
EMDR Therapy Online: Accessible, Stigma-Free Therapy from Home with Pathfinder Recovery
November 7, 2025
Written and reviewed by the leadership team at Pathfinder Recovery, including licensed medical and clinical professionals with over 30 years of experience in addiction and mental health care.
If you have ever wondered what is telehealth, the answer is simpler than it sounds. It is the use of digital technology to connect you with doctors, counselors, and care teams without needing to visit a clinic in person. For people seeking help with substance use disorders, this means you can attend therapy, get medication, and receive support using your phone or computer.
In states like Vermont, Massachusetts, Connecticut, and New Hampshire, this technology has become a lifeline. It helps people in rural areas or busy cities get the same high-quality care they would receive in an office. Instead of driving for hours or taking time off work, you can log in from a private space and talk to your provider face-to-face through a screen.
"Telehealth is not just a video call; it is a complete way to deliver healthcare, education, and support over a distance."
Modern telehealth is more than just video chats. It includes secure texting, apps that track your health, and tools that let you send information to your doctor at any time. For those dealing with addiction and co-occurring mental health needs, this constant connection can make a huge difference in staying on track with recovery.
Telehealth is a big umbrella term. It covers all the ways technology helps you manage your health. This includes live visits, sending messages, and even remote monitoring tools. It is especially useful for people who cannot easily get to a doctor's office.
According to federal health resources, over 95% of health centers now use these tools to help patients.1 Whether you call it virtual care, digital health, or remote healthcare, the goal is the same: to bring care to you, wherever you are.
When we ask what is telehealth, we are talking about using the internet and devices to bridge the gap between you and your healthcare provider. It is like having a secure, private clinic right in your pocket. This allows for long-distance health care, patient education, and even public health services to reach people who need them most.1
You might hear the words "telehealth" and "telemedicine" used interchangeably, but they are slightly different. Think of telehealth as the whole school, and telemedicine as the classroom.
| Term | What It Covers | Example |
|---|---|---|
| Telemedicine | Clinical services only. | Diagnosing a cold or prescribing medication via video. |
| Telehealth | Clinical services + non-clinical support. | Provider training, administrative meetings, and patient education. |
Telemedicine focuses on the medical part, like treating a sickness. Telehealth includes that, plus things like education and administrative support.8
The COVID-19 pandemic changed everything for healthcare. When clinics had to close their doors, doctors and patients turned to screens. This shift made virtual care a normal part of life for millions of people.
In 2020, the number of Medicare telehealth visits jumped by 63 times compared to the year before.2 This massive increase proved that remote care could work, especially for people needing ongoing support for substance use and mental health.
During the pandemic, what is telehealth became a critical lifeline. The data shows a 63-fold increase in usage among Medicare users in 2020.2 This allowed people to stay safe at home while still seeing their doctors. It was particularly helpful for vulnerable groups who needed to stay connected to their care teams without risking exposure to the virus.
