
NH Individual Counseling: What You Need to Know
December 29, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
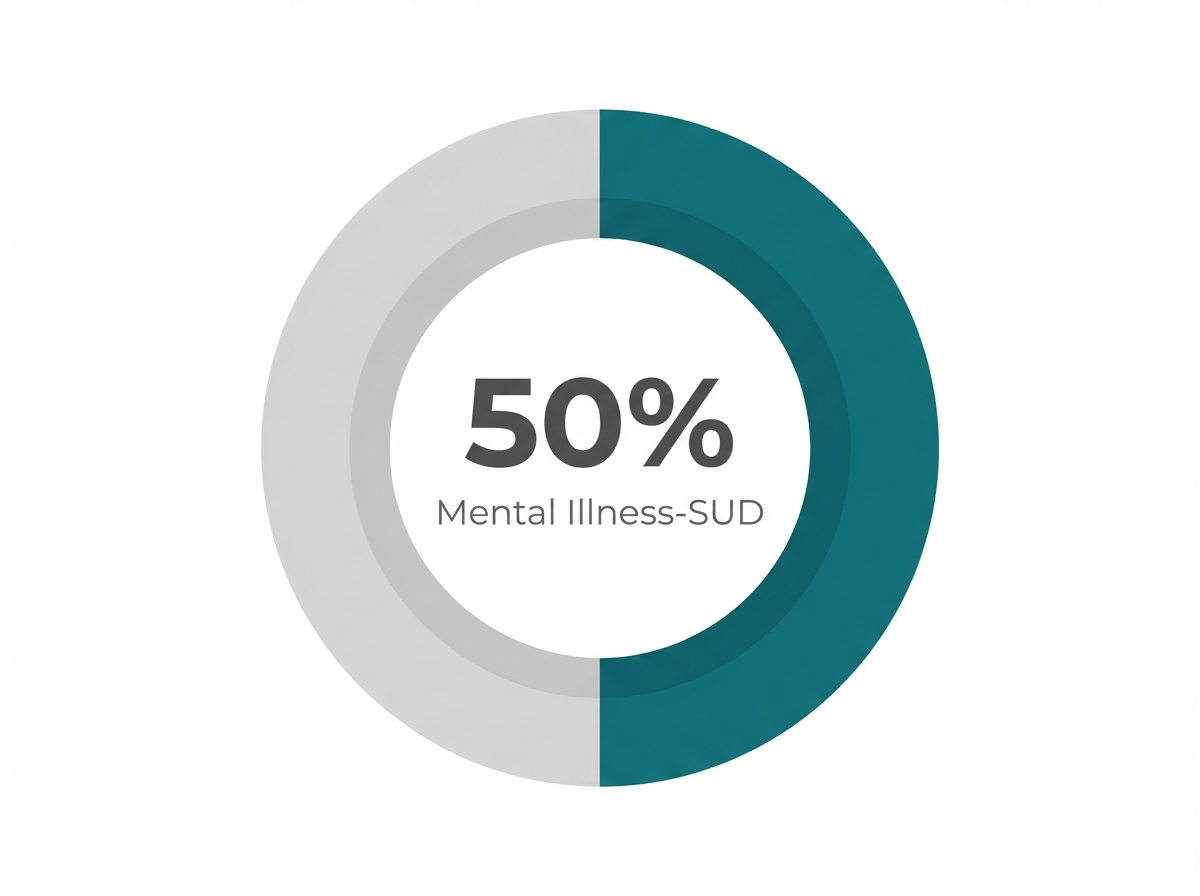
Psychiatric conditions and mental health issues frequently occur together, creating a complex relationship that requires specialized understanding. Research shows that approximately 50% of individuals who experience a dependency disorder will also face a psychological condition at some point in their lives, and vice versa.
This connection exists for several reasons:
Common dual diagnoses include depression and alcohol dependency, anxiety disorders paired with benzodiazepine dependence, and post-traumatic stress disorder alongside various patterns of addiction. Integrated treatment approaches that simultaneously address both psychiatric and behavioral health concerns offer the most promising outcomes for long-term wellness.
Checklist: Recognizing Co-Occurring Disorders
- Review your personal or family history for both substance use and mental health issues.
- Consider whether symptoms like anxiety, depression, or mood swings started before, during, or after substance use began.
