
Virtual Addiction Treatment: Virtual Treatment that Meets You Where You Are
November 6, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
The journey through pregnancy and early motherhood brings profound physical and emotional changes that can create unexpected vulnerabilities. Depression during pregnancy affects up to one in seven women, and when left unaddressed, it can become a significant risk factor for problematic drinking or drug use. Finding effective support for moms in recovery is essential, yet the overwhelming feelings of sadness, anxiety, or disconnection during pregnancy may lead some mothers to seek relief through alcohol or other substances, creating a cycle that's difficult to break without proper help.
What makes this situation particularly challenging is the wall of silence that surrounds it. Society often expects mothers to radiate joy and gratitude, making it incredibly difficult for those struggling with both recovery and emotional wellness concerns to speak up.
"The stigma attached to addiction becomes even more intense when motherhood enters the picture, leaving many women isolated in their struggles. They worry about judgment from healthcare providers, family members, and their communities—fears that can prevent them from seeking the help they desperately need."
For parents managing recovery while raising children, the practical barriers to treatment can feel insurmountable. Between school drop-offs, meal preparation, work schedules, and the countless other demands of running a household, finding time to attend traditional treatment programs becomes nearly impossible. The logistics of arranging childcare, taking time off work, and traveling to appointments create additional stress during a period when stability and support are most critical.
Recognizing these complex barriers—the emotional, social, and logistical challenges that mothers face—some treatment providers have developed approaches specifically designed for the realities of family life. Accessible, flexible options that integrate behavioral health support with addiction treatment can help address the interconnected nature of these struggles. Virtual care models, for instance, allow mothers to receive comprehensive support from home, eliminating transportation and childcare obstacles while providing the privacy that helps reduce stigma and encourage honest conversations about recovery.
This section explores the strong link between prenatal depression and substance use, helping readers understand why addressing both is essential for effective support for moms in recovery. You'll know you've learned it when you can explain how depression during pregnancy can influence substance use—and vice versa.

Studies reveal that depression during pregnancy often goes hand-in-hand with substance use, creating a challenging cycle to break. For example, over 30% of pregnant women in substance use treatment report moderate to severe depression, and these mental health symptoms can increase the likelihood that a mother turns to substances to cope2. This connection highlights why integrated care for maternal mental health and substance use is so critical.
Imagine trying to patch a leaky boat while it’s still taking on water—treating only one side of the problem leaves moms at risk of relapse and ongoing distress. Effective help must address both prenatal depression and substance use together.
When a mother experiences depression, her emotional pain can become overwhelming—like carrying a heavy backpack that gets heavier each day. Research shows that over 30% of pregnant women in substance use treatment also have moderate to severe depression2. This burden often leads to using substances as a way to numb sadness or anxiety, creating a cycle that is hard to break.
The need for emotional relief may drive a mom to reach for drugs or alcohol, even when she wants to stop, especially if she lacks social support or access to mental health care. For many families, breaking this cycle means finding help that addresses both depression and substance use together. That’s why effective support for moms in recovery must include mental health care, ongoing social support, and compassionate resources for maternal well-being.
Research shows that women who use substances during pregnancy are not just a little more likely to experience postpartum depression—they face a 3.67x higher risk compared to mothers who did not use substances1. For moms working toward recovery, this means the postpartum period can feel like walking a tightrope with extra weight, where every step carries added emotional risk. This is where maternal mental health support and targeted resources become critical in preventing setbacks and promoting healing.
Stigma acts like an invisible wall: it doesn’t just blame mothers for their struggles, but also makes it hard for them to reach out for substance use and emotional support7. Studies reveal that fear of being judged or reported to authorities leads many women to avoid treatment, even when they want to get better5. For moms, this stigma is often stronger than for other groups, especially with added pressure from societal expectations around parenting and maternal mental health.
For many mothers, the idea of asking for help brings more than just worry—it brings genuine fear that reaching out will lead to being judged as an unfit parent or trigger CPS involvement. Studies reveal that the possibility of losing custody or facing legal consequences keeps many mothers away from treatment, even when they want to recover5, 10. This fear is worsened by stigma around maternal mental health and substance use, making it feel safer to hide struggles than to risk family separation.
