Outpatient Treatment Explained
January 26, 2026
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
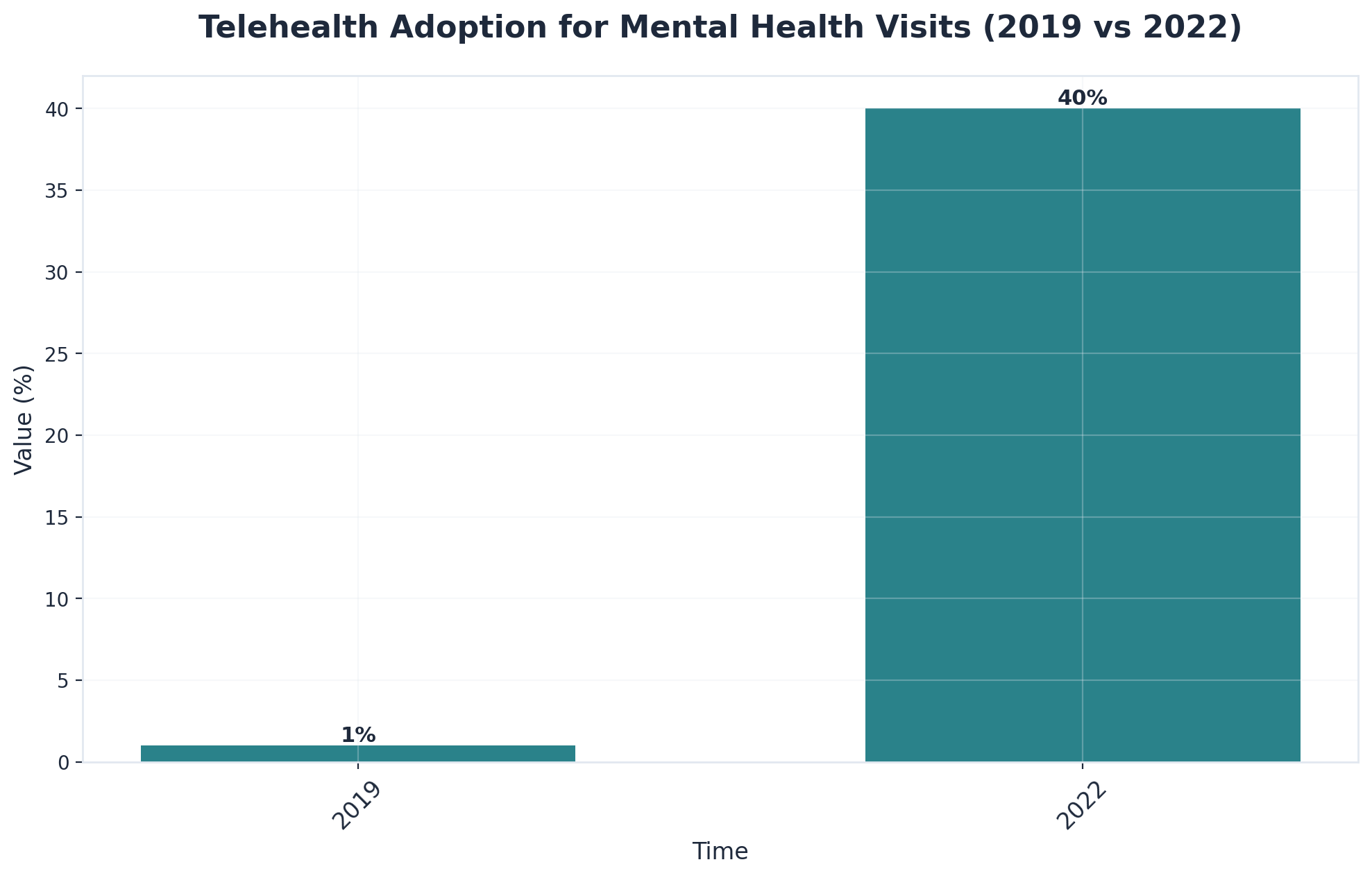
Accessing therapy from home has transformed how people manage psychological support, particularly for those navigating recovery alongside co-occurring psychiatric conditions. This remote care model connects you directly with licensed therapists through secure video platforms, effectively removing the logistical friction—like traffic, childcare, or distance—that often derails treatment plans.
The foundation of effective virtual therapy rests on the exact same clinical principles as in-person sessions. Licensed clinicians employ evidence-based treatment approaches, including Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and trauma-informed care. The primary difference is the medium: sessions occur through HIPAA-compliant video conferencing rather than face-to-face in an office.
"Virtual therapy isn't 'diet' therapy. It is the full clinical experience delivered through a different lens, often resulting in higher attendance rates because life gets in the way less often."
Think of therapy from home like having a familiar path through a challenging forest: when the path starts at your own front door, you are more likely to take the first step. One major reason home-based therapy is effective is that it removes common barriers. This makes it much easier for people in recovery to stick with appointments, leading to fewer missed sessions and more consistent progress10.
Three Core Advantages:
Clinical research consistently demonstrates that therapy from home is just as effective as in-person treatment for a wide range of mental health conditions. A large-scale analysis found no significant difference in outcomes between teletherapy and office-based care—patient satisfaction and progress were high in both settings1.
Once you understand the benefits, the next step is navigating the practical aspects of accessing care. The process typically begins with an initial assessment conducted through a secure video platform, where clinicians evaluate treatment needs and determine appropriate care levels.