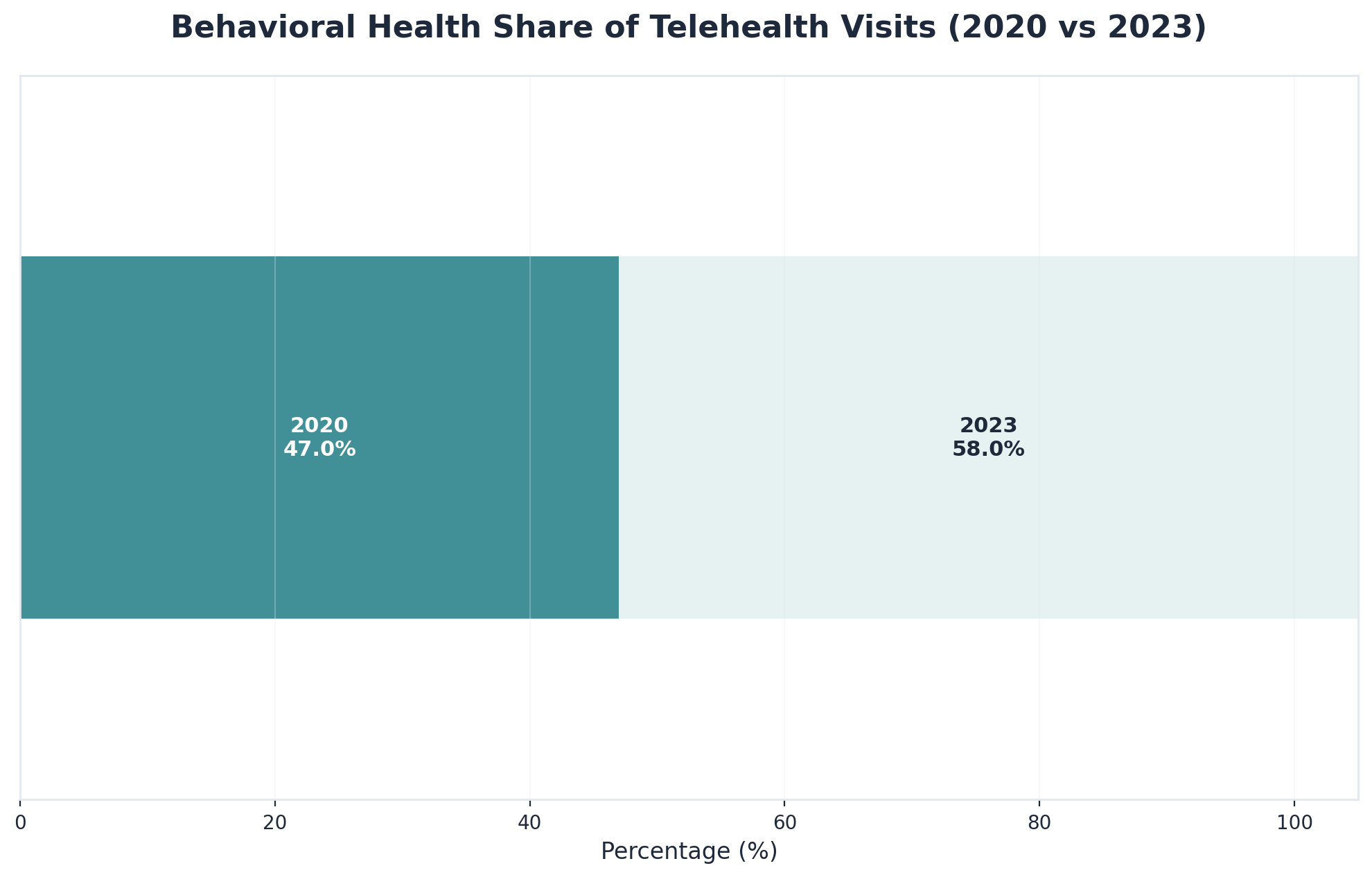
Even now, years later, digital health is going strong. About 71.4% of physicians still use telehealth weekly.3 It has become a standard way to treat behavioral health needs. In fact, in 2023, 58% of all telehealth visits were for mental and behavioral health.5 This shows that virtual care is here to stay.
Knowing what is telehealth is one thing, but understanding how it works is another. The process is designed to be as simple as possible. It usually follows these steps:

During the session, your provider can check your symptoms, discuss your treatment plan, and even prescribe medication. For addiction treatment, this might include counseling or checking in on your progress. The platforms used are secure and follow strict privacy laws to keep your information safe.
You do not need to be a tech expert. If you can use a smartphone or browse the web, you can use telehealth. Providers often send clear instructions to help you get started. This ease of use removes barriers like transportation and childcare, making it easier to stick with your recovery plan.
There are three main ways you might use telehealth. Each one serves a different purpose in your care.
These methods help connect patients and providers efficiently. More than 71% of physicians now use these tools every week to care for their patients.3
This is what most people think of when they ask what is telehealth. It is a live video meeting. You and your counselor can see and hear each other, allowing for a natural conversation. This is great for therapy and medical checks because the provider can see how you are doing, just like in an office.