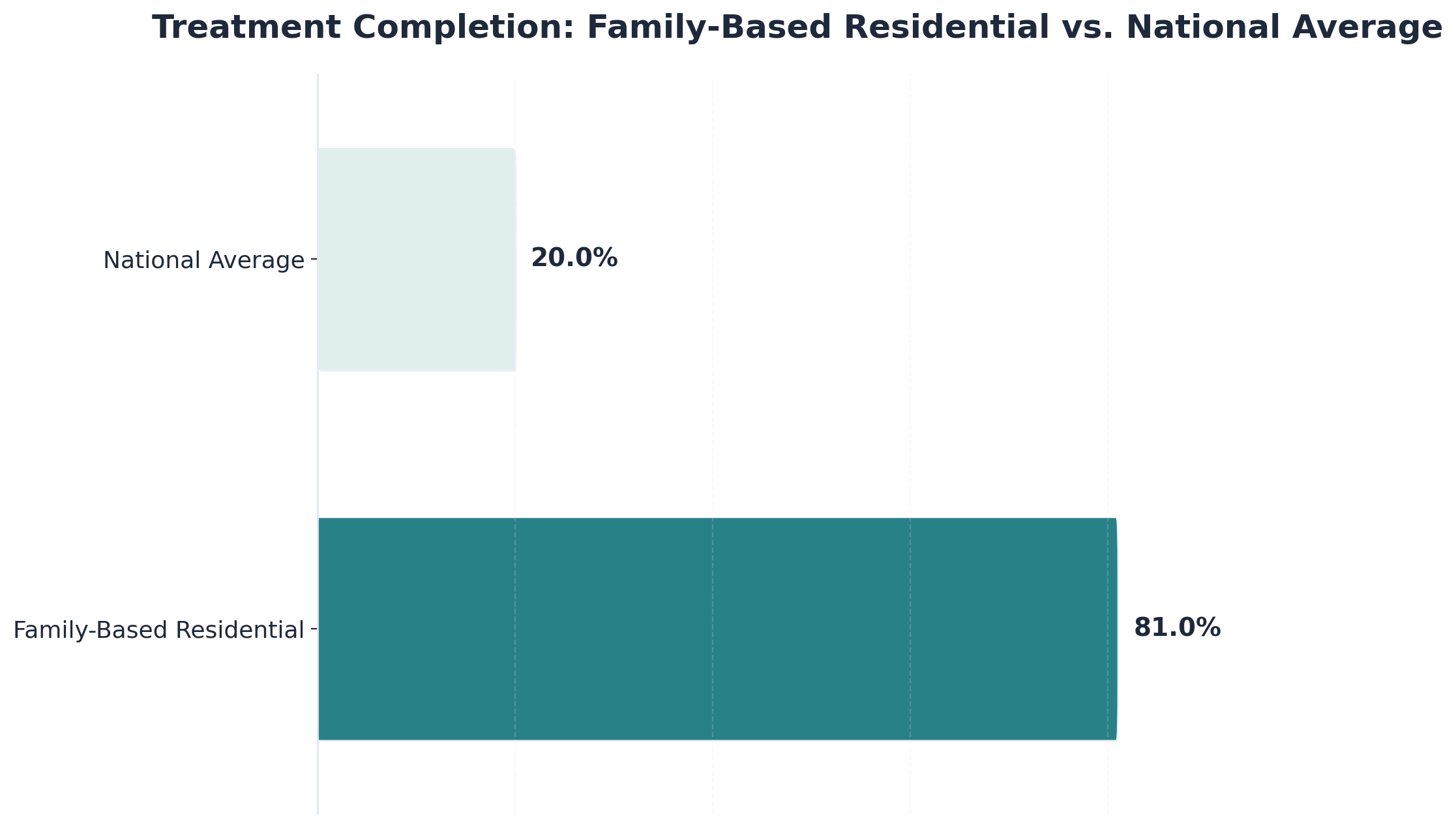
Traditional treatment programs often require rigid schedules, lack childcare, and separate moms from their children—making it nearly impossible for working mothers to attend or complete treatment. Research shows that only about 20% of moms finish standard programs, compared to 81% completion in family-based residential programs, which allow women to stay with their children and offer flexible services9. Without access to maternal mental health support and family-friendly care, many moms simply can’t get the help they need.
The postpartum period demands an extraordinary balancing act, and for mothers managing addiction recovery, the challenge intensifies dramatically. A therapy appointment scheduled at 2pm conflicts with school pickup. A support group meets during the only hour available for meal prep. The pharmacy closes before childcare arrangements can be made. These aren't hypothetical scenarios—they're the daily reality for mothers trying to maintain sobriety while meeting the relentless demands of family life.
The time-management puzzle becomes particularly complex when recovery requirements collide with parenting essentials. Attending a mandatory outpatient program means finding three hours of childcare, three times per week. Completing daily check-ins and journaling exercises competes with preparing meals, helping with homework, and managing bedtime routines.