- Ask your care team if your treatment plan addresses both substance use and mental health needs together.
For many, it might come as a surprise that having both a substance use disorder and another mental health condition is more common than facing just one or the other. National data reveals that about half of people who experience a mental illness in their lifetime will also encounter a substance use disorder2. Among adolescents receiving substance use care, over 60% are diagnosed with an additional mental health condition2.
Clinicians point out that these dual diagnoses often emerge because the conditions share risk factors and may even influence each other’s development. If you’re building a recovery plan, this path makes sense when you want to address the full picture, not just one set of symptoms.
Research reveals that both conditions are deeply linked through shared brain pathways and risk factors3. For instance, the brain’s dopamine system—responsible for motivation and pleasure—can be altered by both substance use and conditions like depression or anxiety. Trauma and long-term stress also disrupt the brain’s stress response system (the HPA axis), which is tied to both substance use and mental health conditions3.
Genetics play a role as well. People with a family history of either mental health issues or substance use are at higher risk for developing both. Understanding these shared roots helps explain why integrated treatment is so important.
Understanding the connection between addiction and mental health conditions naturally leads to an important next step: evaluating your own situation. Before choosing a treatment path, taking time for honest self-reflection can provide valuable clarity about which level of care might be most appropriate.
Start by examining when emotional or psychiatric symptoms first appeared. Did anxiety, depression, or other concerns exist before drinking or drug use began, or did they emerge afterward? Consider whether alcohol or drugs were initially used to cope with difficult emotions or situations.
As you reflect, ask yourself these specific questions to identify potential dual diagnosis concerns:
Certain warning signs indicate that professional assessment is essential rather than optional. If you've experienced suicidal thoughts, severe panic attacks that feel uncontrollable, or find yourself unable to function in daily life even when not actively using substances, immediate professional evaluation is critical.
Clinicians rely on questions like these to help distinguish between symptoms caused by substance use and those that signal underlying mental health conditions. This distinction is crucial: research shows that individuals with both substance use and mental health issues are more likely to face challenges in treatment, including a higher risk of not completing care5.
Decision Tool: Signs It’s Time to Seek Integrated Treatment
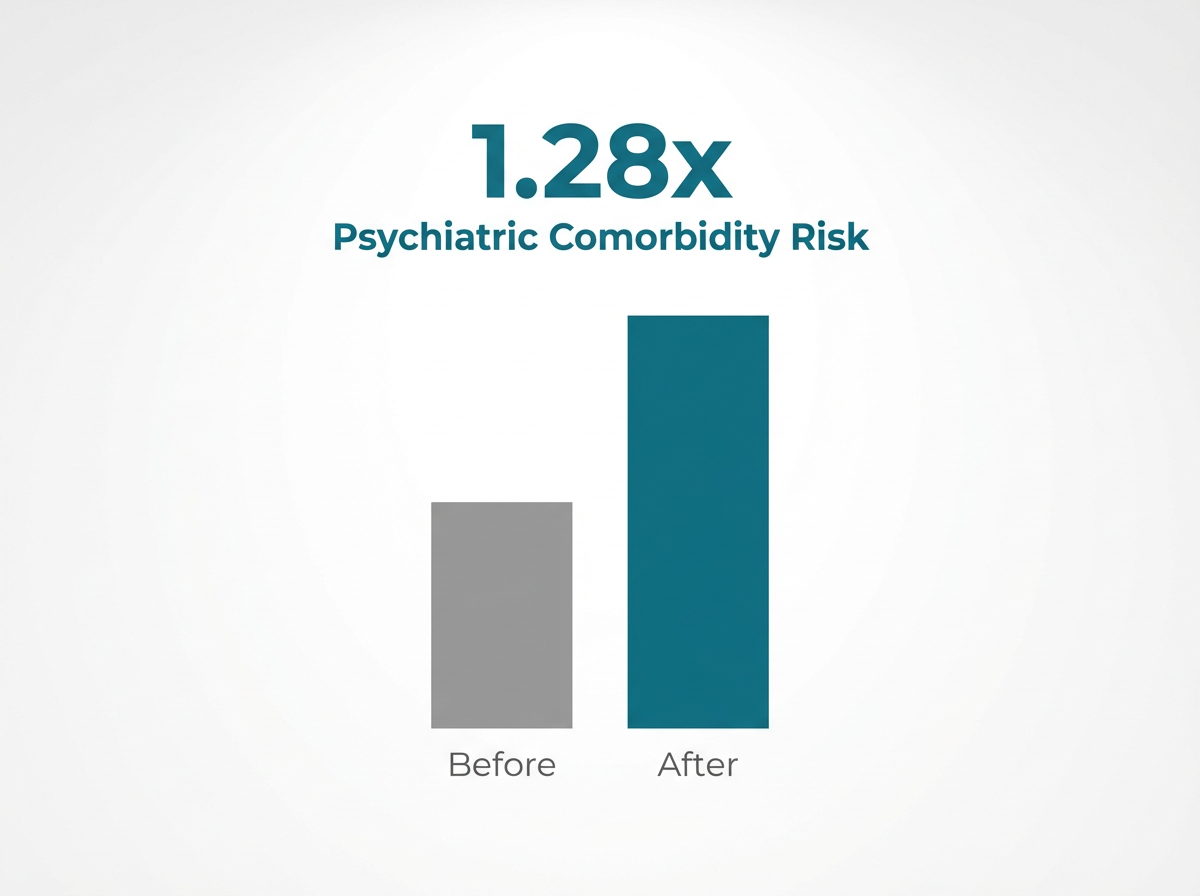
Integrated treatment is designed for individuals whose mental health issues and substance use challenges are deeply connected. Studies reveal that people with both conditions are 1.28 times more likely to struggle with treatment completion if their care isn’t coordinated5. Opt for integrated care when you want support that recognizes how these issues interact.