Sometimes you don't need a live call. Asynchronous care lets you send a secure message with a question or an update. Your provider answers when they are free. Remote monitoring uses technology to keep an eye on your health between visits. This is helpful for managing ongoing conditions and keeping you connected to your care team.
To use these services, you need the right tools. A reliable internet connection is the most important part. You also need a device like a phone, tablet, or computer.
However, not everyone has easy access to these tools. About 28% of people in rural areas still lack high-speed internet.7 This "digital divide" can make it hard for some people to get the care they need.
High-speed internet, or broadband, is essential for clear video calls. Without it, the video might freeze or drop. You also need a device that can run the secure apps used by doctors. While technology is getting better, ensuring everyone has access to good internet is a major goal for healthcare leaders.7
Privacy is a top priority. Telehealth platforms must follow HIPAA rules. These are federal laws that protect your health information. They ensure that video calls are secure and that messages are encrypted. This means that what you say to your doctor stays between you and your doctor.10
Telehealth has changed the game for addiction treatment. It breaks down the walls that used to stop people from getting help. Things like living far away, not having a car, or working odd hours are no longer deal-breakers.
Consistency is key in recovery. If your car breaks down or you can't find a babysitter, you might miss an in-person appointment. With virtual care, you can still make that meeting. This helps you stay on track and lowers the risk of relapse.
Privacy is another huge benefit. Many people worry about being seen walking into a treatment center. With telehealth, you can get help from the privacy of your own home. This can make it much easier to take that first step toward recovery.
You might wonder if video visits are as good as seeing a doctor in person. The answer is yes. Research shows that telehealth is just as effective for treating substance use disorders.
Patients using telehealth are just as likely to stick with their medication and therapy as those who go to a clinic. In some cases, they do even better because it is easier to attend appointments.4
Studies have found that people receiving treatment online have similar success rates to those treated in person. This includes staying in treatment and avoiding substance use. When it comes to taking medication regularly, virtual care can be equally or even more effective.4
Telehealth programs have significantly increased engagement among people living in rural areas. One study noted a 143% increase in engagement for rural residents.4 This demonstrates that removing the barrier of distance allows more individuals to access and commit to the help they need.
Telehealth solves many practical problems. It removes the need for long drives and waiting rooms. It also helps people who might feel ashamed or anxious about seeking help in public.
By offering a private, flexible way to connect, digital health tools open doors for people who might otherwise go without care.4
For people with jobs, taking time off for rehab can be hard. Telehealth allows you to schedule sessions during lunch breaks or before work. The strict privacy rules mean you can get treatment without your employer or colleagues knowing, protecting your professional life while you heal.10
Life is busy. Telehealth fits into your schedule, not the other way around. You can book appointments at times that work for you. This flexibility leads to better attendance and better results in treatment.4
While telehealth is amazing, it is not perfect. There are still hurdles that make it hard for some people to use. We need to understand these challenges to make sure everyone gets a fair shot at recovery.
