
Virtual Detox Program: Safe, Compassionate Virtual Detox with Pathfinder Recovery
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
Research suggests that up to 50% of adults with ADHD and a significant proportion of autistic adults will struggle with substance use disorders at some point in their lives—yet most addiction treatment programs remain fundamentally misaligned with how their brains work. This represents the first critical mistake in seeking care: assuming a neurotypical framework can serve everyone equally well. Finding a specialized neurodivergent recovery program is often the deciding factor between a cycle of relapse and sustainable, long-term well-being.
Most addiction treatment programs follow a neurotypical framework that assumes all participants process information, manage emotions, and respond to interventions in similar ways. This one-size-fits-all approach overlooks the distinct neurological differences that shape how neurodivergent adults experience both addiction and recovery.
Traditional group therapy settings often present significant barriers for individuals with autism spectrum disorder or ADHD. The emphasis on reading social cues, maintaining eye contact, and processing verbal information quickly can create overwhelming sensory and cognitive demands. When neurodivergent adults struggle in these environments, their difficulties are frequently misinterpreted as resistance or lack of motivation instead of being recognized as accessibility issues.
Standard treatment protocols also tend to underestimate the role of executive function challenges in addiction disorders. For someone who has ADHD, difficulties with impulse control, time management, and emotional regulation aren't character flaws—they're neurological realities that require specialized strategies. Similarly, autistic adults may turn to substances to manage sensory overload or social anxiety, yet few programs address these underlying needs.
The result is predictable: neurodivergent adults cycle through treatment programs that weren't designed for their brains, experiencing repeated setbacks that damage their confidence and hope for lasting recovery.
Mistake 2: Overlooking Therapist Training Gaps in Neurodiversity

A major misstep many people make is assuming that all therapists within a recovery program are prepared to support neurodivergent individuals. In reality, most therapists receive little to no formal education on autism, ADHD, or related neurodivergent conditions.
A recent study found just 2% of psychotherapists reported high knowledge of autism, while more than half had minimal or no autism-specific training1.
This gap can have serious consequences: therapists without neurodiversity expertise may misinterpret behaviors, miss underlying needs, or unintentionally reinforce masking and shame. Imagine someone with autism or ADHD entering a standard SUD program, seeking help. If their therapist lacks neurodivergent understanding, sessions might focus on "fixing" behaviors rather than supporting authentic self-advocacy or sensory regulation. This can leave individuals feeling misunderstood or even blamed for their struggles. Over time, this disconnect increases dropout rates and reduces the likelihood of lasting recovery.
What can be done? When considering a neurodivergent recovery program, always ask specific questions about the staff’s neurodiversity training and ongoing education. Look for programs that require specialized training, consult with neurodivergent advisors, and use evidence-based, affirming approaches. Taking these steps helps ensure therapy sessions are empowering, supportive, and truly tailored to neurodivergent needs.
Mistake 3: Relying on One-Size-Fits-All Treatment Models
A frequent pitfall for individuals seeking SUD support is enrolling in programs that treat every participant the same—regardless of neurotype. Many traditional recovery models use fixed schedules, standardized therapy groups, and uniform expectations around communication and participation. For someone who is neurodivergent, this can feel like being asked to wear a suit that just doesn’t fit. Industry experts point out that typical addiction interventions are often unsuitable for autistic adults, and rigid group sessions may actually increase discomfort or lead to early dropout8.
Imagine a person with autism or ADHD navigating a group therapy session filled with loud noises and rapid discussions. Instead of feeling supported, they might become overwhelmed, anxious, or misunderstood. Studies reveal that neurodivergent individuals are nearly nine times more likely than non-autistic peers to use substances to manage their unique symptoms7. That means a recovery program must be flexible and affirming, not just generic.
To avoid this mistake, look for a program that adapts its structure to individual needs—offering sensory accommodations, flexible scheduling, and communication options. Ask how the program tailors treatment to support neurodivergent strengths and preferences. These steps help ensure that each person’s path to recovery is both accessible and sustainable.
Many treatment programs assign counselors and therapists based on availability instead of specialized training in neurodivergent conditions. This approach creates a fundamental mismatch between the support needed and the support provided. When clinicians lack understanding of how ADHD, autism, or other neurodivergent conditions interact with addiction, they may misinterpret behaviors or apply strategies that work against natural neurological differences.
