
Therapist Near Me That Accept Medicaid: Virtual Care That Breaks Barriers and Builds Futures
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
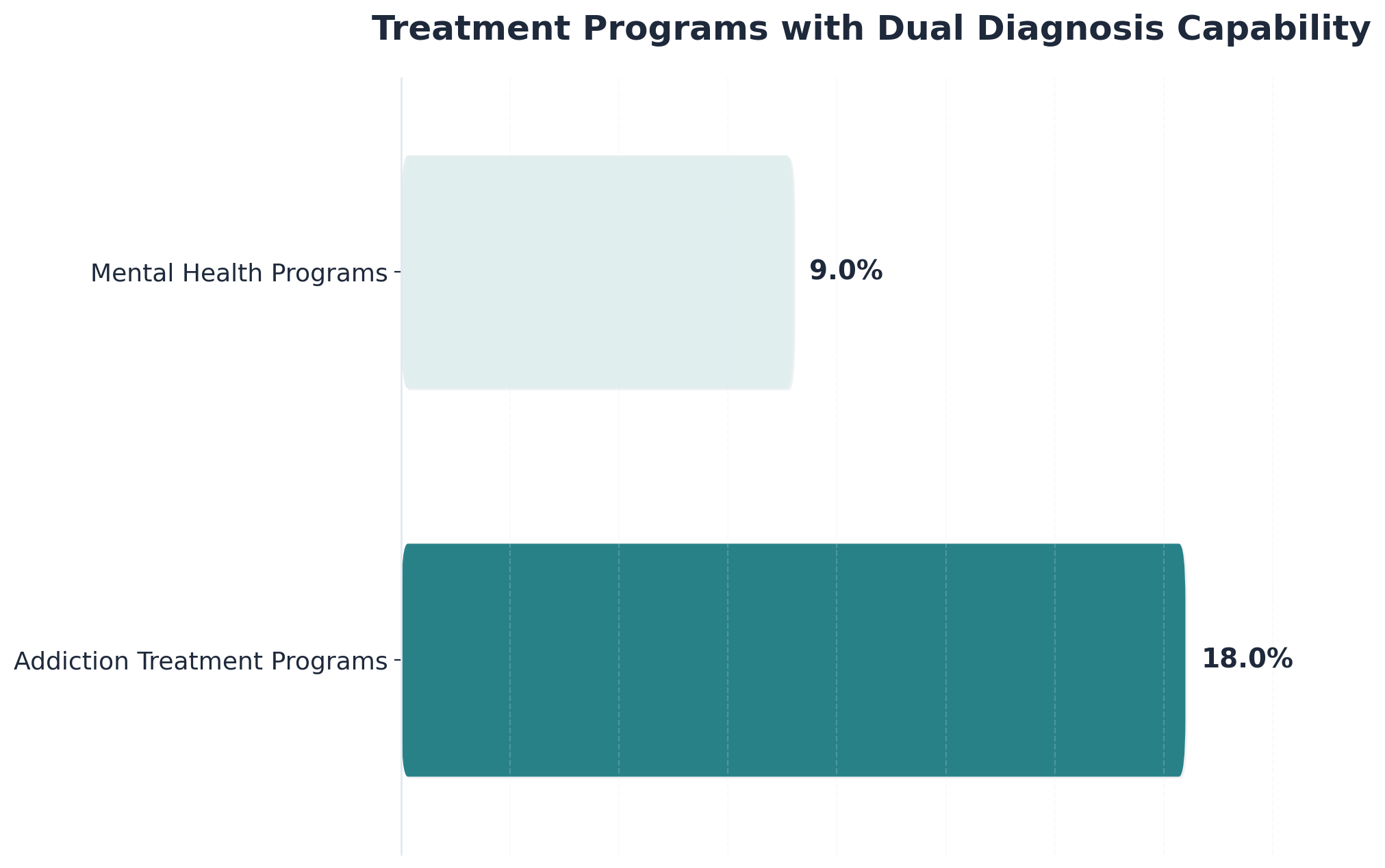
The relationship between mental health conditions and addiction disorders operates as a complex, bidirectional pathway. Research consistently shows that individuals with psychological challenges face significantly higher risks of developing dependency issues, while those struggling with addiction often experience co-existing psychiatric symptoms. This interconnection, known as dual diagnosis or concurrent disorders, affects nearly half of all people seeking treatment for addiction disorders.
Psychiatric conditions can drive addictive behaviors as individuals attempt to self-medicate uncomfortable symptoms. Someone experiencing anxiety might turn to alcohol for temporary relief, while a person with depression may use stimulants to counteract persistent fatigue and low mood. This pattern creates a deceptive cycle where substances provide short-term relief but ultimately worsen the underlying psychological condition.
