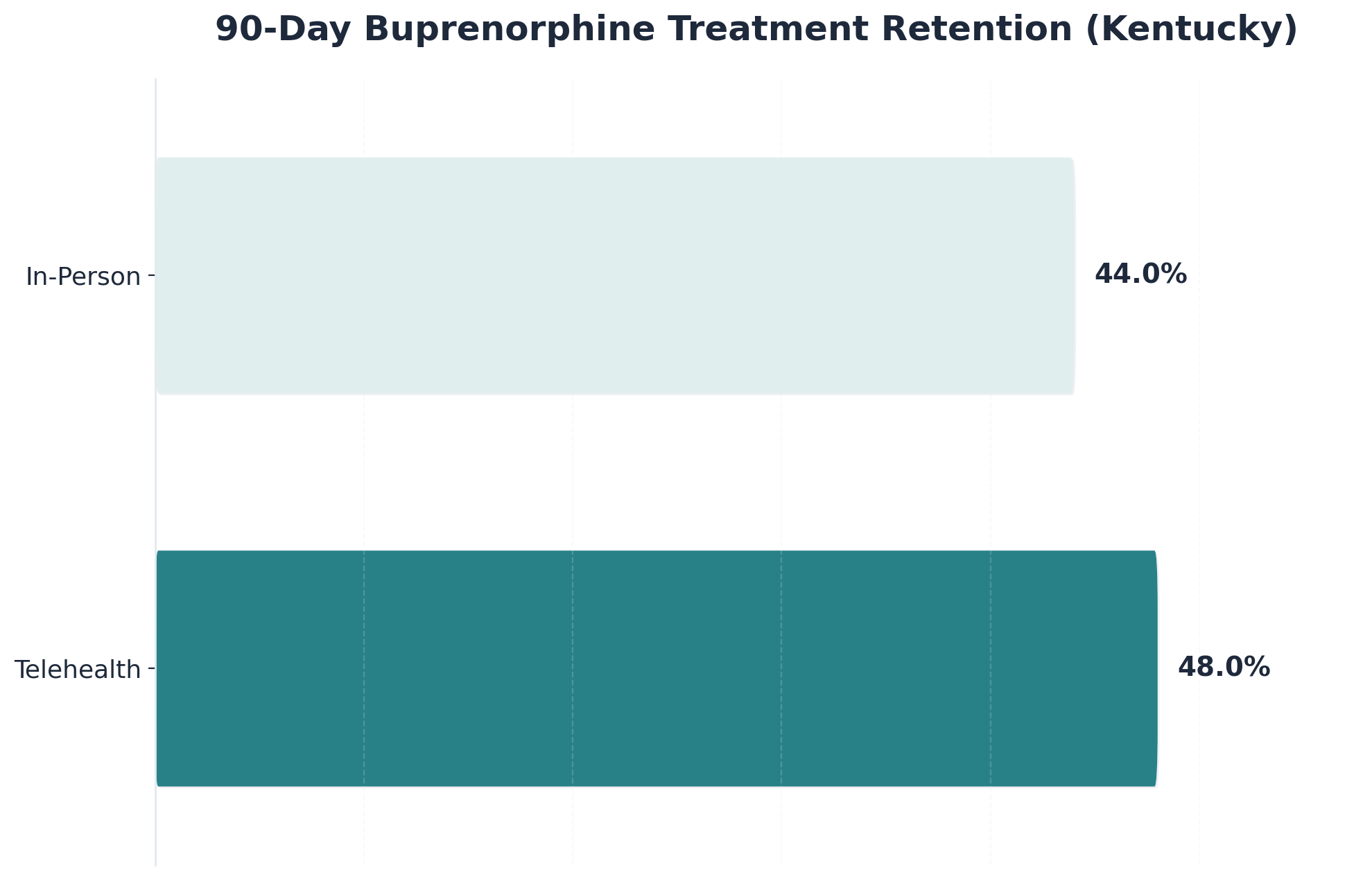
When it comes to treatment retention, studies show that online rehab programs consistently match or even surpass the rates seen in face-to-face settings. Medicaid data from Kentucky and Ohio echoed these findings: 48% of individuals starting buprenorphine via telehealth stayed in treatment for 90 days, compared to 44% for in-person starts in Kentucky.2
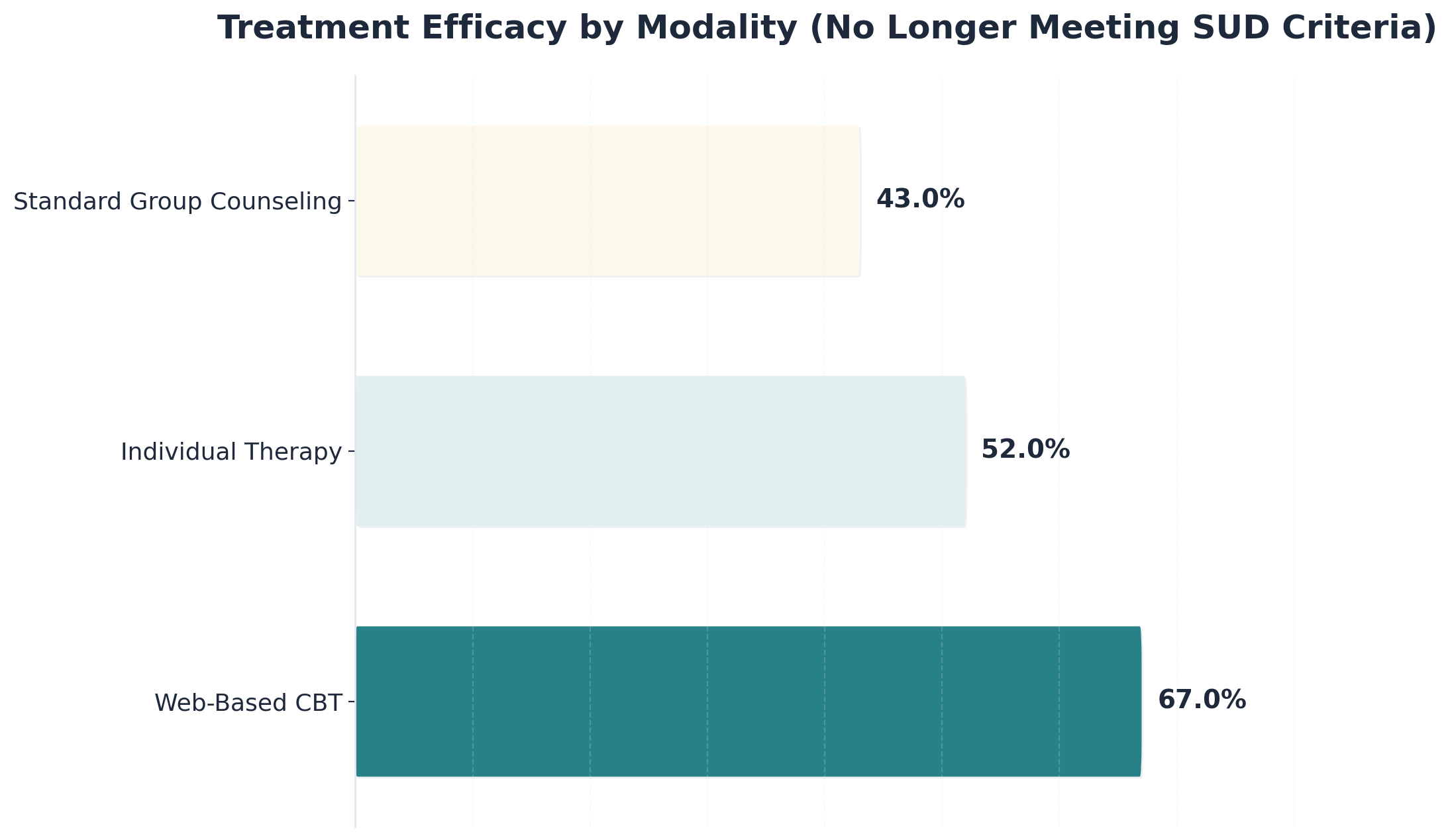
Recent studies confirm that virtual recovery programs deliver strong abstinence outcomes. In a large telehealth intensive outpatient program, 91% of participants who stayed engaged for at least 30 days achieved 30 consecutive days of abstinence.4 Another compelling example comes from a Yale study: 67% of individuals using a web-based CBT program no longer met criteria for substance use disorder at the end of treatment, compared to 43% in standard group counseling.6
Multiple large-scale studies show that telehealth addiction services are not just convenient—they deliver results equal to or better than traditional models. For example, one major review found that virtual care achieves abstinence rates and substance use reductions comparable to in-person treatment.3
| Metric | Virtual Outcome | In-Person Outcome | Key Insight |
|---|---|---|---|
| Retention (30 Days) | 80% Engagement | 50-68% Engagement | Virtual care often retains patients longer due to reduced barriers.4 |
| Opioid Overdose Reduction | 36% Reduction | Baseline | Starting buprenorphine online significantly reduces overdose risk.5 |
| Dropout Rates (CBT) | 25% Dropout | 50% Dropout | Web-based CBT keeps neurodivergent and general populations engaged.6 |
When it comes to treatment retention, studies show that online rehab programs consistently match or even surpass the rates seen in face-to-face settings. Medicaid data from Kentucky and Ohio echoed these findings: 48% of individuals starting buprenorphine via telehealth stayed in treatment for 90 days, compared to 44% for in-person starts in Kentucky.2