A provider unfamiliar with attention differences might view difficulty maintaining eye contact or fidgeting during sessions as disengagement or resistance, when these behaviors are simply part of how someone processes information. Similarly, a counselor without autism training might push for group therapy participation without recognizing that social processing differences make traditional group formats genuinely challenging, not just uncomfortable.
| Feature | General Addiction Provider | Neurodivergent Specialist |
|---|---|---|
| Behavior Interpretation | May view fidgeting or lack of eye contact as "resistance." | Recognizes these as self-regulation or processing styles. |
| Group Therapy | Mandatory, high-sensory group sessions. | Optional small groups, sensory breaks, or 1:1 alternatives. |
| Goal Setting | Standardized timelines and rigid compliance. | Flexible goals adapted to executive function capacity. |
The consequences extend beyond misunderstanding. Generic treatment plans often fail to account for the executive function challenges common in neurodivergent adults—difficulties with time management, task initiation, and working memory that directly impact treatment adherence. Without providers who recognize these patterns, individuals may be labeled as unmotivated or non-compliant when the real issue is a lack of appropriate accommodations. Effective treatment requires clinicians who understand neurodivergence as a core aspect of how someone experiences the world, not as a secondary consideration or behavioral quirk to overcome.
Mistake 5: Overlooking the Risk of Diagnostic Overshadowing and Misdiagnosis
One of the most damaging mistakes when searching for a neurodivergent recovery program is underestimating the risk of diagnostic overshadowing. This happens when a provider misinterprets neurodivergent traits—like social differences, sensory sensitivities, or communication styles—as signs of unrelated mental health conditions.
Research shows that nearly one in four autistic adults received a mental health diagnosis, such as a personality disorder or mood disorder, before ever being recognized as autistic6.
This misdiagnosis often delays access to effective support and can lead to treatments that don’t address the root causes of substance use. Picture someone seeking help for substance use challenges who is actually autistic but told their struggles are due to a personality disorder. Instead of receiving affirming, autism-informed care, they might end up in therapy that misses their true needs—leaving them feeling frustrated and unsupported. Studies reveal that this pattern is especially common among autistic women, with one in three reporting perceived misdiagnosis before their autism was identified6.
To avoid this mistake, choose a recovery program that takes time for thorough, specialized assessment and stays alert to the possibility of autism or ADHD—even when other diagnoses are present. Ask if the program routinely screens for neurodivergence and if staff receive training in recognizing less obvious presentations. These steps make it far more likely that individuals receive care tailored to who they truly are.
Mistake 6: Missing Autism-Affirming Care Standards
Selecting a program that lacks clear autism-affirming care standards is a mistake that can quietly undermine recovery. Many neurodivergent adults, especially those with autism, have tried programs where the focus is on "fixing" behaviors or enforcing neurotypical social skills, rather than building on each person’s strengths and identity. When the recovery environment expects masking—hiding autistic traits to fit in—individuals can feel invalidated, which research shows increases anxiety and can worsen substance use patterns4.
Instead, look for a recovery program that explicitly states its commitment to autism-affirming practices: celebrating neurodivergent ways of communicating, offering sensory-friendly spaces, and respecting individual needs without judgment. Ask if staff are trained to recognize masking and support authentic self-expression. Studies reveal that recovery outcomes improve when programs affirm autistic identity and avoid shame-based tactics4. To set yourself up for success, prioritize providers who partner with autistic advisors, use identity-affirming language, and adapt care to the lived experiences of neurodivergent individuals.
Many treatment programs overlook the sensory sensitivities and executive function challenges that commonly accompany neurodivergence. Individuals with ADHD, autism, or other neurodivergent conditions often experience heightened sensitivity to lights, sounds, textures, and smells. Traditional group therapy rooms with fluorescent lighting and crowded seating arrangements can trigger sensory overload, making it nearly impossible to focus on recovery work.
Executive function differences—affecting organization, time management, task initiation, and emotional regulation—also require specific accommodations. Standard treatment expectations like remembering multiple daily appointments, completing extensive paperwork independently, or managing complex medication schedules may set neurodivergent individuals up for failure without proper support systems in place. When programs fail to address these needs, people may appear "non-compliant" or "unmotivated" when they're actually struggling with unaccommodated neurological differences.