Even simple acts of self-care—taking prescribed medications on schedule, attending twelve-step meetings, or practicing mindfulness—require carving out moments that simply don't exist in a day already stretched beyond capacity.
| Feature | Traditional Outpatient Rehab | Virtual Support for Moms |
|---|---|---|
| Time Investment | Fixed hours (e.g., M/W/F 9am-12pm) | Flexible (Naptime, Evenings) |
| Childcare | Required (Must leave home) | Not Required (Care from home) |
| Commute | 30-60 mins travel time | 0 mins (Instant access) |
| Privacy | Public waiting rooms | Private, encrypted video |
Sleep deprivation compounds every challenge. When nighttime feedings interrupt rest, maintaining the emotional regulation necessary for recovery becomes exponentially harder. Decision fatigue sets in: Should you attend the evening support group or use that precious hour to prepare tomorrow's lunches? Is it worth the logistical complexity of arranging a sitter for a therapy session, or can it wait another week? Each choice carries weight, and the cumulative burden of these daily negotiations can threaten the stability that recovery requires.
This is where accessible, personalized care becomes essential. Pathfinder offers integrated behavioral health treatment alongside addiction support, designed specifically for the realities of maternal life. Serving individuals in Vermont, Massachusetts, Connecticut, and New Hampshire, their virtual platform eliminates the logistical nightmares of arranging transportation and childcare for in-person appointments. Women can access evidence-based treatment from their own homes, during naptime or after the children are in bed, making therapeutic support fit into the demanding rhythm of family life rather than competing with it.
For moms, recovery isn’t just about attending appointments—it’s balancing a long to-do list that rarely takes a break. Imagine trying to complete a puzzle, but the pieces keep shifting as kids need attention, laundry piles up, and work deadlines approach. Research shows that mothers face significant scheduling conflicts, limited childcare, and inflexible program hours, all of which can block access to maternal mental health support or substance use care5. Emotional support for mothers and flexible treatment options, like virtual care, are vital for making recovery possible within busy family routines.
For mothers balancing work, childcare, and home responsibilities, finding time for treatment often feels impossible. Studies highlight that inflexible program hours and long waitlists mean moms must choose between attending appointments and meeting their families’ needs5. This can delay or derail access to maternal mental health support or substance use care, especially for those without backup childcare. Emotional support for mothers and programs that offer flexible scheduling—like evening or virtual sessions—can help break down these time-related barriers.
Getting to treatment isn’t always as simple as hopping in the car—especially for moms juggling work and childcare. Research finds that transportation gaps and long travel distances can make it nearly impossible for mothers to attend regular appointments, particularly in rural areas or when public transit is limited5. Scheduling barriers, like programs only running during business hours, add another layer of difficulty for those with unpredictable routines. Emotional support for mothers and flexible options such as telehealth have been shown to lower these barriers, helping more women access the care they need.
The first year postpartum is often described as a crossroads for mothers navigating both healing and new parenthood. Research shows that relapse rates reach as high as 80% during this time, even though many women stop using substances while pregnant4. The sudden shift from pregnancy to caring for a newborn brings intense stress, sleep deprivation, and emotional changes—all of which can trigger old coping patterns. For mothers, this period can feel like walking a tightrope without a safety net, especially if access to maternal mental health support or emotional support for mothers is limited.
Research shows relapse rates can reach 80% for mothers in their first year after childbirth, despite many achieving abstinence while pregnant4. This high risk is often linked to the sudden loss of structure and support after delivery, combined with major life changes like sleep deprivation, hormonal shifts, and increased emotional demands. Without ongoing maternal mental health support or consistent emotional support for mothers, old coping patterns can return quickly. The shift from pregnancy-focused care to the realities of caring for a newborn can leave moms feeling overwhelmed and isolated, making it difficult to maintain recovery goals.