Recent studies confirm that virtual recovery programs deliver strong abstinence outcomes. In a large telehealth intensive outpatient program, 91% of participants who stayed engaged for at least 30 days achieved 30 consecutive days of abstinence.4 Another compelling example comes from a Yale study: 67% of individuals using a web-based CBT program no longer met criteria for substance use disorder at the end of treatment, compared to 43% in standard group counseling.6
Having established a solid understanding of how online addiction recovery services work, you can now apply that knowledge to evaluate specific programs. Not all telehealth platforms offer the same level of care. Start by examining the clinical credentials of the treatment team. Quality digital platforms employ licensed clinicians with specialized training in addiction treatment.
Ask programs directly:
Evaluate the level of care provided and flexibility of scheduling. Effective virtual treatment programs offer various intensity levels, from intensive outpatient sessions meeting multiple times weekly to ongoing maintenance support. Finally, examine support structures beyond individual therapy sessions. Group counseling opportunities, peer support networks, family involvement options, and crisis intervention protocols indicate comprehensive care.
Virtual recovery programs thrive when they combine proven techniques that translate well to digital care. Medication-assisted treatment (MAT), for instance, has shown impressive results. Virtual therapy, including web-based cognitive behavioral therapy (CBT), can outperform traditional counseling.
MAT—especially with medications like buprenorphine—has proven highly effective in telehealth addiction services. Recent research found that starting buprenorphine treatment virtually led to a 36% reduction in opioid overdose rates compared to starting in person.5 These outcomes show that virtual recovery programs not only match but sometimes exceed traditional success benchmarks.