After identifying your psychological needs, the next step involves selecting a treatment approach that aligns with your specific situation. This decision requires balancing several factors: the severity of your symptoms, your current support system, insurance coverage, and whether you're managing dual diagnoses.
Understanding symptom severity helps determine appropriate care levels:
For individuals experiencing mild to moderate symptoms without addiction concerns, standard outpatient therapy or telehealth counseling may provide sufficient support. However, those with severe symptoms or dual diagnoses require more intensive intervention, such as Intensive Outpatient Programs (IOP) which provide 9-12 hours of structured treatment weekly.
| Feature | Integrated Care | Sequential Treatment |
|---|---|---|
| Approach | Treats mental health and substance use simultaneously. | Addresses one concern first (usually substance use), then the other. |
| Team Structure | Coordinated team (therapists, prescribers, coaches). | Separate providers, often uncoordinated. |
| Best For | Deeply connected symptoms; history of relapse. | Symptoms that are less intertwined; need for stabilization first. |
| Outcome | Lower relapse rates; improved daily functioning1. | Higher risk of non-completion if coordination fails5. |
Integrated care means treating mental health issues and substance use at the same time. Research shows this method leads to better recovery outcomes, especially for those whose symptoms overlap1. Sequential treatment works when symptoms are less intertwined, but studies reveal that people with co-occurring disorders who receive only single-focus care are 1.28 times more likely not to complete treatment5.
Criteria Guide: Making the Choice
- Consider Medication + Therapy if: Symptoms are moderate to severe, or you have experienced relapse when only using one approach.
- Consider Medication alone if: Therapy isn't enough to manage severe depression, anxiety, or cravings.
- Consider Therapy alone if: Symptoms are mild and you have a strong support network.
Deciding between medication, therapy, or a combination depends on how mental health issues and substance use affect you personally. Research shows that using both—such as combining Cognitive Behavioral Therapy (CBT) with medications like antidepressants or Medication-Assisted Treatment (MAT)—often leads to the strongest recovery outcomes1, 9.
Taking action within the next month can significantly impact long-term recovery outcomes. Research shows that the sooner someone begins treatment after recognizing a dependency issue, the better their chances of sustained recovery.
Schedule consultations with at least three treatment providers. During these calls, ask specific questions:
Progress Marker: By end of Week 1, contact 3 providers and schedule one initial appointment.
Establish concrete support connections. Attend one peer support meeting (SMART Recovery, AA, Refuge Recovery) even if just to observe. Identify your three biggest triggers in daily routines and plan alternatives. Remove all substances from your living space.
Progress Marker: By end of Week 2, attend one support meeting and identify 2 support people.