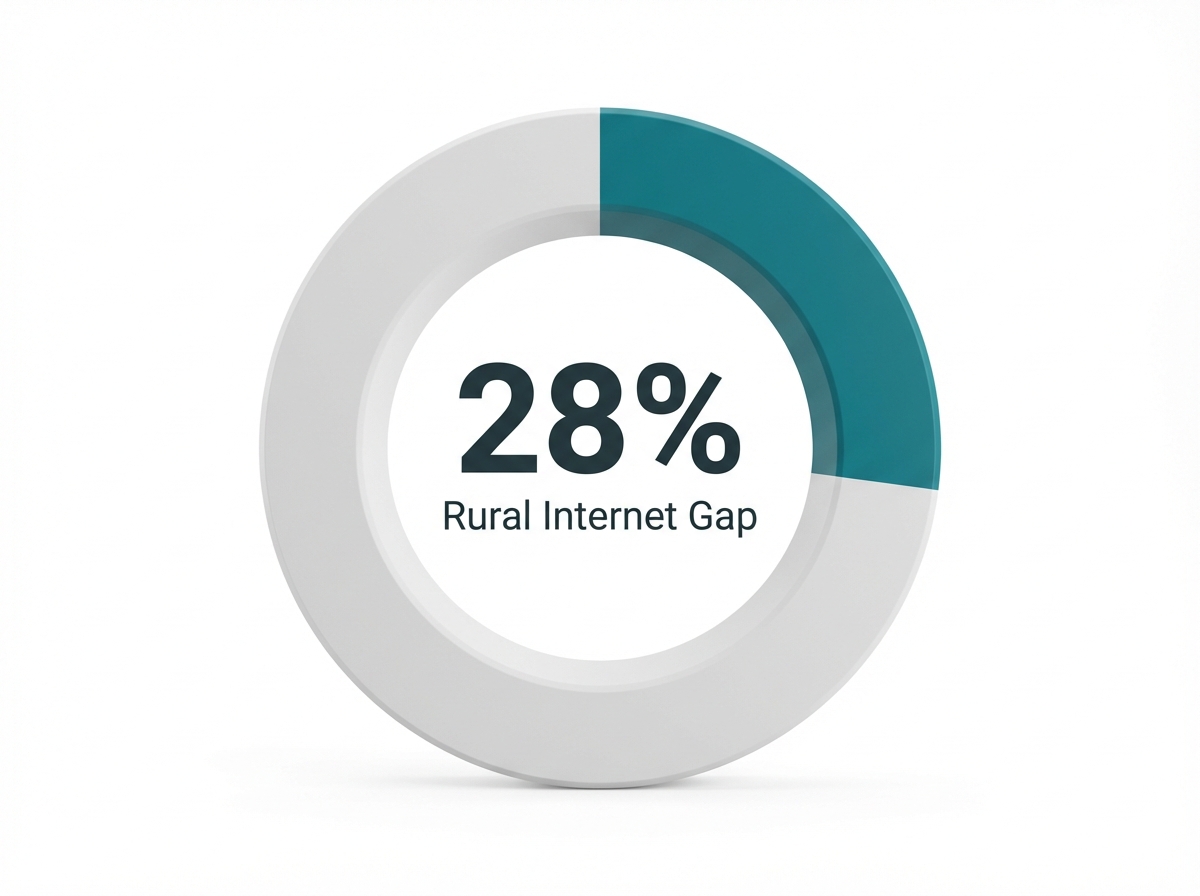
The biggest issue is the digital divide. Not everyone has a smartphone or good internet. For people who are homeless or struggling with money, buying a device can be impossible. If you can't get online, you can't get virtual care.
Tech skills are another barrier. Some older adults or people who aren't used to computers might find it hard to log in or download apps. This can be frustrating and might make them want to give up.
Privacy at home is also a concern. If you live in a crowded house, finding a quiet place to talk to a therapist can be tough. This lack of privacy might stop people from being open and honest during their sessions.
The gap between those who have internet and those who don't is real. About 28% of people in rural areas lack high-speed broadband.7 This means that where you live can determine if you can get help.
We need to work on getting better internet and devices to everyone so that telehealth can truly be for all.9
Internet access is now seen as a basic need for health, just like food or housing. Without it, you are cut off from modern healthcare. Bridging this gap is essential for fair health access.7, 9
Rural communities often face the hardest challenges. They have fewer doctors nearby and worse internet. Even on some Tribal lands, up to 24% of people have no broadband at all.7 Helping these communities get connected is a top priority for expanding telehealth.
Many of the rules that allow easy telehealth access are temporary. They were made during the pandemic and might expire in 2025. If they do, it could become harder to see a doctor from home.
In 2024, 25% of Medicare users relied on telehealth.6 Losing this access would be a big blow to many people who depend on it.
Experts call the potential end of these rules the "2025 telehealth policy cliff." If Congress doesn't act, insurance might stop covering home visits for many conditions. This would force people to go back to driving to clinics, which isn't always possible.6
Many groups are fighting to keep telehealth available. They want lawmakers to make the temporary rules permanent. This would ensure that everyone, regardless of where they live, can continue to get the care they need from home.6
Telehealth has truly changed the way we look at addiction recovery. It has opened doors for people who once felt locked out of the healthcare system. By removing barriers like distance and scheduling conflicts, virtual care makes it possible for more people to get the help they deserve.