Virtual therapy—including video-based individual counseling and web-based CBT—has shown strong outcomes. Patient satisfaction with virtual therapy remains high, and many clinicians now view online counseling as equally effective to in-person care after gaining virtual experience.7
At-home detox within telehealth addiction services involves a careful balance of accessibility and medical monitoring. Virtual recovery programs start with thorough assessments to determine if at-home detox is safe, often reserving this approach for those with mild to moderate withdrawal risk.
Practice This: Create a checklist of questions to ask a provider about their at-home detox protocols:
1. How do you handle medical emergencies? 2. What technology is required for monitoring? 3. How frequently do medical check-ins occur?
High-quality virtual recovery programs share a few essential features. First, they employ licensed clinicians with specialized training in substance use disorder and co-occurring mental health care. Reputable telehealth addiction services also maintain strict privacy protections, including HIPAA-compliant technology.
Every reputable virtual recovery program should only employ licensed clinicians who are authorized to provide substance use disorder and co-occurring mental health care in your state. State-by-state licensing ensures that providers meet local regulations and are accountable for upholding professional standards.
Every reputable virtual recovery program should use HIPAA-compliant video platforms, encrypted messaging, and strict confidentiality policies. These privacy measures help participants feel comfortable sharing honestly. Research shows that robust privacy practices are closely linked to higher satisfaction and engagement in virtual recovery programs.7
Understanding which programs work—and for whom—naturally leads to examining how virtual recovery platforms adapt to serve populations with distinct treatment needs. When standard approaches don't adequately address particular challenges, specialized programs emerge to fill critical gaps.