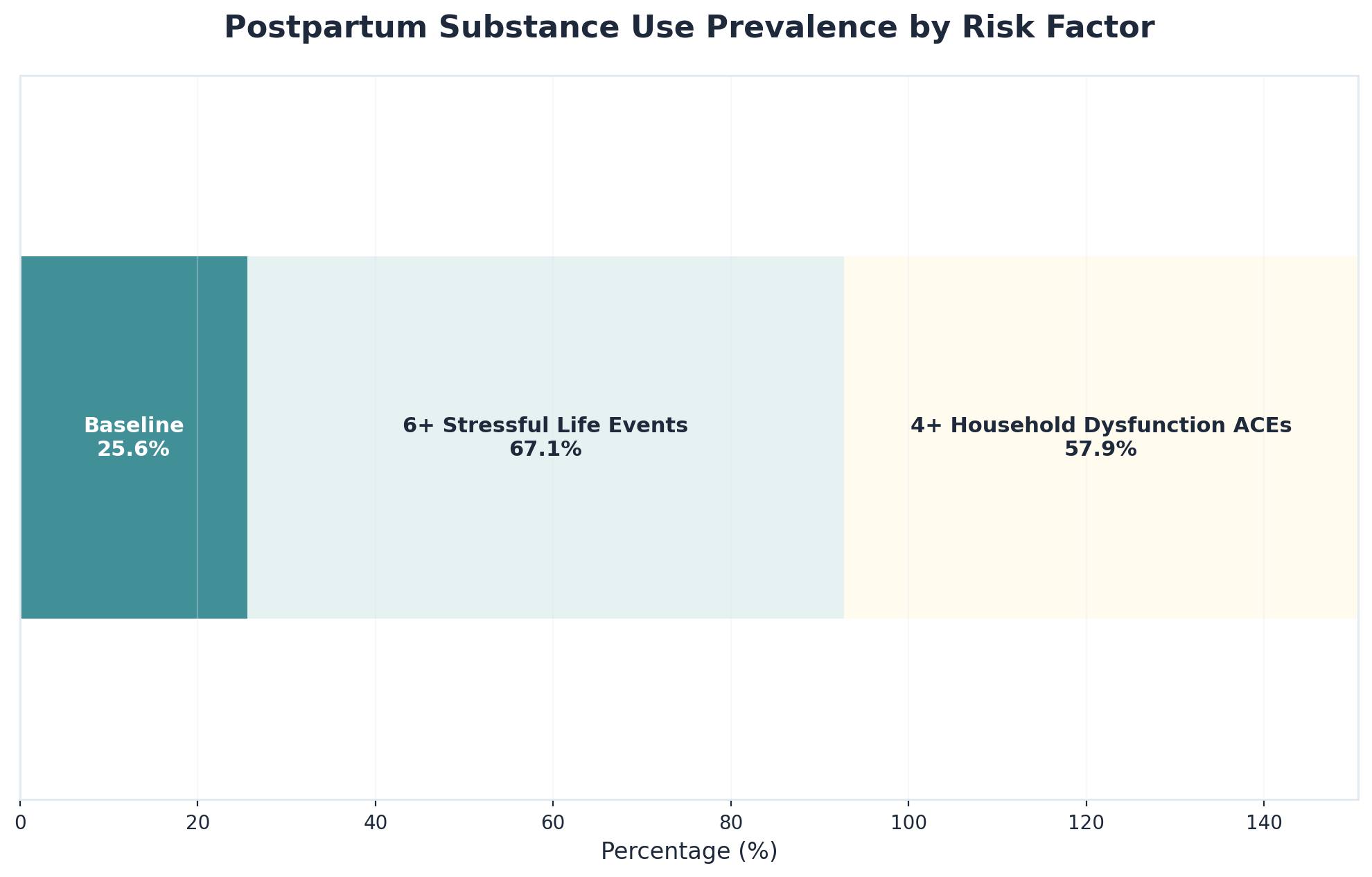
Stressful life events, like losing a job, relationship problems, or housing instability, can feel like sudden storms for mothers during the fragile first year after childbirth. Studies show that postpartum women who experienced six or more major stressors had a 67.1% rate of substance use, and those with four or more adverse childhood experiences (ACEs) faced a 57.9% rate—far higher than those with fewer stressors3. Trauma, whether from the past or recent events, can add another layer of emotional pain, making it harder to use healthy coping skills. That’s why emotional support for mothers and trauma-informed care are essential parts of effective maternal mental health support.
Recovery doesn't happen in isolation—it requires a network of understanding, practical help, and emotional support. For mothers navigating sobriety while managing households, careers, and children's needs, building this support system presents unique challenges. The demands of daily life often make it difficult to attend traditional treatment programs or support groups, leaving many feeling isolated precisely when connection matters most.
Creating an effective support system starts with identifying trustworthy people who can provide different types of support. Partners might handle morning routines on therapy days or take over bedtime duties when cravings intensify in the evening. A trusted neighbor could become the go-to person for emergency childcare during support group meetings. A sister or close friend might serve as the designated "check-in person"—someone to text during difficult moments who responds without judgment. The key is matching specific needs with specific people, rather than expecting one person to provide everything.
Communication strategies make these support systems work in practice. One mother established "recovery time" on her family calendar—blocking out Tuesday and Thursday evenings just like soccer practice or piano lessons, signaling to everyone that this time is non-negotiable. Another created a simple code with her partner: "I'm at a 7 today" immediately conveyed she needed extra help without lengthy explanations in front of the kids.
Effective support systems look different for everyone, but they share common elements. Consider Maria, who arranged with her mother-in-law to watch the kids every Wednesday afternoon—not for errands, but specifically for recovery activities like attending meetings or simply resting. Or Jennifer, whose partner took over all evening responsibilities on her therapy days, protecting that time as sacred. Virtual treatment options have expanded possibilities further, allowing access to specialized care during naptime or after bedtime. The most successful support systems combine multiple strategies: telehealth therapy for convenience, in-person connections for accountability, family help for practical needs, and structured routines that make recovery a visible, respected priority rather than something squeezed into leftover moments.