The reverse pathway proves equally powerful. Chronic dependency fundamentally alters brain chemistry, potentially triggering or exacerbating psychiatric conditions. Prolonged alcohol use can intensify depression, while stimulant abuse may precipitate anxiety disorders or paranoia. These substance-induced changes can persist long after someone stops using, complicating the recovery process.
Neuroscience reveals why these conditions so frequently coexist. Both psychiatric disorders and addiction involve similar brain regions responsible for reward processing, impulse control, and emotional regulation. Genetic factors, traumatic experiences, and environmental stressors can simultaneously increase vulnerability to both conditions, creating overlapping risk profiles.
This intricate connection explains why treating only one condition while ignoring the other rarely produces lasting recovery. When psychological symptoms remain unaddressed during addiction treatment, they continue driving addictive behaviors. Similarly, focusing solely on psychiatric care without addressing dependency patterns leaves individuals vulnerable to relapse. Effective recovery requires comprehensive treatment that simultaneously addresses both conditions, recognizing them as intertwined aspects of a person's overall health rather than separate, isolated problems.
To understand why mental health and substance use disorders often appear together, it helps to look at the underlying science. Research points to a mix of genetic, biological, and environmental influences that can make someone more vulnerable to both conditions.
Studies reveal that nearly half of individuals with substance use disorder also meet criteria for post-traumatic stress disorder, showing a clear overlap in risk factors.7
The concept of co-occurring disorders—sometimes called dual diagnosis—recognizes that psychological distress, trauma exposure, and neurobiological changes interact in ways that amplify both addiction and emotional challenges. This approach is ideal for people seeking a deeper understanding of how mood regulation, brain function, and life experiences connect in recovery. Next, let’s break down how brain chemistry and external factors shape these overlapping conditions.
Brain chemistry plays a central role in linking mental health challenges with substance use patterns. When someone experiences chronic stress, trauma, or emotional pain, the brain’s reward system—including neurotransmitters like dopamine and serotonin—can become imbalanced. This chemical imbalance often drives individuals to seek relief or pleasure through substances, which temporarily boost these brain chemicals.
Over time, repeated substance use alters brain pathways, making it harder to experience motivation or joy naturally—a cycle that deepens both emotional distress and addictive behavior.4 This path makes sense for individuals who notice mood swings or difficulty coping with stress, as brain-based changes in motivation and resilience are a key part of recovery. Understanding these neurobiological links helps clarify why emotional struggles and substance use so frequently occur together, setting the stage to explore how our environment and genetics also affect risk.
A simple self-checklist can help clarify risk: Do you have blood relatives with addiction or depression? Have you experienced ongoing stress, trauma, or unstable living conditions? Research shows that genetics account for 40-60% of a person's risk for substance use and related behavioral health challenges, while environmental factors like early-life adversity or chronic stress can activate this genetic vulnerability.3
Experts note that individuals with both a genetic predisposition and exposure to environmental hardship are far more likely to develop co-occurring conditions. This solution fits those who recognize family history or ongoing stress in their lives, as understanding these dual influences can guide more effective prevention and recovery planning. These combined risks set the stage for identifying your personal treatment needs in the next section.
Before choosing a recovery path, it helps to use a self-assessment tool to clarify your treatment needs. Start by asking: Are you struggling with both mood-related symptoms—like anxiety, irritability, or persistent sadness—and substance use? Have you noticed patterns where one issue seems to trigger or worsen the other?
Research shows only 14.5% of people with both substance use and behavioral health conditions receive treatment for both at the same time, highlighting a major care gap.1 This approach works best when you’re unsure whether your symptoms are connected or if you need integrated support for emotional well-being and substance use. Identifying these patterns early can guide you toward evidence-based, whole-person care. In the next sections, we’ll break down diagnostic questions and explore how trauma might shape your recovery needs.
A quick diagnostic checklist can help clarify if you’re dealing with co-occurring mental health and substance use conditions. Ask yourself the following questions:
Industry guidelines recommend looking for patterns where behavioral health symptoms and substance use reinforce each other, as this is common with dual diagnosis.8 This method works when you’re unsure whether you need support for both emotional well-being and addiction, as it helps identify personal patterns that might require integrated care. If several of these questions resonate, it’s a sign to seek a professional assessment for both conditions.
A trauma self-check can help clarify if past experiences are shaping your substance use patterns. Ask yourself: Have you lived through distressing events that continue to affect your daily life? Do you find yourself using substances to numb memories or emotional pain?