Pregnant and Postpartum Individuals: Virtual platforms eliminate logistical obstacles like childcare and transportation while providing consistent engagement. Research shows this increases treatment retention by 40-60% compared to traditional models for this population.
Rural Populations: A resident of rural Montana or Vermont seeking specialized dual-diagnosis treatment might find no qualified providers within a three-hour drive. Virtual platforms bridge these gaps by connecting individuals with clinicians who possess expertise unavailable locally.
Veterans and First Responders: Virtual programs designed for these populations employ providers with specialized training in military culture and post-traumatic stress. The privacy of home-based treatment proves particularly valuable for active-duty service members who fear career consequences from seeking help through official channels.
Virtual recovery programs are especially well-suited for working professionals who need discretion, individuals with neurodivergence or trauma histories, and people in rural or underserved communities. Research shows that telehealth addiction services remove barriers like travel time and scheduling conflicts.
Many working professionals hesitate to seek substance use disorder support due to concerns about workplace stigma. Virtual recovery programs solve these concerns by allowing confidential access to care from a private space. This flexibility lets individuals schedule appointments around work commitments, reducing missed sessions.
Many neurodivergent adults and trauma survivors find traditional rehab settings overwhelming due to sensory overload or triggering social dynamics. Virtual recovery programs address these challenges by allowing participants to engage from the safety of their own space. Research shows that web-based CBT reduces dropout rates from 50% in traditional modalities to just 25% in web-based programs.6
For individuals living in rural Vermont, New Hampshire, Massachusetts, or Connecticut, traditional in-person substance use disorder treatment can be hard to reach. Virtual recovery programs bring care directly to them. Research shows that engagement and retention rates in telehealth addiction services often exceed those of in-person care.2
While virtual recovery programs offer proven benefits, challenges like lack of reliable internet or private spaces persist. Research shows that 31% of individuals using telehealth for substance use disorder treatment report barriers related to technology access or privacy.8
Tech Issues: Use phone-based counseling backups or asynchronous modules.
Privacy Issues: Utilize noise-canceling headphones, white noise machines, or chat-based functions during sessions.
Engagement: Consider hybrid models that blend virtual and occasional in-person contact.
The digital divide remains one of the biggest barriers to virtual recovery programs. To help bridge this gap, some programs now offer tech support hotlines, lend tablets, and create simple guides to boost digital literacy. Flexible options like phone-based counseling can provide access even if video calls aren't possible.
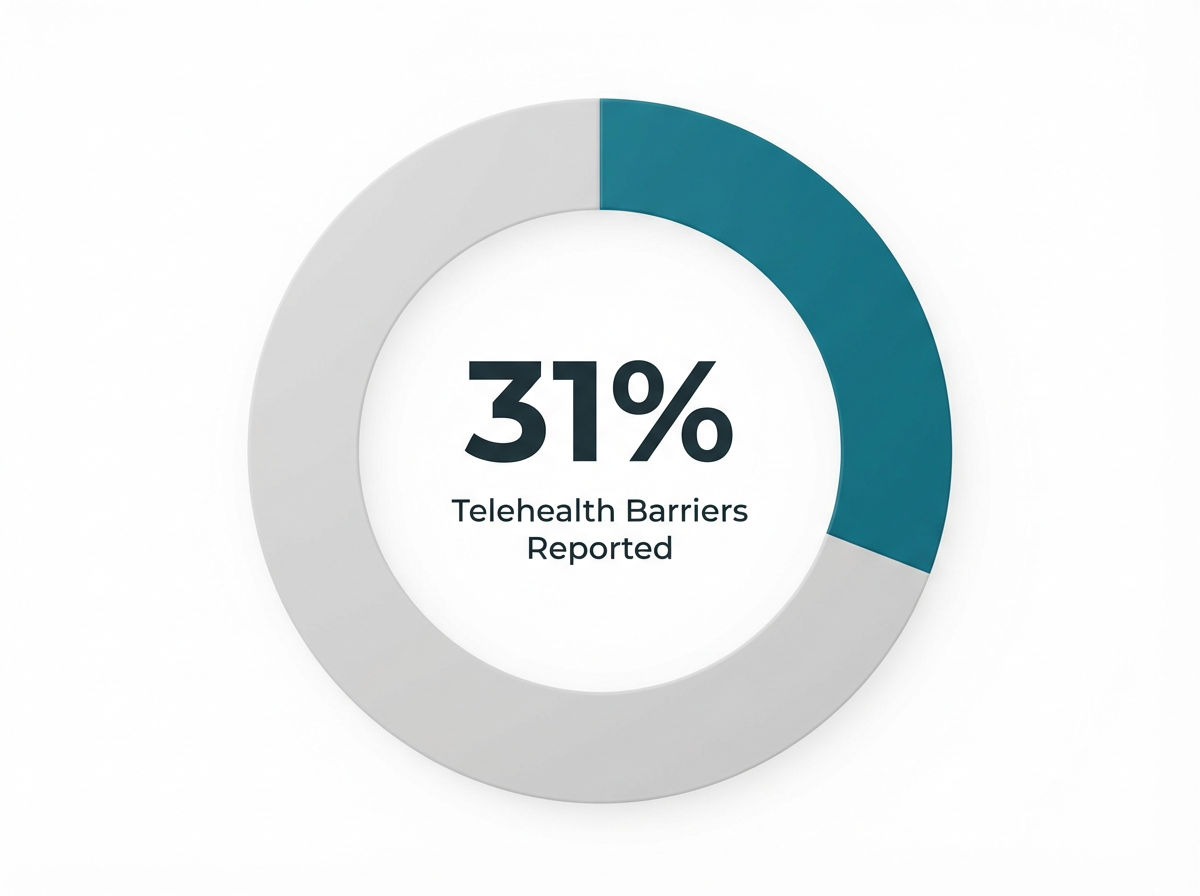