Effective neurodivergent-affirming care includes specific accessibility measures:
These modifications aren't special treatment—they're necessary accessibility measures that enable full participation in recovery.
Mistake 8: Underestimating the Impact of Overwhelming Group Therapy Environments
A frequent stumbling block for neurodivergent individuals in recovery is the exposure to group therapy environments that are loud, chaotic, or socially demanding. These traditional settings—often filled with rapid conversations, bright lighting, and little control over participation—can trigger sensory overload or social anxiety for those with autism or ADHD. Industry leaders find that such environments can actually increase distress, causing participants to withdraw or even leave treatment prematurely8.
For example, someone with sensory sensitivities might struggle to focus amid overlapping voices and background noise, while another person may feel pressured to conform to neurotypical social rules. These experiences don’t simply cause discomfort—they can actively block engagement and progress in the recovery process.
To avoid this mistake, ask whether the neurodivergent recovery program offers smaller, quieter groups, and choices about how and when to participate. Seek programs that allow for sensory accommodations, such as noise-canceling headphones or breaks, and encourage alternative forms of communication like written responses. These steps make it more likely that each participant can access support in a way that feels safe and sustainable.
Mistake 9: Accepting Inflexible Scheduling and Rigid Protocols
It’s easy to underestimate how much strict routines and unbending program rules can disrupt recovery for neurodivergent individuals. Many traditional addiction programs require participants to attend sessions at fixed times, complete standardized homework, or follow rigid participation protocols. For someone with executive function challenges—like trouble with planning, time management, or adapting to last-minute changes—these requirements can quickly become overwhelming rather than supportive. Research shows that neurodivergent individuals are nearly nine times more likely than non-autistic peers to use substances to manage their unique daily struggles, including difficulty with routine and transitions5.
Imagine someone with ADHD or autism trying to juggle appointments, group sessions, and paperwork, only to be penalized for missing a step due to forgetfulness or sensory overload. Instead of fostering progress, overly strict systems can trigger anxiety or reinforce feelings of failure, sometimes pushing individuals to leave treatment altogether.
To avoid this mistake, seek out a recovery program that offers flexibility: options for rescheduling, multiple session formats (like virtual or asynchronous check-ins), and individualized planning tools. Ask how the program supports participants with reminders, organizational aids, or alternative ways to meet requirements. These practical steps can help empower individuals to take part in recovery on their own terms and reduce unnecessary barriers.
Traditional addiction treatment often focuses exclusively on stopping drug and alcohol consumption without exploring the underlying reasons someone began using in the first place. For neurodivergent individuals, this approach misses critical connections between their neurological differences and patterns of dependency. Many people living with ADHD, autism, or other neurodivergent conditions discover that substances temporarily ease overwhelming sensory experiences, quiet racing thoughts, or help them feel more comfortable in social situations.
Without addressing these root causes, treatment becomes a cycle of stopping and starting instead of sustainable recovery. Effective treatment recognizes that dependency frequently serves a purpose—even if that purpose creates more problems than it solves. Perhaps stimulants helped someone focus before they received an ADHD diagnosis, or alcohol reduced anxiety in social settings for someone on the autism spectrum. Understanding these patterns allows treatment teams to develop healthier coping strategies that address the actual needs substances were filling.
Recovery programs that incorporate neurodivergent-affirming approaches help individuals identify their specific triggers, sensory needs, and executive function challenges. This foundation makes it possible to build coping skills that actually work for how their brain functions, instead of expecting them to succeed with strategies designed for neurotypical individuals. When treatment addresses root causes alongside problematic consumption patterns, lasting change becomes achievable.
Mistake 11: Overlooking Masking, Trauma, and Self-Medication Patterns
One of the most overlooked mistakes when seeking a neurodivergent recovery program is failing to recognize how masking, trauma, and self-medication are deeply intertwined with substance use for many autistic and ADHD adults. Masking—the exhausting effort to hide neurodivergent traits and "blend in"—often leads to chronic stress, anxiety, and even depression. Research shows that many autistic individuals use alcohol or other substances not to rebel, but to manage the intense social anxiety, sensory overload, and emotional fatigue that come from constantly camouflaging their true selves34.