Virtual care is like having a lifeline that meets moms where they are—at the kitchen table, during naptime, or after work hours. Research shows that digital health and telehealth solutions help mothers overcome major obstacles such as transportation, childcare, and rigid program hours, leading to higher engagement and better outcomes9. These virtual models offer maternal mental health support and substance use care through video visits, secure messaging, and online groups, designed to fit real-life family routines. Emotional support for mothers becomes more accessible, and the stigma or fear tied to in-person visits can be reduced when care happens in a familiar, private setting.
Telehealth works like a bridge connecting moms to vital care, right from their own home. By using video appointments, secure messaging, and digital check-ins, mothers can connect with maternal mental health support and substance use counseling without leaving their children or rearranging work shifts. Studies highlight that digital health and telehealth services break down common barriers such as lack of transportation, limited childcare, and rigid program hours, making it easier for moms to stay engaged in recovery and emotional support for mothers9.
MAT from home combines safe, evidence-based medications with virtual check-ins and support, allowing moms to manage substance use and mental health needs without frequent clinic visits. Research shows that digital health and telehealth solutions—including remote MAT—help mothers overcome transportation, childcare, and scheduling barriers, all while improving engagement with maternal mental health support9. Emotional support for mothers and integrated care options can be woven into these programs, reducing stigma and making it easier to stick with recovery.
Integrated support is like weaving a safety net with both strong and flexible threads: substance use treatment is one piece, but maternal mental health care and emotional support for mothers are equally important. Studies show that over 30% of pregnant women in substance use treatment screen positive for moderate to severe depression, and more than 40% report postpartum depression symptoms2. When programs address both addiction and mental health needs together, moms are more likely to stay engaged and make progress in their recovery journey2.
Support for moms in recovery works best when mental health support, addiction care, and practical family strategies come together—whether it’s through counseling, peer recovery coaching, or resources for emotional well-being. For personal use, this means seeking out programs or providers who look at the whole picture, not just one piece. For business application, providers can design care models that coordinate mental health services, addiction treatment, and family involvement for better results.
For many mothers, recovery is not just about stopping substance use—it’s also about managing persistent feelings of sadness or worry. Studies show that over 30% of pregnant women in substance use treatment have moderate to severe depression, and more than 40% experience postpartum depression2. Anxiety often travels hand-in-hand with these symptoms, making daily life feel overwhelming and unpredictable. Think of depression and anxiety like invisible weights: when left untreated, they can pull mothers back toward old coping habits, making recovery much harder.
Effective support for moms in recovery brings mental health care and addiction support together. This might include counseling that addresses both substance use and emotional well-being, or peer support that acknowledges the impact of anxiety and mood swings. Programs that treat these conditions side by side—rather than in isolation—help mothers build resilience, boost confidence, and stay on track with recovery.
Family involvement acts like an anchor, helping mothers feel less isolated and more motivated to stay on track. Studies reveal that concern for children and the desire to provide care are major motivators for moms seeking treatment, while emotional distance or lack of support from family can predict relapse4. Programs that include family not only increase engagement but also help maintain custody and strengthen the parent-child bond—key parts of maternal mental health support and emotional support for mothers.
The expansion of telehealth has fundamentally transformed addiction treatment accessibility, particularly for parents who previously faced impossible choices between seeking help and managing family responsibilities. Virtual recovery programs now offer evidence-based treatment through secure video platforms, allowing individuals to access professional support from their own homes. This shift has removed many traditional barriers—commute time, childcare logistics, and schedule inflexibility—that once made treatment unreachable for countless mothers.
When evaluating virtual recovery programs, look for providers offering comprehensive services rather than just basic counseling. Effective programs should include individual therapy, group sessions, medication management when appropriate, and care coordination with other providers. Verify that clinicians are licensed in your state and that the platform meets HIPAA security standards. Ask about their approach to co-occurring conditions like depression or anxiety, which frequently accompany substance use challenges. Programs should also provide crisis support options and clear protocols for situations requiring in-person intervention.
Creating an effective home treatment space doesn't require a dedicated room, but does need intentional planning. Identify a spot where you can close a door or establish privacy during sessions—even a bedroom or parked car can work. Use headphones to maintain confidentiality and minimize distractions. If possible, schedule sessions during predictable quiet times: naptime, after bedtime, or when a partner can engage the children.
Maximizing virtual treatment effectiveness requires active participation strategies. Keep cameras on when possible to build stronger therapeutic connections. Take notes during sessions and review them between appointments. Engage fully in group sessions by sharing your experiences and supporting others. Between scheduled sessions, many programs offer peer support groups, educational resources, and check-in tools—use them. Recovery thrives on connection, and virtual platforms can facilitate meaningful relationships when you approach them with openness. Providers like Pathfinder Recovery and similar services throughout New England now offer these comprehensive virtual programs, making personalized, flexible treatment a realistic option for mothers balancing recovery with the demands of family life.