About 31% of people using virtual recovery programs report privacy challenges. To address this, participants use noise-canceling headphones or join sessions from their car. Programs are also encouraging flexible scheduling and offering phone-based or asynchronous options for those unable to secure a private space.
Hybrid models blend the best of telehealth addiction services with the unique strengths of in-person care. Recent research shows that individuals who take part in both virtual and in-person group therapy have significantly higher treatment completion rates than those in virtual-only programs.10
Taking the first step toward recovery can feel overwhelming, but online treatment programs have made accessing support more straightforward than ever. The journey begins with a simple phone call or online inquiry, where intake coordinators help determine the appropriate level of care based on individual circumstances and needs.
Most virtual treatment programs start with a comprehensive assessment conducted through a secure video platform. This evaluation examines addiction history, current challenges, and any concurrent psychological concerns that may require integrated treatment. The assessment process typically takes 60 to 90 minutes and helps create a personalized treatment plan that addresses specific recovery goals.
After the initial assessment, individuals can often begin participating in group therapy sessions, individual counseling, and educational workshops within days rather than weeks. This streamlined access to care represents a significant advantage over traditional programs that may have lengthy waitlists. Digital platforms allow treatment teams to schedule sessions around work commitments, family responsibilities, and other life obligations that might otherwise create barriers to recovery.
Technology requirements for virtual recovery programs are minimal. Most people can participate using a smartphone, tablet, or computer with internet access and a private space for confidential sessions. Treatment providers typically offer technical support to help navigate any platform challenges, ensuring technology never becomes an obstacle to receiving care.
The transition into online treatment also includes connecting with peer support networks and recovery communities online. Many programs facilitate introductions to others at similar stages in their healing journey, creating accountability partnerships and lasting connections. These relationships often extend beyond formal treatment sessions, providing ongoing encouragement during challenging moments.
Virtual treatment has fundamentally transformed how people access addiction recovery services, removing traditional barriers of distance, scheduling conflicts, and limited local resources. While online programs may not suit everyone's needs, they provide a legitimate and effective pathway to recovery for those who can benefit from their flexibility. For individuals seeking help, these digital platforms represent an opportunity to begin healing immediately, with professional support and evidence-based care delivered wherever they feel most comfortable engaging in the recovery process.
If you're considering virtual recovery support, you're likely weighing practical concerns alongside deeper questions about whether remote care can truly meet your needs.