For example, someone might use alcohol as a "social lubricant" to tolerate overwhelming events or to quiet the critical voice that says they must act neurotypical to be accepted. These coping strategies can become deeply ingrained, especially for those who spent years undiagnosed or misunderstood.
To avoid this mistake, look for a program that acknowledges masking and self-medication as survival strategies, not personal failures. Ask if the program uses trauma-informed care, supports unmasking in safe environments, and helps participants find healthier ways to manage stress. By understanding the "why" behind substance use, programs can offer more meaningful, lasting recovery support.
Mistake 12: Ignoring Untreated ADHD and Co-Occurring Conditions
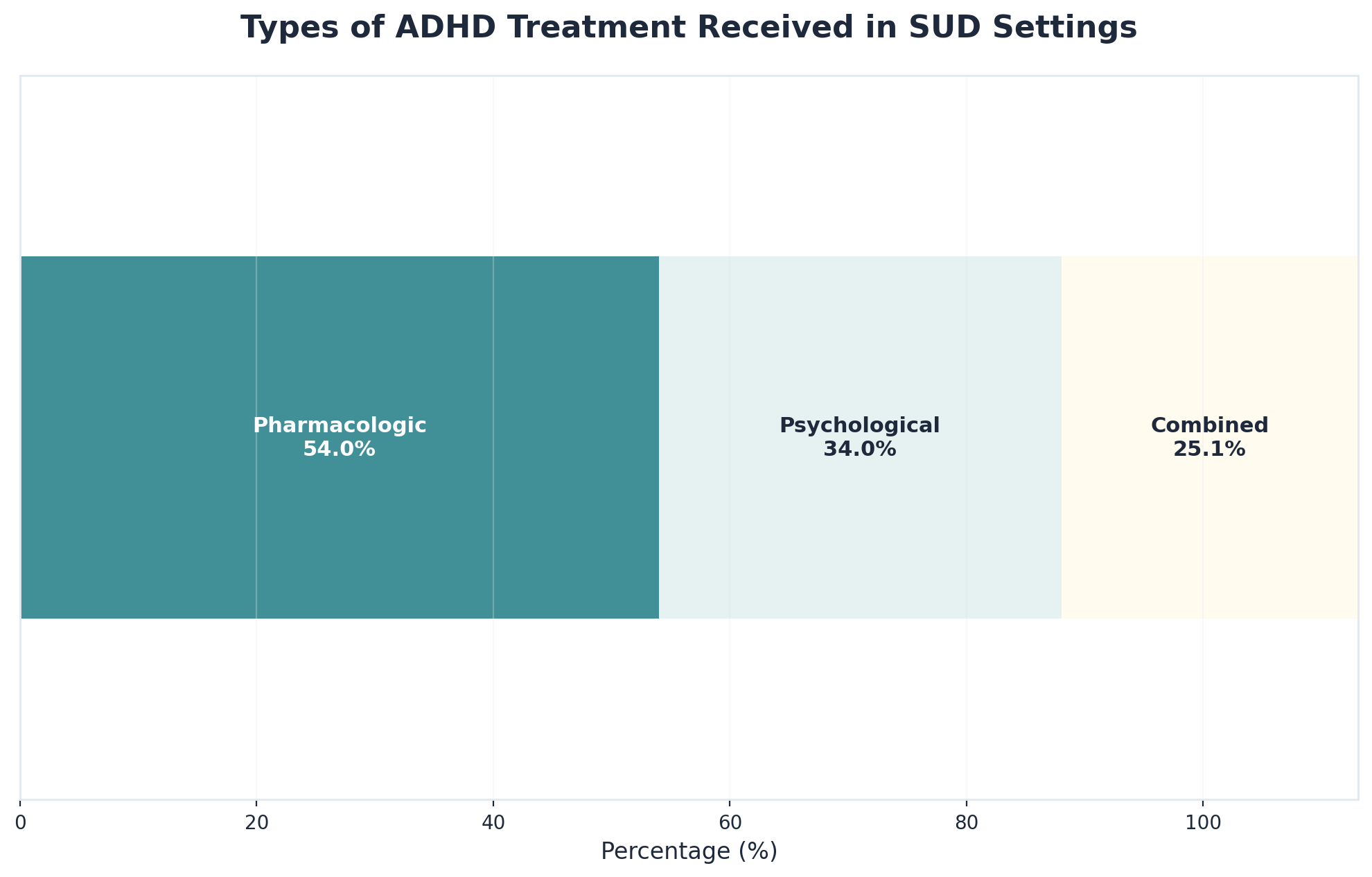
Another major mistake when looking for a recovery program is not addressing ADHD and other co-occurring conditions alongside substance use. People with ADHD, for example, are almost three times more likely to develop substance use disorders compared to those without ADHD7. When ADHD symptoms like impulsivity, restlessness, or trouble focusing go unrecognized and untreated, individuals often struggle to engage in recovery, stick with routines, or manage cravings. This can make recovery feel like an uphill battle.