Attend all scheduled appointments, whether virtual or in-person. Start implementing one healthy coping mechanism daily—this could be a 20-minute walk or 10 minutes of meditation. Track your progress by noting daily wins and challenges.
Progress Marker: By end of Week 4, attend all scheduled sessions and practice coping mechanisms 20 out of 28 days.
The connection between mental health and substance use disorders isn't coincidental—it's a clinical reality that demands integrated care. As established at the outset, dual diagnosis treatment recognizes that lasting recovery requires addressing both conditions simultaneously, not as separate problems but as interconnected aspects of whole-person health.
Throughout this guide, you've explored the essential decision points for choosing addiction treatment: understanding whether you're facing co-occurring disorders, evaluating the appropriate level of care intensity based on your specific circumstances, and identifying providers equipped to deliver integrated treatment.
Recovery from addiction requires more than willpower—it demands comprehensive support, evidence-based treatment, and a sustainable path forward. The right combination of clinical expertise, peer support, and personalized care creates the foundation for lasting change.
Your next steps: Start by completing the self-assessment questions in Section 2 to clarify your treatment needs. Then use the decision framework in Section 3 to identify which level of care aligns with your situation. Finally, reach out to providers who specialize in dual diagnosis treatment and can offer the integrated approach your recovery deserves.
Recovery raises many questions, and having clear answers helps you move forward with confidence. While every person's journey is unique, certain questions come up consistently as individuals explore their options for sustainable recovery from co-occurring disorders.
The cost of integrated treatment for co-occurring mental health issues and substance use disorders varies widely depending on several factors, including your location, the type of services needed, and whether you have insurance that covers both conditions. Studies reveal that financial barriers are the most common reason people cannot access needed care for these challenges4. While some treatment providers accept insurance or Medicaid, others may require out-of-pocket payments. In general, care that includes therapy, medication management, and regular follow-ups will be more expensive than single-focus services. Virtual treatment can sometimes reduce costs by eliminating travel and offering more flexible scheduling.
Telehealth treatment has become a trusted option for addressing co-occurring mental health issues and substance use, especially in regions where in-person resources are limited. Research shows that virtual care can provide outcomes comparable to traditional face-to-face treatment, making it a strong choice for many individuals seeking support7. Telehealth allows people to access therapy, medication management, and recovery coaching from home, which can reduce barriers like transportation, scheduling conflicts, or stigma.
Experiencing relapse after previous treatment attempts is common for those managing both substance use and mental health issues. Integrated care takes a different approach by addressing both conditions at the same time, which research shows leads to stronger outcomes and a lower risk of dropping out of treatment compared to single-focus care1, 5. If past programs mainly focused on substance use or mental health separately, integrated care may help prevent important factors from being overlooked.
Knowing whether Medication-Assisted Treatment (MAT) is a good fit for your recovery depends on several factors. MAT is most often used for opioid use disorder, and it combines medications like buprenorphine or methadone with counseling to address both substance use and mental health issues. Research shows MAT can reduce overdose risk by up to 76% at three months and 59% at one year9. Virtual providers in Vermont, Massachusetts, Connecticut, and New Hampshire can guide you through this decision and help coordinate ongoing care.
Privacy is a top concern for many people seeking virtual treatment for substance use and mental health issues. By law, telehealth providers must protect your health information under HIPAA (the Health Insurance Portability and Accountability Act), which means your employer or colleagues do not have access to your treatment records without your explicit written consent. Virtual sessions are typically conducted on secure platforms, and appointment details are kept confidential.
Family involvement can be a powerful support in recovery, but it’s natural to worry about feeling micromanaged or losing a sense of independence. Research shows that when family members are included in psychoeducation or structured support sessions, outcomes improve—people are less likely to return to substance use and experience stronger overall well-being8. To keep things balanced, it helps to set clear boundaries: talk openly with your family about what kind of help feels encouraging versus what feels intrusive.
If your mental health symptoms get worse during early recovery, it’s important to act quickly and reach out for support. Start by contacting your care team—whether that means your therapist, counselor, or primary care provider—so you can review your symptoms together and adjust your treatment plan. Research shows that individuals with co-occurring mental health issues and substance use are more likely to face challenges in treatment, especially if new or worsening symptoms aren’t addressed right away5.

December 29, 2025

November 6, 2025

December 12, 2025