Studies reveal that nearly half of individuals with substance use disorder also meet criteria for post-traumatic stress disorder, pointing to a strong link between trauma exposure and addiction risk.7 This solution fits people who notice their substance use increases after reminders of past trauma or when coping with anxiety and stress. Recognizing the impact of trauma is key, as trauma-informed care has been shown to improve outcomes for those managing both behavioral health issues and addiction. Identifying these patterns now can guide you toward care that addresses both emotional distress and substance use together.
The complexity of dual diagnosis established above leads to an important question: how do you actually choose the right path forward? Rather than a vague "it depends," effective decision-making follows specific criteria that clarify which approach fits your situation.
| Decision Factor | Assessment Criteria | Recommended Action |
|---|---|---|
| Severity Assessment | Active suicidal ideation, severe psychosis, or life-threatening withdrawal (tremors, seizures). | Emergency Intervention: Call 911 or visit an ER immediately. |
| Symptom Pattern | Psychiatric symptoms persist regardless of consumption patterns (e.g., depressed whether drinking or not). | Integrated Care: Requires coordinated dual-diagnosis care from day one. |
| Resource Constraints | Rural location, limited local options, or tight work schedule. | Virtual/Telehealth: Seek specialized virtual providers for therapy and medication management. |
| Support System | Stable housing, supportive family, workplace flexibility. | Intensive Outpatient (IOP): 3-4 sessions weekly combined with medication management. |
Decision Point 1: Severity Assessment
Begin by evaluating immediate risk and symptom intensity. If symptoms are moderate (persistent depression interfering with daily function, daily drinking to manage anxiety), you can proceed through standard care channels, but dual-diagnosis specialization remains essential. Mild symptoms (occasional low mood, weekend drinking that concerns you) allow more flexibility in provider selection, though integrated assessment still provides the clearest picture.
Decision Point 2: Symptom Pattern Analysis
Track how your psychiatric symptoms and substance use interact over two weeks. If depression or anxiety clearly worsen during active use and improve during abstinence, addiction treatment with psychiatric consultation may be primary. Example: "My panic attacks disappear after three days without alcohol."
Decision Point 3: Resource and Timeline Considerations
Evaluate practical constraints honestly. Check whether your insurance covers dual-diagnosis programs specifically, as standard mental health or addiction-only benefits may not. If you need treatment within days, hospital-based programs offer immediate access; if you can wait 2-4 weeks, outpatient dual-diagnosis clinics provide more scheduling flexibility.
Decision Point 4: Support System Evaluation
Assess your current stability and resources. If your support system is limited or housing is unstable, residential dual-diagnosis programs provide structure while you build recovery foundations. Personal readiness matters too—if you feel prepared to engage actively in therapy and make lifestyle changes, you're positioned for outpatient success.
A simple comparison checklist can help clarify which treatment model may fit your needs: Do you want both behavioral health and substance use challenges addressed in the same setting, or are you considering tackling them one after the other? Integrated treatment—delivering support for emotional well-being and addiction at the same time—consistently leads to better outcomes in symptom relief, stability, and daily functioning compared to sequential approaches.2
Consider this route if you’ve found that separating care leaves gaps or makes it harder to stay on track. Sequential models may appeal to those with strong preferences or barriers to accessing dual diagnosis care, but research strongly favors integration for long-term recovery. Next, we’ll explore why these differences matter and look at settings where each approach is used.
An outcome comparison checklist helps illustrate why integrated care stands out: Are you looking for improvements not just in substance use, but also in daily functioning, emotional stability, and long-term wellness? Studies demonstrate that when behavioral health and addiction are addressed together, people experience better results across substance use reduction, psychiatric symptom relief, housing stability, and overall functioning compared to treating each condition separately.2
This solution fits individuals who notice their mental well-being and recovery progress are deeply connected—integrated care is more likely to close gaps that sequential models leave open. Experts point out that integrated programs also reduce hospitalization and arrest rates, supporting a more stable return to work or community life. For those aiming to improve both emotional health and recovery outcomes, industry leaders find that a unified approach is the clear choice for sustained success.2
A quick comparison tool can help people decide between virtual and traditional (in-person) treatment settings for substance use and behavioral health support. Virtual care—delivered via telehealth—offers flexibility, privacy, and the ability to access therapy and group sessions from home. This approach is ideal when transportation, scheduling, or stigma makes in-person visits difficult.
Studies reveal that telehealth expansion has significantly increased access to integrated care, especially in rural areas and for those with demanding schedules.9 Traditional settings, such as clinics or rehab centers, suit individuals who prefer face-to-face interaction or need more intensive supervision. This method works when hands-on support or daily monitoring is crucial for safety. Both settings can deliver evidence-based therapy for emotional well-being and substance use, but virtual options are rapidly growing in effectiveness and acceptance.