Research shows that successful recovery is much more likely when programs treat both substance use and ADHD (or other conditions) at the same time, rather than one after the other9. Yet, many programs still overlook or delay treating ADHD, which can lead to repeated relapses or dropouts. Imagine trying to focus on building new coping skills while your brain is constantly distracted or overstimulated—it’s no wonder so many people give up.
To avoid this mistake, look for a program that screens for ADHD and other co-occurring conditions, and can coordinate care for both. Ask how the program supports medication management, executive function coaching, and flexible routines. These steps help address the real reasons behind substance use, giving each person a stronger chance at lasting progress.
Now that we've examined the common pitfalls—the misdiagnoses, the one-size-fits-all approaches, and the treatments that ignore neurodivergence—let's focus on what actually works. Creating a sustainable recovery plan requires acknowledging how neurodivergence intersects with addiction. The most effective approaches combine evidence-based addiction treatment with neurodivergent-affirming strategies that honor how your brain works.
Start by seeking providers who understand both addiction disorders and neurodevelopmental conditions. This dual expertise ensures treatment addresses the complete picture instead of treating conditions in isolation. When interviewing potential providers, ask specific questions: "How do you modify treatment approaches for neurodivergent clients?" and "What experience do you have treating co-occurring ADHD/autism and substance use disorders?" Look for credentials like CASAC (Credentialed Alcoholism and Substance Abuse Counselor) combined with specialized training in neurodevelopmental conditions. Red flags include providers who dismiss your self-knowledge, insist all clients follow identical protocols, or suggest you're "using neurodivergence as an excuse." Seek programs offering integrated care that weaves together addiction support and co-occurring mental health treatment.
Build routines that accommodate your specific needs. People managing ADHD may benefit from structured check-ins and visual reminders, while those on the autism spectrum might prioritize predictable schedules and sensory-friendly environments. For example, Maya, a client with ADHD and alcohol use disorder, found success when her treatment team helped her create a recovery routine with phone alarms for medication, body-doubling sessions for difficult tasks, and permission to fidget during group therapy—accommodations that made sobriety sustainable rather than exhausting. Recovery tools should work with your neurology, not against it.
Connect with neurodivergent peer support communities where shared experiences create genuine understanding. These connections combat isolation while providing practical strategies from others navigating similar challenges. Remember that recovery isn't linear, and setbacks don't erase progress. Neurodivergent brains may require different timelines and approaches. What matters is finding sustainable strategies that support long-term wellness while respecting your authentic self.
Yes. Prescribed medications for diagnosed conditions like ADHD are considered essential medical treatment, not a violation of recovery principles. Most evidence-based treatment programs distinguish between therapeutic medication management and substance misuse. The key is working with a psychiatrist who understands both addiction and neurodevelopmental conditions—ideally one who can coordinate with your recovery team. If you encounter resistance in a support group or program, ask to speak with the clinical director about their medication policy. Many programs now explicitly state that prescribed psychiatric medications are compatible with recovery.
Start by searching directories like Psychology Today or CHADD's professional directory using filters for both "substance use" and "ADHD" or "autism." When contacting potential providers, ask specific questions: "How do you adapt CBT techniques for clients with executive function challenges?" or "What accommodations do you offer for sensory sensitivities?" Request a brief consultation call to assess their knowledge. Red flags include providers who dismiss your self-diagnosis, suggest you can't have both conditions, or insist neurodivergent traits are just addiction symptoms. Green flags include familiarity with terms like "double empathy problem," willingness to provide written summaries, and flexible session structures.