This isn't just about convenience; it's about providing complete, high-quality care. From medication management to therapy for co-occurring mental health needs, telehealth offers a full range of services. It allows for personalized treatment plans that fit into your real life, all while keeping your information safe and secure.
For residents of Vermont, Massachusetts, Connecticut, and New Hampshire, help is closer than ever. Whether you live in a city or a quiet rural town, you can access top-tier specialists without leaving your home. The journey to recovery is personal, and having a flexible, supportive team just a click away can make all the difference.
Yes, many people can receive substance use disorder (SUD) treatment entirely through telehealth, provided they have the necessary technology and their specific treatment plan is suitable for virtual care. Telehealth services—such as video sessions and secure messaging—allow individuals to connect with counselors and support teams for co-occurring mental health needs from the privacy of their own homes. This approach expands access for those in Vermont, Massachusetts, Connecticut, and New Hampshire who may face travel or scheduling barriers.
Yes, research indicates that telehealth is just as effective as in-person treatment for addiction recovery. Studies comparing digital health options with traditional office visits found no significant difference in treatment retention or substance use outcomes. For medication adherence, virtual care can sometimes be even more effective than face-to-face approaches, offering a flexible way to stay engaged in recovery.4
Yes, in many cases, licensed providers can prescribe medication-assisted treatment (MAT) through telehealth. Platforms allow providers to assess needs and prescribe medications like buprenorphine or naltrexone during secure video visits. Policy changes have improved access to these prescriptions in New England states without requiring an initial in-person appointment.
Telehealth sessions are designed to be strictly private and confidential. Virtual care platforms must comply with HIPAA regulations, which act like a digital lock on your medical records. These laws ensure that secure video and encrypted messaging protect your personal health information, allowing only you and your approved care team to access it.10
To participate, you typically need a reliable internet connection and a device with a camera and microphone, such as a smartphone, tablet, or computer. Most platforms work through a web browser or a simple app. Having a quiet, private space is also essential for your appointments.
Yes, most major insurance plans, including Medicare and Medicaid, cover telehealth for substance use disorder and co-occurring mental health treatment. Coverage often includes video visits and medication management. However, it is always best to check with your specific insurer to confirm current benefits.6
Yes, you can attend sessions from work or while traveling, provided you have a private space and a good internet connection. However, you must be physically located in a state where your provider is licensed to practice (such as Vermont, Massachusetts, Connecticut, or New Hampshire) during the call.
Without reliable internet, video telehealth can be difficult. Some providers may offer audio-only phone options, or you might be able to find a private space with Wi-Fi, such as a community center or library private room. Improving broadband access remains a key goal for healthcare equity.7
Yes, audio-only phone calls are a form of telehealth and can be used for counseling or follow-up care when video isn't possible. While video is often preferred for building a connection, phone calls help bridge the gap for those with limited internet access.9
Yes, therapies like EMDR can be delivered effectively through telehealth using specialized digital platforms. You will need a stable internet connection and a private space to ensure safety and comfort during the process.
Yes, telehealth services for substance use disorder and co-occurring mental health support are widely available across Vermont, Massachusetts, Connecticut, and New Hampshire. This allows residents to connect with providers virtually, regardless of their specific location within these states.1
Telehealth offers a different environment that may help some individuals. Being in a familiar, comfortable setting can lower stress, and the flexibility of virtual care makes it easier to maintain consistent contact with your care team, which is crucial for long-term recovery.4
Yes, telehealth can be adapted for neurodivergent individuals. Features like flexible scheduling, the comfort of home, and the option for written communication can make care more accessible. Providers can tailor sessions to fit unique learning and communication styles.5
Telehealth makes it easier for family members to join therapy sessions or treatment planning meetings, even if they live in different locations. This increased involvement helps build a strong support system for the individual in recovery.5

November 7, 2025

December 29, 2025

June 16, 2025