A practical MAT (medication-assisted treatment) decision checklist can clarify if this approach fits your recovery needs: Are you managing opioid or alcohol use disorder and seeking to reduce cravings or withdrawal symptoms while building emotional resilience? MAT combines FDA-approved medications with behavioral therapies to stabilize brain chemistry and support functional recovery.
Research shows that when medication is paired with counseling, people experience improved outcomes in reducing substance use, managing psychiatric symptoms, and maintaining daily life stability.2 This approach works best when cravings or withdrawal make it difficult to engage in therapy alone, or when co-occurring behavioral health symptoms complicate recovery. If you’re navigating both substance use and mood challenges, MAT may offer a bridge to more consistent progress. Up next, we’ll compare specific medication options for different substances and discuss how therapy can be integrated for whole-person support.
A quick comparison chart can clarify which medication-assisted treatment (MAT) options are available for different substance use disorders.
methadone, buprenorphine, and naltrexone. Methadone is typically delivered in specialized clinics and suits those needing daily, structured support. Buprenorphine may be prescribed in office-based settings and works well for people seeking flexibility. Naltrexone is best for individuals who have already detoxed.acamprosate, disulfiram, and naltrexone can help reduce cravings or discourage drinking.This approach fits those who want medical support tailored to specific substance challenges, especially when symptoms of anxiety or depression complicate recovery. Studies reveal that combining MAT with behavioral interventions leads to higher rates of sustained recovery and improved emotional wellness compared to therapy alone.2
A practical integration checklist can help clarify how therapy and medication-assisted treatment (MAT) work together for lasting recovery: Are you receiving regular counseling sessions alongside prescribed medications? Are your providers coordinating to address both your substance use and underlying emotional challenges, such as anxiety or mood swings?
Research demonstrates that combining pharmacological support with behavioral therapies—like cognitive-behavioral therapy or motivational interviewing—produces better outcomes in symptom management, relapse prevention, and daily functioning than either approach alone.2 This method works when emotional resilience is just as important as reducing cravings, and when you want support for both behavioral well-being and substance use patterns. For many, this coordination helps address root causes and coping skills, creating a more stable foundation for recovery.
Recovery looks different for everyone, and the path forward depends heavily on individual circumstances, support systems, and the severity of dependency. Understanding which implementation pathway aligns with your current situation helps set realistic expectations and increases the likelihood of sustained success.

For individuals experiencing severe withdrawal symptoms or using substances like alcohol or benzodiazepines, medical detoxification provides the safest starting point. Research indicates that medically supervised detox reduces complication rates by 60-80% compared to unsupervised withdrawal. This controlled environment manages physical withdrawal while stabilizing health markers before transitioning to ongoing care. Following detox, residential programs offer 24/7 support and remove environmental triggers during the critical early recovery phase, with studies showing completion rates of 65-75% when medical detox precedes residential placement.
Those with stable housing, supportive relationships, and moderate dependency patterns often find success with intensive outpatient programs (IOPs). Clinical data demonstrates that IOPs achieve 50-60% abstinence rates at 12-month follow-up for individuals without severe dependency or co-occurring disorders. These structured interventions typically involve 9-15 hours of programming per week while allowing individuals to maintain work, family, and educational commitments. This pathway works particularly well when combined with regular peer support meetings and accountability check-ins, with telehealth delivery options expanding access for those with transportation or scheduling constraints.
For people already established in recovery who need additional support for concurrent psychological challenges, integrated dual diagnosis treatment addresses both dependency and emotional wellness simultaneously. Research shows that integrated care models improve outcomes by 30-40% compared to sequential treatment approaches, preventing the common pitfall of treating one issue while neglecting the other. This coordinated intervention recognizes that anxiety, depression, trauma, and addiction often interconnect, with many programs now offering hybrid in-person and telehealth formats to maximize accessibility.
Choosing the right pathway requires honest assessment of several key factors: severity of physical dependency (does withdrawal require medical supervision?), environmental stability (are triggers manageable at home?), support system strength (do you have accountability partners?), and co-occurring conditions (are mental health symptoms present?). Telehealth delivery has expanded across all pathways, offering individual therapy, group sessions, and medication management through secure video connections—particularly valuable for rural residents, those with mobility limitations, or individuals balancing intensive work schedules.
A practical resource planning checklist can help individuals weigh the real-life demands of recovery: How many hours per week can you dedicate to therapy or group sessions? What forms of social, family, or peer support are available? Are you able to access care through insurance or need to explore sliding-scale or state-funded options?
Studies reveal that only 14.5% of people with co-occurring behavioral health and substance use conditions receive treatment for both, often due to logistical or financial barriers.1 This solution fits those looking to balance treatment with work, family, or rural living; virtual and outpatient models now allow people to pursue emotional well-being and substance use recovery while maintaining daily routines. Up next, we’ll look at specific ways working professionals and at-home detox seekers can tailor their care plans.