Pathfinder recognizes that every mother’s recovery journey is unique. That’s why their model is built on flexible scheduling, allowing moms to attend appointments and groups around nap times, school pickups, and work shifts. Their telehealth services—available in Vermont, Massachusetts, Connecticut, and New Hampshire—remove transportation and childcare barriers that often keep women from maternal mental health support or substance use care. Research shows that digital health and virtual care options designed for mothers lead to higher engagement and long-term success compared to traditional in-person programs9.
Pathfinder’s model treats flexibility as a core feature, not just a bonus. Moms can book virtual appointments during nap times, after bedtime, or between school pickups—so care fits seamlessly into real life instead of the other way around. Research shows that digital health and telehealth solutions offering this kind of flexibility lead to higher engagement and better outcomes for mothers needing maternal mental health support and emotional support for mothers9. By removing the need for travel and allowing mothers to keep parenting responsibilities front and center, Pathfinder’s approach helps ensure recovery support is not just available, but actually practical for busy families.
Pathfinder’s virtual care goes far beyond video calls. Their approach combines secure telehealth appointments, peer recovery coaching, group sessions, and digital resources for maternal mental health support—all from the comfort of home. Family involvement is encouraged, making it easier for loved ones to join sessions, learn new support skills, and strengthen the recovery environment. Research shows that mothers are more likely to engage in treatment and experience lasting results when family-based and virtual services are available, as seen in programs with 81% completion rates compared to just 20% for traditional models9.
Starting recovery can feel overwhelming, especially with all the emotional and practical demands mothers face every day. Research shows that virtual, flexible options for maternal mental health support and substance use care dramatically improve treatment engagement and completion rates for moms9. These personalized resources—like telehealth sessions, online peer groups, and family-inclusive support—help break down barriers such as transportation and scheduling, making it easier to get help without disrupting your daily routine.
For many moms, fear of judgment or concern about who might find out can feel like a locked door between them and the help they need. Studies highlight that stigma and the possibility of child protective services involvement are major reasons mothers hesitate to seek treatment, even when flexible, virtual options exist5, 10. Confidential telehealth services offer a private, judgment-free setting—think of it like having a conversation behind a closed door, where only you choose who’s included.
Sustaining recovery is about more than just the first step—it’s about creating a stable foundation for yourself and your loved ones. Research shows that mothers who have access to flexible, family-based programs and consistent emotional support are much more likely to complete treatment and avoid relapse9. Tools like regular virtual check-ins, family involvement in sessions, and daily self-care routines help keep recovery on track. Emotional support for mothers and maternal mental health resources are essential for weathering life’s ups and downs, and teaching children healthy coping skills along the way.
Starting the conversation about needing support can feel overwhelming, but honesty creates the foundation for healing. Consider choosing a calm moment with a trusted family member and expressing your feelings directly: "I've been struggling with [specific challenge], and I need professional support to work through this." Many mothers find it helpful to come prepared with information about the treatment approach you're considering. Remember that asking for help demonstrates strength and commitment to your family's wellbeing, not weakness.
Virtual care eliminates this significant barrier entirely. Through telehealth services, mothers can attend therapy sessions, counseling appointments, and group support meetings from home—during nap time, after bedtime, or while children are at school. This flexible approach means you don't need to arrange transportation or childcare, making treatment accessible even when resources are limited. Pathfinder Recovery's virtual platform serves families throughout Vermont, Massachusetts, Connecticut, and New Hampshire, bringing professional support directly to where you are.
Proactively seeking treatment actually demonstrates responsible parenting and commitment to your children's wellbeing. Courts and child welfare agencies view voluntary treatment positively, recognizing that parents who address challenges head-on are investing in their family's future. Confidential therapeutic support through licensed providers is protected by privacy laws, and choosing to pursue wellness shows the kind of judgment and care that strengthens families rather than threatening them.
Recovery timelines vary significantly based on individual circumstances, challenges being addressed, and personal goals. Some mothers benefit from short-term focused interventions lasting several weeks, while others find ongoing support over months or years most effective. Integrated behavioral health treatment adapts to your progress and changing needs. The key is that treatment remains flexible around your family responsibilities, allowing you to maintain consistency without sacrificing your role as a parent.
Setbacks are a common part of the recovery journey, not signs of failure. Effective treatment programs recognize this reality and provide compassionate support to help you understand what triggered the setback and develop stronger coping strategies moving forward. The goal isn't perfection—it's progress. Having professional support means you're never alone when challenges arise, and each experience becomes an opportunity to build resilience and deepen your understanding of sustainable wellness practices that work for your life.