Request written agendas before group sessions, permission to use fidget tools or stim discreetly, and breaks during long meetings. Ask if you can record sessions or receive written summaries of key points. For residential programs, inquire about single rooms, flexible meal times, or quiet spaces for sensory breaks. Request advance notice of schedule changes when possible. If traditional talk therapy feels unproductive, ask about body-based approaches, art therapy, or walk-and-talk sessions. Don't hesitate to request specific communication preferences—such as email over phone calls, or direct language instead of implied expectations. These aren't special favors; they're legitimate accessibility needs.
Proactively educate your treatment team about your baseline behaviors. Provide written information explaining that stimming, social withdrawal after overstimulation, or rigid routines are coping mechanisms, not red flags. Create a personalized relapse prevention plan that distinguishes between your typical neurodivergent patterns and actual warning signs. For example, your plan might note: "Normal for me: needing alone time after groups, repeating phrases when stressed. Actual warning signs: skipping meals entirely, isolating for multiple days, romanticizing past use." If providers still conflate the two, request a team meeting to clarify or consider seeking a second opinion. Your recovery plan should accommodate your neurotype, not pathologize it.
If you find yourself in a recovery program that doesn’t seem to understand neurodivergence, you’re not alone—and you’re not stuck. Many neurodivergent adults start treatment only to realize their needs around sensory sensitivity, communication, or routines aren’t being met5. First, make a list of what’s not working for you—such as overwhelming group sessions, inflexible schedules, or a lack of understanding from staff. Bring these concerns to your treatment provider using clear, non-confrontational language: "I need quieter spaces to focus," or "Flexible scheduling would help me participate more fully."
Advocating for your needs is a strength, not a weakness. If the program isn’t willing or able to adapt, consider seeking a referral to a neurodivergent recovery program that offers sensory accommodations, flexible routines, and staff with neurodiversity training. Research shows that outcomes improve and dropout rates decrease when individuals are supported in ways that fit their neurotype5. Remember, you have the right to care that respects and responds to your unique needs.
To verify that a therapist truly has neurodivergent expertise—beyond just general mental health training—start by asking direct, specific questions. Don’t settle for vague answers about "working with everyone" or "having some experience with neurodivergent clients." Instead, ask about their formal education: Have they completed autism- or ADHD-specific training or continuing education? What percentage of their caseload is neurodivergent? Do they participate in supervision or consult with neurodivergent advisors? Research shows that only 2% of surveyed therapists report high knowledge of autism, while more than half have minimal or no autism-specific training1.
Request examples of how they adapt sessions for sensory sensitivities, communication styles, or executive function needs. A therapist with genuine neurodivergent expertise will be able to describe practical accommodations and identity-affirming approaches, not just generic empathy. You can also look for credentials, memberships in neurodiversity-focused organizations, or ask if they use a neurodivergent recovery program model. Trust your instincts—if their responses are dismissive or unclear, it’s a sign to keep searching for a provider who is equipped to meet your unique needs.
Yes, virtual recovery treatment can be effective for people with autism or ADHD—especially when the program is thoughtfully designed for neurodivergent needs. Telehealth offers benefits like reduced sensory overload, flexible scheduling, and the comfort of participating from a familiar environment. Research shows that many neurodivergent individuals struggle with traditional group settings due to sensory sensitivities or social anxiety, making virtual options a valuable alternative5.
The most effective neurodivergent recovery program will provide options for video, audio, or even text-based sessions, and will adapt communication to fit a participant’s preferences. Studies reveal that when barriers like transportation or sensory overwhelm are lowered, engagement and outcomes improve5. However, virtual care works best when providers still offer accommodations—such as breaks, clear instructions, and visual aids—and maintain strong communication. If you’re considering virtual treatment, ask whether the program has experience supporting neurodivergent adults and how they tailor sessions for autism and ADHD. This way, you can access support that meets your unique needs and helps you move forward confidently.