A practical scheduling tool can help working professionals evaluate recovery options: Can you set aside time for weekly evening or early-morning telehealth sessions? Do you need a flexible approach that fits around meetings, travel, or family duties? Outpatient and virtual models now allow individuals to participate in therapy or support groups from home or the office, making it easier to maintain both emotional well-being and work responsibilities.9
This approach is ideal for people who want to protect their career while addressing behavioral health and substance use challenges, as research shows the outpatient segment is growing rapidly due to demand for care that accommodates job commitments. Industry leaders find that programs offering after-hours group therapy and digital support communities are especially helpful for those balancing a busy schedule. For many, these adaptable solutions remove barriers to treatment and reduce stigma, making recovery accessible without pausing professional life.
A home detox checklist brings clarity to the most important priorities: daily medical check-ins (virtual or phone), clear emergency protocols, and access to a supportive network. If you’re considering at-home detox, be honest about your health history, possible withdrawal risks, and whether you have a safe, sober environment.
Clinical guidelines recommend medical oversight for any detox—especially when withdrawal from substances like alcohol or opioids, which can cause dangerous symptoms, is possible.8 This method works when professional inpatient detox isn’t accessible, but only if regular nurse or physician contact is arranged and family or friends are ready to help monitor for complications. For many, virtual care models now mean medically supervised withdrawal and emotional support can happen from home, making early recovery more accessible for those balancing privacy and daily life.
A practical approach-matching tool can help individuals identify therapies tailored to their unique backgrounds and needs: Are you seeking support for trauma history, or do you benefit from neurodivergent-adaptive strategies? Studies reveal that nearly half of people with substance use disorder also experience PTSD, making trauma-informed therapies like Eye Movement Desensitization and Reprocessing (EMDR) and Internal Family Systems (IFS) especially valuable.7
This solution fits those who notice that traditional talk therapy hasn’t addressed deeper emotional wounds or unique ways of thinking. For individuals with neurodevelopmental differences, research shows that adaptive treatment models improve engagement and outcomes by honoring sensory preferences and communication styles.2 This approach is ideal for people who have not found success with one-size-fits-all care, as specialized methods can empower more effective healing. Next, we’ll break down what these therapies look like in practice and how to select the right fit for your situation.
A practical trauma-focused therapy checklist can help individuals identify if advanced modalities like Eye Movement Desensitization and Reprocessing (EMDR) or Internal Family Systems (IFS) are useful for their recovery journey. Ask: Do you experience distressing memories, flashbacks, or intense emotional reactions linked to past events? Have standard talk therapies left you feeling stuck or unable to process deeper trauma?
Research shows that trauma-informed approaches—such as EMDR, which uses guided eye movements to help reprocess painful memories, and IFS, which explores internal 'parts' of the self—can be especially effective when trauma and substance use disorders overlap.7 This approach is ideal for those who recognize unresolved emotional wounds are fueling substance use or mood challenges, as trauma-focused therapies address root causes and foster emotional healing. For people navigating both behavioral challenges and substance use, these specialized methods offer a path toward lasting resilience by integrating emotional wellness and recovery skills.
A neurodivergent-adaptive treatment checklist can help people with ADHD, autism spectrum disorder, or other neurodevelopmental differences identify support that honors their unique needs. Ask: Does your treatment environment respect sensory preferences (like lighting, sound, or breaks)? Are communication styles flexible—allowing for written responses, visuals, or extra processing time?
Research shows that adaptive models—those adjusting therapy to fit sensory, cognitive, and communication needs—lead to better engagement and outcomes for neurodivergent individuals receiving behavioral health and substance use support.2 This path makes sense for anyone who has struggled with traditional approaches that don’t accommodate differences in attention, emotional regulation, or learning style. Prioritize programs that offer structured routines, predictable formats, and space for self-advocacy, as these factors foster empowerment and resilience.
With a recovery pathway selected, the next critical step involves translating that choice into concrete action. A structured 30-day plan transforms intention into momentum, providing the scaffolding needed during this vulnerable transition period. This initial month serves as a critical period where new habits take root, support systems solidify, and the integrated approach to both mental health and addiction recovery becomes part of daily life.

Common Week 1 Challenge: Overwhelming emotions or physical withdrawal symptoms may make routines feel impossible. Navigate this by breaking tasks into 15-minute increments and communicating openly with treatment providers about symptom management.
Common Week 2 Challenge: Feeling disconnected at meetings or uncertain about medication changes. Remember that finding the right community takes time, and psychiatric medications often require adjustment periods.