Yes, you can access treatment while breastfeeding, and many recovery programs—including virtual care options—recognize the importance of supporting mothers during this stage. Providers offering support for moms in recovery will work closely with you to find safe, evidence-based care that considers both your health and your baby’s well-being. For example, medication-assisted treatment, counseling, and maternal mental health support can often be safely integrated with breastfeeding, though your provider will review your specific circumstances and any medications involved. Research shows that flexible, virtual models make it easier for mothers to get the help they need, even while managing postpartum demands like breastfeeding and infant care9. Emotional support for mothers and access to maternal mental health resources are available, ensuring you don’t have to choose between your child’s needs and your own healing.
Pathfinder takes confidentiality and privacy seriously, offering secure, HIPAA-compliant telehealth services so mothers can access support for moms in recovery from the comfort of home. Virtual sessions are conducted on encrypted platforms, and all personal health information is protected by strict privacy policies—only you and your chosen care team have access to your records. Research shows that confidential, home-based care helps overcome barriers like stigma and fear of judgment, allowing more mothers to seek maternal mental health support and emotional support for mothers without worry5. If you have questions about how your information is used or stored, Pathfinder’s team is always available to review privacy policies and address your concerns, making your safety and trust their top priority.
Pathfinder Recovery currently serves individuals in Vermont, Massachusetts, Connecticut, and New Hampshire, providing specialized support for moms in recovery through a fully virtual, telehealth-based model. This means mothers seeking maternal mental health support and emotional support for mothers can access care from the comfort and privacy of their homes within these states. By prioritizing accessible, family-friendly recovery options, Pathfinder helps break down barriers like transportation and scheduling, making it easier to receive compassionate care where it’s needed most9.
No, you do not need to have childcare arranged before starting treatment—especially with virtual care options like those offered by Pathfinder. Many programs are designed with the understanding that mothers often juggle parenting without extra help. Flexible telehealth appointments, evening sessions, and family-inclusive services allow you to access support for moms in recovery without needing to secure outside childcare first. Research shows that digital and family-friendly models help mothers overcome practical barriers such as lack of childcare, transportation, or rigid scheduling, so you can begin your healing journey even as you care for your children at home9. This approach ensures maternal mental health support and emotional support for mothers are truly accessible, meeting you where you are.
Yes, Pathfinder can help if you have a history of trauma or adverse childhood experiences (ACEs). Their virtual support model is designed to address the unique needs of mothers who have experienced stressful life events or trauma, which research shows can sharply increase the risk of substance use and relapse in the postpartum period3. Support for moms in recovery at Pathfinder includes trauma-informed care, emotional support for mothers, and resources that focus on building resilience and coping skills—all delivered in a confidential, home-based setting. Maternal mental health support and peer coaching are woven into their approach, helping you work through the impact of past trauma while also managing substance use and parenting challenges. This integrated model makes it easier for moms with a history of ACEs to access compassionate, effective help without leaving home or worrying about stigma or exposure. If you’re seeking a recovery path that recognizes your whole story, Pathfinder’s services are equipped to support you every step of the way.
Virtual recovery support stands out from traditional rehab programs by offering flexibility, privacy, and family-friendly options that make healing more accessible for mothers. Instead of requiring travel or long stays away from home, virtual care lets moms connect to emotional support, maternal mental health resources, and substance use counseling right from their living room. Studies show that virtual models—using video visits, secure messaging, and online groups—help break down major barriers like transportation, childcare, and rigid scheduling, leading to higher engagement and better outcomes for mothers9. Unlike standard rehab, which can disrupt family life and often lacks specialized resources for moms, virtual support is designed to fit around parenting duties and real-life routines. Emotional support for mothers and integrated care for co-occurring mental health and substance use needs are woven into these digital services, making support for moms in recovery both practical and effective. This approach not only improves access, but also empowers mothers to prioritize their wellness without sacrificing family stability.
Virtual treatment is designed to make support for moms in recovery fit real family life, even with young children at home. With telehealth, mothers can join therapy or group sessions from their kitchen table, during naptime, or after kids are asleep—no need for travel or finding extra childcare. Research shows that flexible, digital care models help mothers overcome common barriers like transportation and rigid scheduling, leading to higher engagement and better outcomes9. Many programs offer options like after-hours appointments, secure messaging, and short check-ins, so care can adjust to a mom’s unpredictable routine. Emotional support for mothers and maternal mental health support can be accessed in a private, comfortable space, helping moms stay connected to their recovery journey while still being present for their children. If interruptions happen, providers understand and can work with you to reschedule or adapt sessions as needed, making virtual support a practical and compassionate solution for busy families.