Technical Requirements Checklist:
Insurance coverage for therapy from home has expanded significantly. Many plans now cover telehealth services at the same rate as in-person visits. For those in Vermont, Massachusetts, Connecticut, and New Hampshire, state policies have largely supported this parity. Always verify coverage details before beginning treatment to avoid unexpected costs.
Setting up your home therapy environment is like prepping for a meaningful meeting—you want a space that feels safe, private, and comfortable. Start by choosing a spot that is quiet and away from high-traffic areas. Even a cozy chair in the corner with headphones can help create a sense of separation from daily life.

Small touches like a notepad, a glass of water, or a calming item (like a soft pillow or plant) can enhance the experience. Make sure your device is charged and your internet connection is stable—studies reveal that a reliable tech setup increases satisfaction with remote sessions9.
Many people wonder if virtual sessions are truly private. Platforms designed for healthcare use strict security measures like end-to-end encryption and HIPAA compliance, so your conversations stay confidential4.
Virtual care is not limited to standard talk therapy. Major telehealth platforms have simplified access, connecting individuals with licensed therapists through secure video, messaging, and phone sessions. Insurance coverage has expanded significantly—over 80% of commercial health plans now cover telehealth services as of 2021.
Types of Specialized Virtual Care:
Delivering trauma-focused therapies through telehealth means individuals can process painful memories in a familiar and controlled environment. Research shows that trauma-focused therapies, including EMDR, deliver comparable outcomes when provided via secure video platforms, provided clinicians plan for safety7.
Safety Tip: Before a trauma session, prepare a "Grounding Kit" near your computer. This might include a textured object to hold, a strong scent (like peppermint oil), or a glass of ice water to help bring you back to the present moment if emotions become overwhelming.
Virtual MAT allows individuals to meet with providers, receive prescriptions, and get support for medication management from the privacy of their home. Research shows that MAT delivered through therapy from home leads to similar or even better retention rates compared to in-person care5.
Providers follow strict protocols for verifying identity and monitoring medication use. Clinicians use video visits to assess progress, adjust dosages, and answer questions, while digital tools help monitor symptoms.
Recovery requires daily tools and ongoing support to navigate challenges as they arise. Below are practical strategies for common home-based recovery scenarios.
Start with a systematic room-by-room assessment. Remove all substances and paraphernalia, including items in less obvious places like medicine cabinets, garage storage, and guest rooms. Look for associated items that might trigger memories—certain glassware or even decorative items linked to past use. Ask a trusted friend or sponsor to help identify items you might overlook.
Have a direct conversation early. Explain that your home needs to be substance-free or that certain areas must remain clear. If complete removal isn't possible, request that substances be stored out of sight in designated areas. Establish clear expectations about gatherings that might involve substance use.
Create designated spaces for recovery activities. Set up a meditation corner, establish a regular sleep schedule, and plan structured meal times. Fill the times when you previously used substances with scheduled activities—morning exercise, evening journaling, or virtual support group meetings.
Schedule daily check-ins with your sponsor or a supportive family member. Participate in virtual support groups to build relationships. Consider inviting trusted friends for regular recovery-focused activities like sober game nights. Proactively build connection into your week rather than waiting for loneliness to emerge.
Sample Crisis Plan Template:
My Emergency Contacts: 1. Therapist: [Name/Number] 2. Trusted Friend: [Name/Number] 3. Local Crisis Line: [Number] If I feel an urge to use: 1. I will wait 15 minutes. 2. I will call [Trusted Friend]. 3. I will use [Coping Skill, e.g., Box Breathing].
Many people seeking support for addiction have similar questions about virtual treatment options. Below are answers regarding insurance, privacy, and clinical outcomes.
Most major health insurance plans—including Medicaid and many commercial insurers—now cover virtual therapy sessions in the same way they do in-person visits. This shift was accelerated by federal and state policy changes, making it easier for individuals in Vermont, Massachusetts, Connecticut, and New Hampshire to access therapy from home without extra out-of-pocket costs6. Coverage typically includes therapy for substance use disorder and co-occurring mental health needs.
Yes. Many people use virtual therapy while sharing their space. The key is finding creative ways to ensure privacy, such as using headphones, positioning yourself in a quiet room with the door closed, or using a white noise machine. Research shows that these privacy steps make it easier for people to fully engage in therapy from home9.
Your therapist will follow a clear safety protocol. At the start of care, providers gather your location and an emergency contact4. If a situation becomes urgent (e.g., thoughts of self-harm), your therapist may pause the session to ensure you have immediate support, guide you to call 911, or contact your emergency person with your consent.
Research shows that virtual therapy outcomes for co-occurring substance use and mental health conditions are comparable to, and sometimes better than, traditional in-person treatment1,5. Home-based teletherapy often leads to fewer missed appointments and longer engagement in care10.
Most platforms recommend a minimum internet speed of 1-2 Mbps for both upload and download. A laptop, tablet, or smartphone with updated software works well. Using a wired connection or sitting close to your Wi-Fi router can help avoid interruptions.
Yes, many providers offer "hybrid care," which lets you move from remote sessions to office visits as life circumstances shift. This flexibility is especially useful for individuals managing substance use disorder and co-occurring mental health needs.
Yes. Research shows that therapy from home offers comparable outcomes to in-person care, with some individuals experiencing greater engagement due to reduced stigma and logistical barriers1. Virtual care can also introduce new approaches, such as trauma-focused therapies or medication-assisted treatment delivered remotely.
January 26, 2026

February 6, 2026