Common Week 3 Challenge: Techniques feel awkward or ineffective initially. Skills strengthen with repetition; commit to trying each technique at least three times before dismissing it.
Common Week 4 Challenge: Overconfidence leading to reduced meeting attendance or treatment engagement. Early progress is encouraging but doesn't indicate readiness to reduce support.
A simple week 1-2 checklist can guide your first steps: (1) schedule an initial assessment with a provider specializing in co-occurring disorders, (2) review your current symptoms and goals, and (3) build a support network with family or trusted peers. During this phase, individuals typically complete a clinical evaluation to identify emotional, behavioral, and substance use patterns.
Best practice involves setting clear recovery goals and establishing communication channels with your care team. Studies reveal that prompt engagement and assessment in the early weeks lead to better outcomes and greater consistency in sticking with a treatment plan.5 This approach is ideal if you want to build a strong foundation for both emotional wellness and substance use recovery. Up next, we’ll explore how to set clinical baselines and activate your social support systems for lasting progress.
A practical baseline-setting tool helps individuals and providers track starting points for both emotional and substance use challenges. During the first week, you’ll likely complete standardized assessments—these may include self-report surveys or interviews about mood, sleep, cravings, and daily habits. Establishing these clinical baselines gives a clear picture of where you are before treatment begins, making it easier to recognize improvements in areas like anxiety, coping skills, and resilience over time.
Industry leaders find that setting specific, measurable goals—such as reducing substance use days or managing stress triggers—supports accountability and motivation throughout recovery.2 This method works when you want to see tangible progress and make adjustments with your care team. By grounding your plan in data and personal objectives, you’re better equipped to build emotional wellness and sustain long-term change.
A practical family engagement checklist can help individuals activate a strong support system during early recovery: (1) identify key family members or trusted loved ones who can provide encouragement, (2) share your treatment goals and boundaries clearly, and (3) invite them to participate in education sessions or family meetings as recommended by your provider.
Studies reveal that ongoing family involvement—such as attending educational workshops or structured check-ins—can significantly improve both emotional health and substance use outcomes, especially when integrated into the first weeks of care.2 This method works when open communication and shared understanding are priorities, as families who learn about co-occurring conditions are more likely to offer constructive support without enabling. By weaving family education into the early stages of your plan, you help create a stable foundation for long-term well-being and resilience.
A week 3-4 skill-building checklist can guide your efforts: (1) practice healthy coping strategies for cravings and mood swings, (2) work with your care team to set realistic, long-term goals, and (3) create daily routines that support continued progress. During this phase, individuals focus on strengthening resilience and building habits that reinforce both behavioral health and addiction recovery.
Research shows that people who participate in ongoing support—such as peer coaching or structured check-ins—are more likely to maintain positive changes over time.5 This approach is ideal for those who want to prevent relapse and develop lasting wellness, as establishing consistent routines and accountability systems helps bridge the gap between early momentum and sustained growth. As you continue, the next steps will dig deeper into how peer coaching and accountability structures keep progress on track.
A peer coaching and accountability checklist can offer a powerful boost to both substance use recovery and behavioral wellness during weeks 3 and 4. Ask yourself: Do you have access to a peer coach or mentor who has lived experience with recovery? Are you participating in regular check-ins or support groups that encourage honest progress updates?
Research shows that ongoing peer engagement and accountability structures increase the likelihood of maintaining progress, especially when emotional health and substance use challenges are addressed together.5 This solution fits those who benefit from shared understanding, encouragement, and gentle reminders to stay on track. Peer coaches often provide practical feedback, celebrate milestones, and help brainstorm solutions to setbacks, fostering self-efficacy and resilience. For many, these relationships become a steady anchor, supporting long-term skill-building and relapse prevention as you move forward in your recovery plan.
A practical progress-tracking and relapse prevention checklist is essential during weeks 3 and 4 of recovery. Start by reviewing your weekly goals: Are you meeting personal milestones for emotional wellness and reduced substance use? Use tools like daily mood logs or craving journals to spot patterns and early warning signs.
Research shows that individuals who regularly track their behavioral health progress and participate in structured aftercare experience fewer relapses and more stable recovery outcomes.5 This approach suits those wanting to build self-awareness and catch setbacks early, as measurement-based care makes it easier to adjust strategies with your care team. By combining self-monitoring with ongoing support, individuals can strengthen resilience and lower the risk of returning to old habits.
Recovery from addiction is a deeply personal journey, and finding the right support can feel overwhelming. Whether you're considering help for the first time or exploring options that better align with your needs, taking that initial step requires courage and commitment. Understanding that recovery isn't a one-size-fits-all process opens the door to discovering approaches that truly resonate with your individual circumstances.