Relapsing after a previous treatment program is more common than many realize—especially for mothers. Research shows that up to 80% of women experience relapse in the first year postpartum, often due to overwhelming stress, lack of ongoing support, or sudden life changes4. If you’ve relapsed, you’re not alone, and it’s never too late to try again. Support for moms in recovery is designed to meet you where you are, offering practical tools, emotional support for mothers, and flexible, judgment-free care that recognizes recovery as a journey. Virtual and family-based services can help you rebuild a foundation for healing, focusing on both substance use and maternal mental health support. Remember, each step forward counts, and reaching out again is a sign of strength—not failure.
Yes—Pathfinder is designed to address both substance use and postpartum depression together, providing integrated support for moms in recovery. While Pathfinder does not offer primary mental healthcare, their telehealth model specializes in treating co-occurring mental health needs (like depression or anxiety) alongside substance use disorder support. This approach is important because research shows more than 30% of pregnant women in substance use treatment experience moderate to severe depression, and over 40% report postpartum depression symptoms2. By combining maternal mental health support and substance use care in one virtual program, Pathfinder helps mothers access emotional support and practical tools that fit family life. This integrated care model is shown to improve engagement, reduce relapse risk, and support long-term wellness for mothers and their families2, 9.
After your first call, starting treatment can happen quickly—often within just a few days. Pathfinder’s virtual, family-centered approach is designed to minimize wait times, so once you complete an initial assessment, you’ll be matched with a care team and offered flexible scheduling for your first session. Research shows that digital and telehealth-based programs improve access for mothers by reducing common delays like travel and childcare barriers, making support for moms in recovery more responsive and accessible9. Emotional support for mothers and maternal mental health resources are available right from home, helping you take that first step at your own pace. If you have urgent needs or specific schedule requests, let your care coordinator know so they can prioritize your start date.
Yes, your partner or family members can absolutely participate in your recovery journey. Research shows that family involvement is a major motivator for mothers seeking support for moms in recovery, and it can help prevent relapse by reducing feelings of isolation and strengthening the parent-child bond4, 9. Many virtual and family-based programs encourage loved ones to join counseling sessions, learn new support skills, or attend group meetings—making emotional support for mothers even more accessible at home. Including your support network not only boosts engagement but also helps maintain family stability and improves overall outcomes for maternal mental health. Related approaches, such as peer recovery coaching and family-inclusive care, have been shown to increase treatment completion rates and support long-term wellness for both moms and their children9.
Yes, medication-assisted treatment (MAT) is considered safe and effective for many women during pregnancy and the postpartum period when prescribed and monitored by a qualified healthcare provider. MAT—including medications like buprenorphine or methadone—can help stabilize recovery, lower the risk of relapse, and improve overall outcomes for both mother and baby. Research shows that evidence-based MAT, especially when paired with emotional support for mothers and maternal mental health support, leads to better engagement and fewer complications compared to untreated substance use2. Every situation is unique, so a provider will tailor care to your needs, monitor for side effects, and coordinate with your prenatal or postpartum team. Support for moms in recovery often includes regular check-ins, counseling, and education about safe medication use, ensuring both your health and your child's well-being come first.
Recovery is possible when treatment adapts to the realities of parenting rather than demanding parents abandon their responsibilities to access care. Throughout this journey, one truth emerges clearly: maternal wellness and family stability are not competing priorities—they're deeply interconnected. When mothers receive support that acknowledges both their recovery needs and their parenting roles, they can build sustainable healing that strengthens the entire family system.
The hidden challenges facing parents working toward wellness extend far beyond what most people understand. There's the constant vigilance required to maintain sobriety while managing sleep deprivation, the guilt that surfaces during difficult parenting moments, and the fear of being judged by other parents, healthcare providers, or even family members. These struggles are real, valid, and deserve recognition rather than stigma. Yet when treatment models acknowledge these realities rather than ignoring them, parents discover they don't have to choose between their recovery and their children.
The barriers that have kept so many mothers from accessing support—transportation challenges, childcare limitations, inflexible scheduling, and the impossible task of fitting traditional programs into already overflowing lives—are not insurmountable. Virtual care models, peer support networks, trauma-informed approaches, and flexible treatment options are transforming what recovery can look like for busy parents. Solutions exist that eliminate the false choice between personal wellness and family responsibilities.
If you're a parent navigating recovery, know that you don't have to do this alone, and you don't have to wait for the "perfect time" to seek support. Start where you are: research treatment options that offer flexibility, reach out to providers who specialize in maternal mental health and addiction, or simply talk to one trusted person about what you're experiencing. In Vermont, Massachusetts, Connecticut, and New Hampshire, virtual care programs like Pathfinder Recovery are designed specifically around parental realities, but wherever you are, advocates and resources exist to help you find a path forward. Your wellness matters—not just for your children, but for you. Every small step toward support is a step toward the sustainable, compassionate healing you deserve.

November 6, 2025

January 6, 2026

November 7, 2025