Receiving a personality disorder diagnosis before discovering you are autistic is more common than many people realize. Research shows that nearly one in four autistic adults, and one in three autistic women, experienced at least one psychiatric misdiagnosis—most often a personality disorder—before their autism was recognized6. This process, called diagnostic overshadowing, can delay access to supportive care that truly fits your needs and may lead to treatments that feel invalidating or unhelpful.
If this happened to you, it’s important to know that your experience is valid and you are not alone. Start by seeking a provider who understands both autism and substance use—ideally through a neurodivergent recovery program. Bring your full diagnostic history to your intake appointment and share how your understanding of yourself has changed. Ask your new provider how they differentiate between autistic traits and personality disorder features, since the overlap can be confusing even for experienced clinicians.
If you feel comfortable, request a re-evaluation or second opinion from a specialist with neurodiversity expertise. Programs that prioritize autism-affirming care will focus on your strengths and lived experience—not just old labels. Remember, it’s never too late to get the right support that truly fits who you are6.
Yes, harm reduction approaches can be appropriate—and often essential—for neurodivergent individuals with substance use concerns. Research and clinical experience both suggest that abstinence-only models may not meet the unique needs of autistic people or those with ADHD, as these programs often ignore the underlying reasons for substance use, such as managing sensory overload or social anxiety8. In some cases, a strict focus on abstinence can even increase stress and lead to disengagement from care.
A neurodivergent recovery program should offer harm reduction options alongside traditional supports. This might include strategies for safer substance use, flexible participation, and step-by-step goals that recognize each person’s context. Studies reveal that when neurodivergent adults feel respected and empowered to set their own recovery pace, they are more likely to stay engaged and make meaningful progress5.
The key is to find a program that listens to your needs and offers choices—not just one-size-fits-all rules. If you’re considering harm reduction, ask how the program tailors support for neurodivergent individuals and whether advisors with lived experience help shape policies. This way, care can be safer, more respectful, and better matched to your unique journey.
Explaining your sensory needs to a treatment provider doesn’t make you difficult—it makes you empowered and proactive about your recovery. Many neurodivergent adults worry about being perceived as “challenging” when they ask for accommodations, but research shows that sensory sensitivities are a genuine, common part of the neurodivergent experience5. Most providers want you to succeed, and clear communication helps them make the right adjustments.
Start by making a short list of sensory experiences that support your focus and comfort (like dim lighting, soft voices, or breaks during sessions). Use specific, non-blaming language when sharing your needs: try “I focus best in quieter spaces,” or “Bright lights are distracting for me—are there options for softer lighting?” If it feels easier, write your needs down and hand them to your provider or email them in advance.
A neurodivergent recovery program will be familiar with these requests and should offer practical solutions. Remember, self-advocacy is a strength, not a problem. If a provider responds negatively or dismisses your needs, that’s a sign to look for a more supportive fit. Your comfort and safety are essential to successful recovery5.
Recovery from addiction is possible for neurodivergent individuals when treatment honors rather than ignores their neurological differences. Throughout this article, we've explored how conventional approaches often fail ADHD, autistic, and other neurodivergent people—not because recovery is impossible, but because the methods weren't designed with their needs in mind.
The key mistakes to avoid are clear: don't accept treatment that dismisses your neurodivergence as an excuse, forces you into communication styles that drain rather than support you, ignores sensory needs, applies neurotypical social expectations, or separates addiction treatment from neurodivergent-informed care. These aren't minor preferences—they're fundamental barriers that can undermine recovery before it truly begins.
When neurodivergent individuals find treatment providers who understand executive function challenges, respect different communication styles, accommodate sensory needs, and integrate neurodivergent-affirming approaches with addiction care, sustainable recovery becomes achievable. The combination of proper accommodations, therapists trained in both addiction and neurodevelopmental differences, and treatment plans built around how your brain actually works creates the foundation for lasting change.
If you're a neurodivergent person struggling with addiction, you deserve treatment that sees your whole self—not care that asks you to mask, conform, or overcome your neurodivergence to access recovery. Seek providers who explicitly understand neurodivergent experiences, ask about accommodations during initial consultations, and prioritize finding approaches that work with your brain rather than against it. Your path to recovery should honor who you are, not require you to become someone else.

November 6, 2025

November 6, 2025

February 6, 2026