As explored throughout this article, addiction rarely exists in isolation from mental health challenges. The interconnected nature of substance use disorders and conditions like anxiety, depression, or trauma creates complexity that single-focus treatment often fails to address. Integrated care models acknowledge this reality by treating the whole person rather than separating psychological and addiction-related symptoms into disconnected treatment tracks. This comprehensive approach forms the foundation for sustainable recovery.
Choosing the right pathway requires honest self-reflection about your specific situation. Consider what obstacles have prevented you from seeking help in the past, what aspects of your life feel most impacted by addiction, and whether you're experiencing concurrent mental health challenges. These insights become valuable information when discussing care options with healthcare providers and help determine whether outpatient flexibility, intensive programming, or residential immersion best suits your needs.
If you're ready to take concrete steps today, start with these actions: First, contact your insurance provider to understand your mental health and substance use coverage, including any requirements for dual diagnosis treatment. Second, use the SAMHSA National Helpline (1-800-662-4357) or their online treatment locator to identify credentialed providers in your area who specialize in integrated care. Third, schedule an assessment with a dual diagnosis specialist who can evaluate both substance use and mental health concerns simultaneously, providing a comprehensive understanding of your treatment needs.
Remember that the complexity discussed in these pages—the bidirectional relationship between mental health and addiction, the need for personalized treatment intensity, the importance of addressing root causes—isn't a barrier to recovery. It's precisely why integrated treatment exists. Recovery is possible, and taking that first step toward comprehensive care demonstrates the strength and self-awareness necessary for lasting change.
Recovery from addiction raises many questions, especially when psychological concerns are part of the picture. Understanding how comprehensive dual diagnosis care works can help individuals and their loved ones make informed decisions about care.
Dual diagnosis care addresses both addiction and psychiatric challenges simultaneously. This comprehensive approach recognizes that these conditions often influence each other, and treating them together typically leads to better outcomes than addressing them separately. For example, someone with depression and alcohol dependence receives therapy that explores how drinking may temporarily mask depressive symptoms while ultimately worsening them, while also addressing the underlying depression through evidence-based psychiatric treatment.
If you've experienced persistent mood changes, anxiety, trauma symptoms, or other psychological challenges alongside substance use, dual diagnosis care may be appropriate. Warning signs include using substances to manage emotional distress, difficulty staying sober despite previous attempts, or finding that psychiatric symptoms worsen during periods of abstinence. A comprehensive assessment can identify whether co-occurring conditions are present and determine the most effective treatment approach for your specific situation.
It's common for underlying psychiatric symptoms to become more noticeable when substances are removed, as substances often mask or temporarily suppress these symptoms. Integrated dual diagnosis programs anticipate this and provide psychiatric support throughout the recovery process. For instance, someone who used alcohol to self-medicate anxiety may experience increased anxiety initially, but the treatment team adjusts therapeutic interventions and, when appropriate, psychiatric medications to provide stability while developing healthier coping strategies.
Yes, psychiatric medications are often an essential component of dual diagnosis treatment. When prescribed and monitored by qualified professionals who understand both addiction and psychiatric care, medications like antidepressants, mood stabilizers, or non-addictive anxiety medications support recovery without compromising sobriety. The key is working with providers who coordinate care between psychiatric and addiction treatment, ensuring medications address mental health needs while considering addiction vulnerabilities.
Treatment costs vary widely depending on the level of care, program length, and location. Many insurance plans cover addiction and mental health treatment under mental health parity laws, though coverage specifics differ by plan. Outpatient programs typically cost less than residential care, and some community-based programs offer sliding-scale fees. It's important to verify your specific coverage, understand deductibles and copays, and explore financial assistance options if needed.
Recovery timelines vary significantly based on individual circumstances, the substances involved, the presence of psychological challenges, and personal support systems. While initial programs may last 30 to 90 days, recovery is an ongoing process that continues well beyond formal care. Someone with co-occurring PTSD and opioid dependence may need several months of intensive treatment followed by years of continued therapy, while another person might transition to less intensive support more quickly.
Family involvement can significantly support recovery outcomes. Many programs offer family education and therapy sessions that help loved ones understand addiction and psychiatric challenges, develop healthy communication patterns, and create supportive home environments. For example, family sessions might address how to respond supportively when someone experiences psychiatric symptoms or cravings, rather than reacting with frustration or enabling behaviors.