Yes, you can receive medication-assisted treatment (MAT), including medications like Suboxone (buprenorphine/naloxone), through virtual recovery programs. Telehealth addiction services allow licensed clinicians to prescribe and manage MAT remotely, provided you reside in a state where the provider is authorized to operate—such as Vermont, Massachusetts, Connecticut, or New Hampshire. Research shows that starting buprenorphine treatment online not only increases treatment retention but also results in a 36% reduction in opioid overdose rates compared to in-person initiation.5
If you don’t have reliable internet or a private space for virtual recovery sessions, you’re not alone—about 31% of people using telehealth addiction services report these very challenges.8 The good news is, many virtual recovery programs are designed with workarounds. Options like phone-based counseling, asynchronous modules, or flexible scheduling can help you participate without needing strong Wi-Fi or a quiet home office.
Your participation in virtual recovery programs is protected by strict privacy laws and confidentiality policies. High-quality virtual recovery programs use HIPAA-compliant technology and encrypted platforms, so your employer or family will not be notified or have access to your treatment information unless you choose to share it.7
Virtual recovery programs approach at-home detox with careful screening and robust safety protocols. Before beginning, participants are thoroughly assessed to ensure they are suitable candidates. During detox, medical oversight is provided through frequent video check-ins, secure symptom tracking, and 24/7 access to clinical support. If a participant shows signs of serious complications, they'll be directed to seek in-person or emergency care immediately.1
Most online rehab and virtual recovery programs are now covered by major insurance plans, including Medicaid in Vermont, Massachusetts, Connecticut, and New Hampshire. This insurance parity means telehealth addiction services are reimbursed at rates similar to in-person care.3 Providers typically take your insurance information upfront, verify your benefits, and explain any out-of-pocket costs before you start.
Relapsing after traditional rehab can feel discouraging, but switching to online treatment may offer a different experience. Virtual recovery programs are designed for flexibility, privacy, and ongoing engagement. Research shows that telehealth addiction services often lead to higher retention rates compared to conventional care, with 80% of participants staying engaged for at least 30 days versus 50-68% in typical in-person programs.4
Yes, online rehab can be customized to accommodate ADHD or autism. Virtual recovery programs are often more comfortable for neurodivergent adults because you can access support from your own familiar environment and control sensory input. Research shows that web-based cognitive behavioral therapy (CBT) significantly reduces dropout rates for neurodivergent participants—only 25% dropped out of online programs, compared to 50% in traditional settings.6
To verify that an online rehab program has legitimate credentials, check if the organization openly lists its clinicians’ names, credentials, and licensing details on its website. Look for clear confirmation that providers are licensed to practice in your state. You can also confirm clinician licenses by searching your state’s official licensing board database.7
Virtual individual therapy often leads to higher clinical improvement and lower dropout rates due to personalized attention. Virtual group therapy excels at building peer support and accountability. Programs that blend virtual and in-person group sessions (a hybrid approach) see the highest treatment completion rates.610
Yes, you can continue working full-time while participating in online intensive outpatient treatment (IOP). Virtual recovery programs are designed for flexibility—sessions are often scheduled during evenings or outside standard work hours. Research shows that telehealth addiction services are especially effective for working professionals who need discreet, accessible care.7
Yes, many virtual recovery programs include family therapy sessions and dedicated support for loved ones via secure video calls. Research shows that involving loved ones in treatment can enhance engagement and outcomes.7
The current DEA telemedicine flexibilities for prescribing controlled substances are set to last through December 31, 2026. This extension ensures continuity for individuals receiving medication-assisted treatment while permanent telemedicine regulations are developed.9
Yes—trauma-focused therapies like EMDR are increasingly available through virtual recovery programs via secure video platforms. Research shows that virtual recovery programs can be tailored to accommodate the unique needs of trauma survivors, including flexible scheduling and camera-off options.7
Individuals with severe alcohol or benzodiazepine dependence who are at high risk for dangerous withdrawal symptoms often require in-person medical supervision. Similarly, people experiencing acute psychiatric crises or those without reliable access to technology may find that online rehab is not the best fit.18
You can often start treatment with a virtual recovery program within 24–72 hours of reaching out. Most telehealth addiction services offer streamlined intake processes, allowing you to complete assessments and schedule your first session online without the long wait times often associated with in-person rehab.3

November 6, 2025

January 6, 2026

November 6, 2025