Choosing between virtual and in-person treatment starts with your needs and preferences. If flexibility, privacy, and convenience are top priorities—or if transportation or time constraints are barriers—virtual care can be a strong fit. Telehealth has expanded access to behavioral support, especially for those in rural areas or with busy schedules. On the other hand, in-person settings may be better for individuals seeking face-to-face connection or who need more structured supervision.9
Family members can offer strong support in integrated treatment by encouraging healthy boundaries, open communication, and participation in recommended activities—without shielding their loved one from natural consequences. Experts advise families to educate themselves about co-occurring conditions and avoid covering up or rescuing behaviors, which can unintentionally reinforce substance use or emotional avoidance.2
Virtual treatment programs are proving to be as effective as traditional in-person rehab facilities for many individuals seeking substance use and behavioral health support. Research shows that telehealth options deliver comparable results in therapy engagement, symptom reduction, and sustained recovery for co-occurring conditions—especially when care is integrated and evidence-based.9
Insurance coverage for co-occurring disorder treatment—supporting both behavioral health and substance use recovery—varied based on your plan and provider network. Most major insurance plans, including Medicaid, are required to cover evidence-based care for integrated conditions, but the specifics (like in-network access or number of sessions) can differ. Industry leaders find that outpatient and telehealth models are increasingly covered due to their cost-effectiveness and flexibility for people balancing daily responsibilities.9
To find treatment that accommodates neurodivergent needs like ADHD or autism, start by asking providers about their experience with neurodevelopmental differences and whether they offer adaptive therapy options. Research shows that programs adjusting for sensory preferences, flexible communication styles, and structured routines help neurodivergent individuals engage more fully and achieve better outcomes for behavioral health and substance use recovery.2
Recognizing when professional support is needed can make a crucial difference in recovery outcomes. Warning signs include persistent struggles with daily functioning, intense or worsening symptoms like anxiety, depression, or cravings, repeated relapses despite self-help, or feeling unable to manage emotional distress alone. Research shows that only 14.5% of people with co-occurring behavioral health and substance use conditions receive treatment for both, highlighting how easily people can overlook the need for specialized help.1
Starting integrated treatment for substance use and behavioral wellness can often begin promptly, but the exact timing depends on provider availability and your specific needs. Many telehealth and outpatient programs offer quick access to an initial assessment—sometimes within a few days—especially in regions where virtual care is expanding.9 However, high demand or limited local resources may occasionally result in short waiting periods.
The typical cost of integrated mental health and addiction treatment can vary widely depending on the type of care, insurance coverage, and geographic location. While exact cost ranges are not specified in current research, studies show that outpatient programs—which often include both behavioral support and substance use treatment—are experiencing rapid growth due to their affordability and flexibility for individuals balancing work or family responsibilities.9
Yes, it is possible to receive treatment for co-occurring substance use and behavioral health conditions while working full-time. Outpatient and virtual care models are designed to support individuals who need flexible scheduling, allowing for therapy and support groups during evenings, early mornings, or lunch hours.9 Industry experts highlight that these adaptable options mean you don’t have to sacrifice your career to prioritize mental wellness or addiction recovery.
Improvement timelines with integrated treatment vary, but many people begin to notice changes in their emotional wellness or substance use patterns within the first few weeks. Studies reveal that early engagement—such as clinical assessment and starting therapy—can boost consistency and motivation, but sustained progress often builds over several months as skills and routines develop.5
Virtual treatment for substance use and behavioral health is designed with privacy as a top priority. Employers and colleagues are not notified when an individual seeks care unless the person chooses to share this information. Telehealth platforms must comply with strict privacy laws (such as HIPAA), which protect personal health details and treatment participation.9
Relapse is a common part of the recovery journey and doesn’t mean that treatment has failed. Many people experience setbacks as they work to build new habits and manage symptoms related to both substance use and behavioral wellness. Research shows that continuing care and long-term support systems, such as peer engagement and regular check-ins, help reduce the risk of relapse and support a return to progress after a slip.5
It can be challenging to know if substance use is connected to unrecognized trauma or post-traumatic stress disorder (PTSD), but there are some helpful self-reflection steps. Start by asking: Do you use substances to escape distressing memories, numb emotional pain, or cope with anxiety after reminders of past events? Studies reveal that nearly half of individuals with substance use disorder also meet criteria for PTSD, highlighting how trauma and addiction often overlap.7
Medication-assisted treatment (MAT) can serve as either a temporary recovery tool or a longer-term support, depending on a person’s needs and medical guidance. Some individuals use MAT for months to stabilize cravings and rebuild emotional health, then gradually taper off as they strengthen coping skills. Others may benefit from ongoing medication to support behavioral wellness and reduce relapse risk, especially if symptoms resurface with reduced doses.2
Integrated treatment is more effective than treating mental health and addiction separately because it addresses both conditions at the same time, closing the care gaps that often lead to relapse or incomplete recovery. Research demonstrates that people in integrated programs experience greater improvements in substance use, emotional stability, housing, and overall daily functioning compared to those who receive support for one issue at a time.2

November 6, 2025

January 6, 2026

November 6, 2025